All issues > Volume 53(5); 2010
A childhood case of spinal tuberculosis misdiagnosed as muscular dystrophy
- Corresponding Author: Yun-Kyung Kim, M.D. Department of Pediatrics, School of Medicine, Korea University, Ansan Hospital, 516, Gojan-dong, Ansan City, Gyeonggi-do 425-707, Korea. Tel: +82.31-412-6737, Fax: +82.31-405-8591, byelhana@korea.ac.kr
- Received September 14, 2009 Revised October 31, 2009 Accepted December 01, 2009
- Abstract
-
Tuberculosis is primarily a pulmonary disease, but extra-pulmonary manifestations are not uncommon, especially in children and adolescents. Ten percent of extra pulmonary tuberculosis localizes to the bones and joints, and 56% of such cases affect the spine. We treated a childhood case of spinal tuberculosis misdiagnosed as muscular dystrophy in a patient without specific constitutional symptoms. We report this case because the patient had an unusual presentation of spinal tuberculosis.
- Introduction
- Introduction
Tuberculosis (TB) remains a global public health threat. One third of the world's population are estimated to be infected with Mycobacterium(M.) tuberculosis, and 1.7 million people die from TB each year1). TB is often associated with poor socio-economic living conditions and is frequently found as a co-infection in people infected with the human immunodeficiency virus (HIV)1, 2).The incidence rates of TB are highest in developing countries, but the rates have been increasing in Western societies due to the HIV epidemic, immigration and the emergence of drug resistant strains1, 3). TB is primarily a pulmonary disease, but extra-pulmonary manifestations are not uncommon, especially in children and adolescents1). In these groups, ten percent of extra pulmonary TB localizes to the bones and joints (BJTB), and 56% of such cases affect the spine1, 4).In spinal TB, Mycobacterium is deposited via the end arterioles in the vertebral body adjacent to the anterior aspect of the vertebral end-plate. Thus the anterior portion of the vertebral body is most commonly involved5). Extension of the infection into the adjacent soft tissues to form paravertebral or epidural masses is commonly seen. The latter may result in neurological complications such as spinal cord compression6).The signs and symptoms of spinal TB include "night cries" and restless sleep, a low-grade daily fever, and a peculiar position (such as torticollis with cervical lesions) or gait. Findings on physical examination may include marked "guarding" because of dorsal muscle spasm, pain when the back is "pounded," a deformity (such as gibbus), or reflex changes (including clonus)6).In this case, we experienced a 3-year-old girl with spinal TB who was misdiagnosed as progressive muscular dystrophy. This patient showed no specific signs or symptoms of this infection. And, she showed significant neurological signs like muscle weakness and motor dysfunction of the lower extremities. She was evaluated and receiving care with the suspected diagnosis of a muscular dystrophy at several medical centers.But, she was finally diagnosed as longstanding TB spondylitis of the lower cervical and upper thoracic vertebrae with spinal cord compression by epidural abscess formation.
- Case report
- Case report
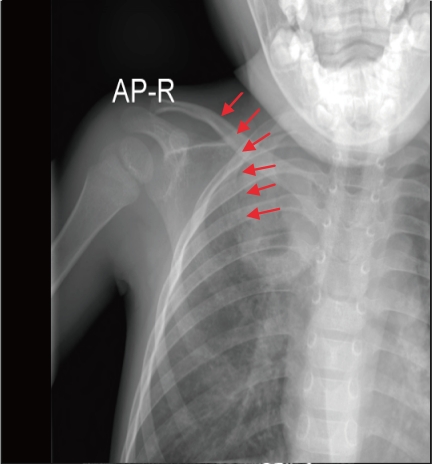
A 3-year-old girl was admitted to the department of pediatrics because of muscle weakness and motor dysfunction of the lower extremities; she had a limping gait and walked with an orthotic. The symptoms had first developed about 20 months previously and thereafter, slowly worsened. The patient was evaluated for muscle weakness of the lower extremities including a muscle biopsy and lumbar and thoracic magnetic resonance imaging (MRI) at several medical centers. The results of all evaluations were normal.Nevertheless, she continued to be seen regularly over the past years with the diagnosis of suspected progressive muscular dystrophy. Although she could not walk, she looked relatively well for about 20 months.On admission, it was noted that she had a cold for five days and had been febrile for three days. On physical examination, the vital signs were stable and the mental status intact. She was slightly underweight considering her age. Her head was tilted to the right side.There is no family history of TB, and the Mantoux test results of her family were all negative. She had been vaccinated with Bacillus Calmette-Guerin (BCG), by intradermal injection, at age of a month. And she had a BCG scar on her left upper arm.On physical examination, her neck was supple; Brudzinski and Kernig sign was negative. A few crackles and expiratory wheezes were heard in both lungs on chest auscultation.On neurological examination, the patient had an incomplete and limping gait. The grade for her lower extremity motor functions was decreased and was approximately 2-3. The deep tendon reflexes of the lower extremities were normal.The laboratory studies showed a white blood cell count of 17,620/mm3 and a platelet count of 664×103/mm3. The erythrocyte sedimentation rate was 9 mm/hr and the C-reactive protein was 0.25 mg/dL. The serum chemistry results were all normal. The Mantoux test result was positive, and measured 15 mm. However, the acid-fast bacillus stain and polymerase chain reaction for M. tuberculosis complex, of sputum, were all negative.Chest radiography showed a round opacity with internal cavitary changes in the posterior segment of the right upper lobe (RUL) of the lung suggestive of a congenital cystic mass in the RUL with a superimposed infection, such as pneumonia or tuberculosis (Fig. 1A, 1B).The chest computed tomography showed localized consolidation in the apical and posterior segment of the RUL. The cavitary changes in the RUL showed a smooth inner wall, suggesting a benign condition. In addition, destructive changes of the upper thoracic vertebral bodies with epidural extension were noted. The findings were suggestive of active pulmonary tuberculosis (TB) in the RUL and TB spondylitis involving the upper thoracic vertebrae with epidural extension (Fig. 2).The MRI of the thoracic spine showed abscess formation and total destruction of the C6 and C7 vertebral bodies. Severe cord compression at the same level and a suspected myelopathy was also seen. Partial destruction of the posterior half of C5 and T1 vertebral bodies were noted. Abscess formation without destruction of the T2 and T3 vertebral bodies were observed(Fig. 3). In summary, these findings suggested longstanding TB spondylitis and discitis with cord compression as well as pulmonary TB. And, there were no manifestations compatible with miliary TB or TB meningitis on all the related evaluations.We started treatment with a quadruple regimen of tuberculosis medications (Isoniazid, Rifampin, Pyrazinamide, and Streptomycin). But, the patient was referred to another hospital for surgical treatment, and at that hospital the diagnosis was pathologically confirmed on a surgical biopsy specimen. No tubercle bacilli were cultured from the specimen.After 18 months of tuberculosis treatment, the patient has completely recovered and has normal motor function of the lower extremities, and no neurological manifestations.
- Discussion
- Discussion
Spinal TB usually affects infants and young children1, 7). This is because of intense blood flow through growing bone in young children. Consequently, they suffer from BJTB more often than older children do.Bone infection can be initiated by two other mechanisms, particularly in the vertebrae: (1) direct extension through the lymphatics from a caseous paravertebral lymph node and (2) direct local hematogenous or lymphatic extension from a neighboring bone. As bone is destroyed progressively by pressure necrosis and formation of a cold abscess, a nearby joint may become involved6).The signs and symptoms of spinal TB include "night cries" and restless sleep, a low-grade daily fever, and a peculiar position (such as torticollis with cervical lesions) or gait.In the present case, the age of our patient at diagnosis was 37 months. Unlike the other typical cases, she had showed no systemic illness like fever, lethargy or irritability until the age, moreover, her neurological symptoms were so insidious that physicians who examined her could not take notice of the possibility of the disease.Cervical involvement of this disease is unusual, being affected in only 0.03% of all cases8, 9). Among the affected cases, the involvement of multiple vertebrae is not uncommon at the time of diagnosis. The average number of vertebrae involved is 2.6, and the most common level of involvement is C6 in cases of cervical tuberculosis8). In the present case, six vertebrae were involved, C5, 6, 7 and T1, 2, 3.On admission, our 3-year-old female patient had torticollis and muscle weakness of the lower extremities but had no constitutional symptoms suggestive of an infectious disease. The patient was evaluated and receiving care with the suspected diagnosis of muscular dystrophy. Accordingly, the correct diagnosis was delayed for about two years.Therefore, in cases with neurological manifestations from a spinal origin, one should consider TB in the differential diagnosis, especially in a patient from a region with endemic TB1). The differential diagnosis must include low-grade infections caused by Staphylococcus, Haemophilus influenzae, Salmonella, and Brucella ; fungal infections; rheumatoid arthritis; malignant disease of bone; eosinophilic granuloma, particularly with skull or pelvic lesions; and osteochondrosis resulting from aseptic necrosis of bone, particularly Legg-Calvé-Perthes disease and tuberculosis of the hip6).In the present case, an early diagnosis was complicated by both patient delay, due to the minimal complaints before vertebral necrosis caused spinal compression and neurological impairment, and diagnostic delay by physicians who misdiagnosed the disease as muscular dystrophy because of the absence of typical constitutional symptoms and the relatively low incidence of these kinds of complicated manifestations of TB.TB is a re-emerging infectious disease. Parallel, extra-pulmonary manifestations are diagnosed more often. An increasing incidence of BJTB is being reported worldwide and attributable to HIV epidemic, immigration and so on1). The number of newly diagnosed extra-pulmonary TB patients was 5,171 in Korea. The age distribution curve showed a peak in the young generation, which implies that TB is still prevalent in Korea11).Therefore, pediatricians must maintain a high index of suspicion for this insidious disease when evaluating children with neurological manifestations10), especially motor dysfunction of the lower extremities such as gait disturbances, in spite of the absence of relevant constitutional symptoms.
- References
- 1. van Well GT, van der Mark LB, Vermeulen RJ, van Royen BJ, Wuisman PI, van Furth AM. Spinal tuberculosis in a 14-year-old immigrant in the Netherlands. Eur J Pediatr 2007;166:1071–1073.2. Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, et al. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med 2003;163:1009–1021.
[Article]3. Faustini A, Hall AJ, Perucci CA. Risk factors for multidrug resistant tuberculosis in Europe: a systematic review. Thorax 2006;61:158–163.
[Article]4. Jutte PC, van Loenhout-Rooyackers JH, Borgdorff MW, van Horn JR. Increase of bone and joint tuberculosis in The Netherlands. J Bone Joint Surg Br 2004;86:901–904.5. Teo HE, Peh WC. Skeletal tuberculosis in children. Pediatr Radiol 2004;34:853–860.6. Starke JR. In: Feigin RD,Tuberculosis. editor. Feigin & Cherry's textbook of pediatric infectious diseases. 20096th ed. Philadelphia: Saunders/Elsevier Co, :1442–1443.
[PubMed]7. Watts HG, Lifeso RM. Tuberculosis of bones and joints. J Bone Joint Surg Am 1996;78:288–298.8. Dogulu F, Baykaner MK, Onk A, Celik B, Ceviker N. Cervical tuberculosis in early childhood. Childs Nerv Syst 2003;19:192–194.9. Wurtz R, Quader Z, Simon D, Langer B. Cervical tuberculous vertebral osteomyelitis: case report and discussion of the literature. Clin Infect Dis 1993;16:806–808.10. Osguthorpe RJ, Parker S, Nyquist AC. Case report: two-year-old boy with a limp. Curr Opin Pediatr 2001;13:598–602.11. Kim HJ. Current situation of tuberculosis and its control in Korea. J Korean Med Assoc 2006;49:762–772.
Fig. 1
Chest radiography shows a round opacity with internal cavitary changes in the posterior segment of right upper lobe (RUL) of the lung.

Fig. 2
On the chest computed tomography (CT), localized consolidation was noted in the apical and posterior segments of the RUL of the lung. Cavitary changes in the RUL had a smooth inner wall, suggesting a benign condition. Destructive changes of the upper thoracic vertebral bodies and epidural extension were noted. Calcified nodes were observed in the lower paratracheal and left hilar areas.
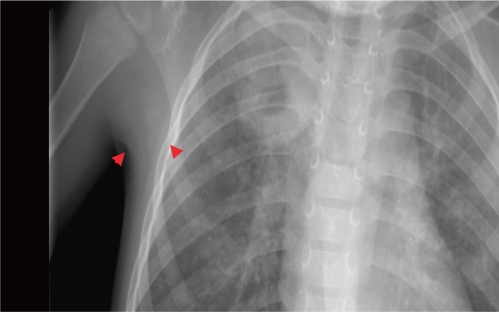
Fig. 3
On the magnetic resonance imaging (MRI) of the thoracic spine, abscess formation and total destruction of C6 and C7 vertebral bodies were seen. Severe cord compression at the same level with a suspicious myelopathy was also seen. Partial destruction of the posterior half of the C5 and T1 vertebral bodies were noted. Abscess formation without destruction of the T2 and T3 vertebral bodies were observed. Combined discitis of the intervertebral discs between T1, T2 and T2, T3 were seen. Subligamentous spread of abscesses from C5 to T5 in the anterior aspect and C4 to T1 in the posterior aspect were noted. Mediastinal extension of subligamentous abscesses were seen, especially on the right side.

 About
About Browse articles
Browse articles For contributors
For contributors
