All issues > Volume 53(7); 2010
Clinical outcome of acute myocarditis in children according to treatment modalities
- Corresponding author: Hong Ryang Kil, M.D. Department of Pediatrics, Chungnam National University School of Medicine, 640, Daesa-dong, Jung-gu, Daejeon 301-721, Korea. Tel: +82.42-280-7251, Fax: +82.42-255-3158, gilhong@cnu.ac.kr
- Received November 16, 2009 Revised February 17, 2010 Accepted March 17, 2010
- Abstract
-
- Purpose
- Purpose
- There is currently little evidence to support intravenous immune globulin (IVIG) therapy for pediatric myocarditis. The purpose of our retrospective study was to assess the effects of IVIG therapy in patients with presumed myocarditis on survival and recovery of ventricular function and to determine the factors associated with its poor outcome.
- Methods
- Methods
- We reviewed all consecutive cases of patients with myocarditis with left ventricular dysfunction verified by echocardiogram who had visited 3 university hospitals between January 2000 and September 2009. These patients were divided into 2 groups. Group 1 consisted of 23 patients (69.6%) who received IVIG alone or IVIG in combination with steroids, and group 2 consisted of 10 patients (30.3%) who received neither IVIG nor other immunosuppressive agents. Clinical manifestations, laboratory results, echocardiographic findings, and outcomes were compared between these 2 groups.
- Results
- Results
- One year after the initial presentation, the difference in the probability of survival did not show statistical significance in IVIG-treated patients (P=0.607). Of the echocardiographic parameters on admission, a shortening fraction of less than 15% was associated with unremitting cardiac failure. Furthermore, anemic patients were more likely to have elevated N-terminal fragment levels of the B-type natriuretic peptide (NT-proBNP) in the progressed group (P=0.036).
- Conclusion
- Conclusion
- There was no difference between the IVIG-treated patients and the control patients in the degree of recovery of left ventricular function and survival. Prospective, randomized, clinical studies are needed to elucidate the effects of IVIG treatment during the acute stage of myocarditis on ultimate outcomes.
- Introdction
- Introdction
The clinical presentations of myocarditis range from nonspecific systemic symptoms associated with viral prodrome to fulminant hemodynamic collapse and sudden death. The extreme diversity of clinical manifestations has made the true incidence of myocarditis difficult to determine. Recent prospective postmortem data have implicated myocarditis in the sudden death of young adults at rates of 8.6% to 12%1, 2).Our current understanding of the pathogenesis of myocarditis derives largely from animal modes. Direct myocardial invasion by cardiotropic virus rapidly progress to the second phase of immunologic activation. The use of immunosuppression during acute viral myocarditis remains controversial3, 4). Lernel5-7) suggested that steroids be avoided at least during the first 10 days of acute infection because steroids inhibit interferon synthesis and increase viral multiplication in experimental coxsackievirus infection. In contrast, in experimental coxsackievirus-induced myocarditis, virus titers in the heart of polyclonal mouse immune globuline (Ig) treated animals were significantly reduced on 7 days after infection8).However, a few Korean reports have been published on pediatric myocarditis regarding the effectiveness of intravenous immune globulin (IVIG) treatment. Therefore, we have described the clinical outcomes of pediatric patients with myocarditis and compared the final outcomes, and the time to recovery of normal left ventricular systolic function in those children treated with IVIG, compared with those treated neither with IVIG nor other immunosuppressive agents. Furthermore, we determined the factors associated with its poor outcome.
- Materials and methods
- Materials and methods
- 1. Patients
- 1. Patients
We retrospectively analyzed the medical records of 33 myocarditis patients who were admitted to the pediatric departments of Eulji University School of Medicine, Daejeon, Soonchunhyang University School of Medicine, Cheonan and Chungnam University School of Medicine, Daejeon.The diagnosis of acute viral myocarditis was defined as the clinical evidence of acute myocardial dysfunction by physical exam, chest X-ray, electrocardiogram (ECG) and echocardiogram associated with an elevation of cardiac enzymes such as MB isoform of creatine kinase (CK-MB), cardiac troponin T, troponin I and N-terminal fragment of B-type natriuretic peptide (NT-proBNP). We excluded patients with a history of chronic renal failure and evidence of long-standing dilated cardiomyopathy by history or physical examination; those with documentation of conditions known to be associated with acute congestive heart failure such as sepsis, Kawasaki disease and those who received previous treatment with a known cardiotoxic agent.- 2. Methods
- 2. Methods
Cardiomegaly on chest X-ray was defined when the cardiothoracic (CT) ratio >50% in children more than 1 year old and CT ratio >60% in infants younger than 12 months of age. Abnormalities on ECG that were recorded were arrhythmia, low voltage QRS, ST segment and T wave changes. Measurements of left ventricular dimension and function were derived from two-dimensional images in the parasternal long-axis view. The echocardiographic examination was used to evaluate the valve regurgitation, quantitative cardiac contractile function, as well as the presence of pericardial fluid. Left ventricular end-diastolic (LVED) dimension, left ventricular end-systolic (LVES) dimension were measured and calculated to the body surface area. Normal dimensions were defined as within two standard deviation (SD)s of the mean9). Normal fractional shortening was 28-35%.In all cases of suspected myocarditis, bacterial cultures from the blood, urine or throat were performed and the antibody titer of cardiotropic virus was measured in serums from the 12 patients. The cases were considered to have tested positive for the virus when the antibody titer increased to more than quadruple. Reverse transcriptase-polymerase chain reaction (PCR) was used to evaluate RSV, influenza A, influenza B, adenovirus, HSV and EBV through tracheal aspirates from 9 patients with respiratory symptoms. In one patient, a right ventricular endomyocardial biopsy was performed.Several factors were compared between group 1 and group 2, such as gender, clinical manifestation, days of ICU admission and intubation care the laboratory findings, ECG and echocardiogram on admission. We also compared the progressed group (including mortality and dilated cardiomyopathy) with the recovery group according to the long-term follow up results.- 3. Statistical analysis
- 3. Statistical analysis
All the results were expressed as mean value±SD, except when stated otherwise. Between the groups, analysis of categorical variables was performed with the two-tailed Fisher's exact test. Student's t-test used to analyze the continuous variables. Survival curves were generated according to the Kaplan-Meir method and were compared using the log-rank statistics. Multivariate analysis was performed using the Cox proportional-hazards model for censored data.
- Results
- Results
- 1. Baseline patient characteristics
- 1. Baseline patient characteristics
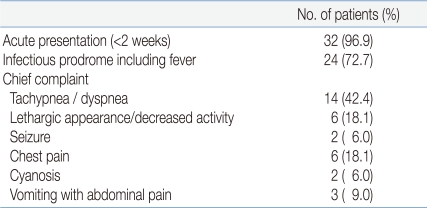
The myocarditis group included 18 males and 15 females with a median age at diagnosis of 47.5 months with a range from 8 days to 19 years. The mean age on admission was 41 months in group 1 and 60 months in group 2. The mean follow up duration was 13.5 months and 13.1 months respectively.The most common chief complaints were tachycarida and respiratory difficulty in 14 patients (42.4%). Poor appetite, lethargy and chest pains were the next chief complaints. Newborns or infants presented with respiratory distress, cyanosis and heart failure. Older patients were initially seen with sudden onset of arrhythmia and chest pain. Recent upper respiratory tract infection was associated with in 72% of the patients and 45% of the patients showed high temperature on admission (Table 1).- 2. Chest radiograph, ECG and echocardiogram
- 2. Chest radiograph, ECG and echocardiogram
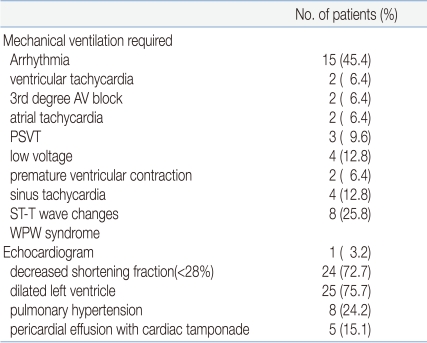
The cardiomegaly was seen in 87% of the patients and there was no difference between the two groups. ECG was performed in 31 patients. Major abnormal ECG were low voltage QRS (12.9%), sinus tachycardia (12.9%) and complete heart block (6.4%). The two patients with third-degree AV block were in group 1 and one case transformed to ventricular tachycardia requiring DC cardioversion. This ECG finding changed to first degree AV block on hospital day 4 and the other patient completely recovered from the third-degree AV block. Atrial tachycardia (6.4%) and ventricular tachycardia (6.4%) was present in group 1. There was no difference between the two groups.An echocardiography was performed upon admission on all patients. At presentation, 24 (72.7%) of the patients had depressed left ventricular contractility. The mean FS on admission was 19±11.3% in group 1 and 20±12.2% in group 2 (P=0.893).The mitral valve was the most frequently affected valve and the tricuspid valve was next. There was no difference between the two groups in the presence of moderate valve insufficiency. Pericardial effusion was present in 39% of the patients and 5 cases necessitated pericardiocentesis due to cardiac tamponade (Table 2).- 3. Laboratory findings
- 3. Laboratory findings
CK-MB was checked in 77% of the patients. The mean CK-MB level was 139.7 ng/dL in group 1 and 96 ng/dL in group 2. There was no difference between two groups (P=0.751). Troponin I was measured in 13 cases and was elevated in 38.4% of the patients. The mean cardiac troponin I (cTnI) was 14.7 ng/dL in group 1 and 2.5 ng/dL in group 2. cTnI was more elevated in IVIG-treated group although there was no statistical significance (P=0.207). Troponin T was checked in 25 cases and was elevated in 60% of the patients. The mean cardiac troponin T (cTnT) level was 1.19 mg/dL in group 1 and 0.69 mg/dL in group 2. There was no difference between two groups (P=0.525).We measured NT-proBNP in 23 cases and the concentrations of NT-proBNP was elevated in 95.6% of patients. The mean concentration of NT-proBNP was 16,126 pg/mL in group 1 and 4,263 pg/mL in group 2 (P=0.019). C-reactive protein (CRP) was significantly elevated in group 1 (P=0.015), and the mean concentration of CRP was 11.1 mg/dL in group 1 and 0.6 mg/dL in group 2.The presence of anemia in conjunction with myocarditis occurred 57.9% of the patients. The proportion of patients with anemia was significantly higher in IVIG-treated patients (P=0.004). Packed red blood cell transfusion was required in 7 cases in group 1 and none in group 2 (Table 3).- 4. Diagnostic evaluation
- 4. Diagnostic evaluation
Among the 33 patients suspected myocarditis, none of the cases showed positive results by bacterial culture of blood, urine, sputum or throat. Fourteen out of 21 cases (66.6%) were positive in viral study in serum, stool, pericardial fluid and tracheal aspirate. An increase in type-specific neutralizing antibodies was found in 5 cases in coxsackie B3, 4 and 5 viruses. Coxsackie A virus (type 2, 5 and 16) was identified in serologic techniques in 3 cases. For the rest, positive mumps IgM (1 case), positive adenovirus IgM (1 case), and high antibody titer of echovirus type 7 (2 cases) were identified by serologic technique. Respiratory syncytial virus (5 cases), influenza A (1 case), influenza B (1 case), and metapneumovirus (1 case) were detected by multiplex RT-PCR in tracheal aspirates (Table 4). Endomyocardial biopsy was performed in 1 DCM patient under fluoroscopic guidance by percutaneous puncture of the right jugular vein; four specimens were obtained from the right ventricular septum. Histology of biopsy revealed focal loss of myofibril and infiltration of myofibril in the interstitium.- 5. Treatment of myocarditis
- 5. Treatment of myocarditis
Of the 33 children with acute myocarditis, 23 (69.6%) patients were treated with high-dose IVIG and 10 (30.3%) were control patients who did not receive IVIG therapy.Seventeen patients received treatment with IVIG (2 g/kg/day) and 6 patients received IVIG and steroids (methylpredisolone, 2 mg/kg/day). In the latter cases, steroids were used for the treatment of associated bronchiolitis. Therefore, we added steroids with a low dose after the fever subsided. Positive inotropic agents, such as dopamine or dobutamine, were used in 19 cases (82.6%) in the IVIG-treated groups. Patients receiving IVIG therapy were more likely to have received inotropic agents. However, the result did not achieve statistical experience (P=0.20). Children in the two groups did not differ significantly in sex distribution, age at presentation, the use of angiotensin converting enzyme (ACE) inhibitor, or the need for ventilator care (Table 3).- 6. Prediction of 1-year survival
- 6. Prediction of 1-year survival
Among the 23 children in the IVIG-treatment group, 3 patients died. 17 month-old girl supported on extracorporeal membrane oxygenation (ECMO) on hospital day 4 expired due to multiorgan failure on hospital day 12. The rest two patients presented as fulminant myocarditis expired on hospital day 2. Two patients progressed DCM required prolonged antiarrhythmic agent for a persistent ventricular arrhythmia, associated with poor ventricular function.Among the 10 patients in the non-IVIG group, 2 patients expired due to ventricular tachycardia on hospital day 1 and 7 respectively. One patient progressed to DCM and was transplanted at another hospital.The overall survival rate was 81.8%. There was no difference in survival at 1 year after presentation between the IVIG-treated group and the control group (P=0.607). The recovery of myocardits was defined as normal ventricular function by echocardiography and the normal values of cardiac enzymes. The mean time to recovery of function was 68 days in group 1 and 33 days in group 2. There was no significant difference between the groups (P=0.485).- 7. Risk factors for adverse outcome
- 7. Risk factors for adverse outcome
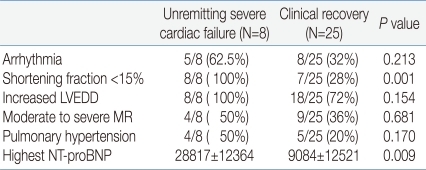
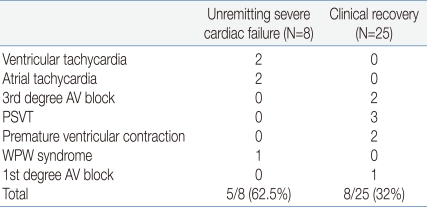
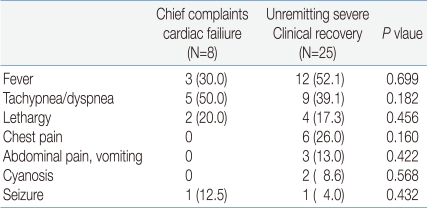
Patients were divided in two groups with based on outcomes. One of the groups was the recovery group and the other was the progressed group. The number of non-survivors was 5 from a total 33 of patients (15.1%). Three cases progressed to DCM (9.0%). We compared the progressed group (including mortality and dilated cardiomyopathy; 8 patients) with the recovery group (25 patients) to assess poor prognostic factor (Table 5).The mean shortening fraction on admission of the patients who developed unremitting cardiac failure was 9.7±3.0%, compared to 23.1±11.2% of those who later recovered cardiac function (P=0.003). The mean concentration of NT-proBNP was 28,817±12,364 pg/mL in unremitting severe cardiac failure, compared to 9,084±12,521 pg/mL in the clinical recovery group (P=0.009). Other variables examined for possible association with outcomes were CRP, hemoglobin, troponin T, and troponin I. None of these were significantly associated with outcomes. The treatment with inotropic agents or ACE inhibitors did not affect the mortality rate.The abnormal ECG findings of the progressed group were found in 62.5% of the patients compared to 32% in the recovery group. However, there was no statistical significance between the two groups (Table 6).
- Discussion
- Discussion
Myocarditis is a process characterized by inflammatory infiltrate of the myocardium with the necrosis and/or degeneration of adjacent myocytes associated with autoimmunity. The true incidence of myocarditis is not known because of the variable clinical manifestations, laboratory findings and etiologies. Viral exposure leads to an acute or subacute immune response that is responsible for most of the inflammation, infiltration, and myocardial damage that ensues. However, if host immune activation continues unabated despite elimination of the virus, autoimmune disease may result. Some remodeling mechanisms leading to dilated cardiomyopathy may be specific to myocarditis. Genetic susceptibility of host was also associated with that immune response10).Presentation depends on the age of the child. Newborns or infants present with fever, poor appetite, respiratory distress and periodic episodes of pallor. Older children and adolescents report chest pain, palpitations or sudden-onset arrhythmia. We analyzed the clinical findings of the recovery and the progressed groups and compared the two groups. Tacypnea and dyspnea were more common in the progressed group, although there was not a significant difference (Table 7).Amsel et al11) described a 3-month old infant who developed myocarditis several hours after diphtheria, pertussis, and tetanus (DPT) vaccination. The time of occurrence of symptoms, the clinical course, and the negative virological studies suggested a possible cardiogenic adverse reaction to the vaccine. In our study, a 2-month old girl presented with irritability and decreased oral intake 1 day after DPT vaccination. However, there was limitation to confirm the vaccination-induced mypocarditis because the etiologic agent was not identified in our study.Fulminant myocarditis was diagnosed on the basis of clinical features at presentation, including the presence of severe hemodynamic compromise, rapid onset of symptoms, and fever. In our study, 4 patients met the criteria for fulminant myocarditis. One patient completely recovered ventricular function and the other 3 patients died. Despite the fact that the time from onset of the symptoms to hospital admission was one or two days, the patients with fulminant myocarditis were critically ill at presentation. Three patients with fulminant myocarditis suddenly expired between 12 and 24 hours of their hospital visit. Two of these patients had evidence of atrial tachycardia on ECG.Most cases of myocarditis result from viral infections. The most common viral causes include adenovirus and enterovirus (coxsackievirus A and B, echovirus). Although infections are often asymptomatic, approximately 5% to 10% of pediatric respiratory infections are due to adenovirus infections, with outbreaks facilitated in environments where young people remain in close proximity12).Tracheal aspirate PCR may provide a safer means of arriving at an etiologic diagnosis in viral myocarditis than endomyocardial biopsy, especially when the right ventricular free wall and outflow tracts are pathologically thinned13). All cases of myocarditis in which biopsies were performed had PCR results of heart specimens identical to the results of tracheal aspirate screening.Considerable data is available to demonstrate that enteroviruses can be detected within the myocardium of patients with acute onset of myocarditis and in mice infected with coxsackievirus. Virus infection has also been associated with direct myocytopathic effects14-16). Altogether, the evidence suggests that both the direct effects of myocardial infection and the activation of the immune process are likely to have significant roles in the development of myocarditis.ECG findings in patients with acute myocardits are highly variable. The most typical findings are: 1) sinus tachycardia; 2) low voltage QRS in standard and precordial leads; and 3) flattened or inverted T waves. Friedman and colleagues reported significant residual ventricular arrhythmias requiring medication in 42% of their patients at a mean follow up period of 51 months, and histologic resolution did not correlate with resolution of arrhythmia17). Whether chronicity of the arrhythmia is due to fibrosis and scarring as a residual effect of the initial insult or is due to undetected persistent inflammation is speculative. In our study, 2 of 31 (6.4%) patients developed complete heart block. At follow-up, both of them showed normal ECG on Holter monitoring. One patient with persistent ectopic atrial tachycarida was on medication (sotalol, propranolol).In patients with clinically suspected myocarditis, laboratory variables conventionally used to detect myocardial cell damage, such as CK or CK-MB levels, are often within the normal range, partly because they are present in normal serum and a small amount of myocardial necrosis does not lead to increases that exceed the normal range. Recently, cardiac troponin T (cTnT), unique to cardiac tissue is used to screen myocarditis. When elevated cTnT levels were detected in patients with clinically suspected myocarditis, immunohistologic analysis of the endomyocardial biopsy specimens showed evidence of myocarditis in 93%18). In our study, elevated cTnT was observed in 15 of 25 (60%) of the patients.Echocardiography is currently recommended in the initial diagnostic evaluation of all patients with suspected myocarditis. However, the most common echocardiographic features of acute myocarditis are quite nonspecific. Segmental wall motion abnormalities were observed in 64% of patients and included hypokinetic, akinetic, or dyskinetic regions19). James et al20) reported that lymphocytic myocarditis was associated with LV diastolic dysfunction of a predominantly restrictive pattern. Myocarditis and fibrosis induced changes in echocardiographic image texture, i.e. increases in brightness, heterogeneity, and contrast21). Typically, patients with fulminant myocarditis presented with nondilated, thickened and hypocontractile LVs, whereas those with acute myocarditis had marked LV dilation, normal LV thickness and decreased LV function22).In our study, 8 patients met the criteria for pulmonary hypertension by echocardiography. Of those, 2 patients expired, one patient progressed to DCM, and the rest of patients recovered ventricular function at the time of discharge. Cappola et al23) reported that the mean pulmonary artery is particularly important for stratifying risk in myocarditis. Our study did not show the pulmonary hypertension as the poor prognostic factor(P=0.17). However, these results should not be generalized due to the small samples in our study.Because there is a risk associated with biopsy, particularly in young children or those with severe ventricular dilatation, many centers tried to find etiology of acute myocarditis in another way. Viral culture of peripheral specimens, such as blood, stool, or urine is commonly performed but is unreliable at identifying the causative infection. A fourfold increase in antibody titer correlates with infection.The clinical utility of endomyocardial biopsy for evaluating patients with possible myocarditis has been debated24). Nevertheless, endomyocardial biopsy continues to be selectively used in many centers for the evaluation of possible myocarditis. Cardiovascular magnetic resonance (CMR) may be a valuable tool to noninvasively identify and assess the extent of myocardial involvement before endomyocardial biopsy is performed. PCR amplified viral genome in 239 of 624 (38%) samples obtained from patients with myocarditis in the previous study25). Pankuweit et al26) confirmed the prevalence of parvovirus B19 genome in endomyocardial biopsy to be highest in patients with myocarditis (19%).The diagnostic complexity created by the multifaceted pathophysiology of continued viral presence might best be deciphered by cDNA microarray analysis of the message from endomyocardial biopsy tissue in the near future.In this study, the lower hemoglobin level, the higher the NT-proBNP level in the progressed group. Levels of BNP are used to facilitate the diagnosis of heart failure and to determine the prognosis in patients with heart failure and myocardial infarction in adults27-29). Recently, the use of NT-proBNP was extended to pediatric inflammatory heart disease or congenital heart disease. However, the association between anemia and high NT-proBNP in acute myocardits is unknown. Rall et al30) reported that anemia is associated with elevated BNP and increased mortality in heart failure. A reduced hematocrit can result not only from a reduced red blood cell volume but also from an increased plasma volume. Volume overload that occurs with hemodilution could also contribute to the worse outcomes31).Previous studies attempted to describe the clinical course of acute myocarditis in pediatric patients. Predictive factors on admission for poor outcome were ejection fraction <30%, increased left ventricular end-diastolic dimension and moderate to severe mitral regurgitation32). In our study, NT-proBNP concentrations and left ventricular fractional shortening were valuable prognostic factors. The existence of moderate mitral regurgitation or pulmonary hypertension did not affect the mortality in this study.Understanding the pathogenesis of myocarditis provided the question of whether there is sufficient scientific evidence to support or discourage the use of IVIG or steroids. According to a recent study in Korea, steroids and IVIG were ineffective treatments in acute myocarditis33). In the study by Drucker et al34), 21 children presenting with presumed acute viral myocarditis were treated with an IVIG (2 g/kg/day). These findings resulted in a higher probability of left ventricular recovery for the immune globulin-treated patients. Kim et al35) reported two children with fulminant myocarditis successfully treated with a 10-h infusion of high dose IVIG. The mechanism by which IVIG may improve myocardial dysfunction in myocarditis is unknown. IVIG could be effective by providing specific antibodies to viruses and thus could lead to a more rapid clearing of myocardial viral infection.Despite the potential therapeutic efficacy suggested by previous uncontrolled studies, treatment of adult patients with recent-onset cardiomyopathy with immune globulin in placebo-controlled trial did not affect improvements in LVEF or functional capacity during follow-up36). In this study, there was no difference between the immune globulin-treated patients and the control patients in the degree of recovery and survival. The efficacy of immunosuppressive therapy for acute myocarditis in children requires investigation with a prospective, randomized, and controlled study. Further studies should identify the clinical predictor or genetic basis of myocarditis progressing DCM.
- Notes
The content of this paper was presented in 59th Annual Autumn Meetings of the Korean Pediatric Society in Seoul, Korea, October 23-24, 2009.
- References
- 1. Theleman KP, Kuiper JJ, Roberts WC. Acute myocarditis (predominately lymphocytic) causing sudden death without heart failure. Am J Cardiol 2001;88:1078–1083.
[Article] [PubMed]2. Doolan A, Langlois N, Semsarian C. Causes of sudden cardiac death in young Australians. Med J Aust 2004;180:110–112.
[Article] [PubMed]3. O'Connell JB, Robinson JA, Henkin RE, Gunnar RM. Immunosuppressive therapy in patients with congestive cardiomyopathy and myocardial uptake of gallium-67. Circulation 1981;64:780–786.
[Article] [PubMed]4. Anderson JL, Fowles RE, Unverferth DV, Mason JW. Immunosuppressive therapy of myocardial inflammatory disease: initial experience and future trials to define indication for therapy. Eur Heart J 1987;8:263–266.
[PubMed]5. Hirschman SZ, Hammer GS. Coxsackie virus myopericarditis: a microbiological and clinical review. Am J Cardiol 1974;34:224–232.
[Article] [PubMed]8. Weller AH, Hall M, Huber SA. Polyclonal immunoglobuliin therapy protects against cardiac damage in experimental coxsackievirus-induced myocarditis. Eur Heart J 1992;13:115–119.
[Article] [PubMed]9. Kampmann C, Wiethoff CM, Wenzel A, Stolz G, Betancor M, Wippermann CF, et al. Normal values of M mode echocardiographic measurements of more than 2000 healthy infants and children in central Europe. Heart 2000;83:667–672.
[Article] [PubMed] [PMC]10. Liu PP, Mason JW. Advances in the understanding of myocarditis. Circulation 2001;104:1076–1082.
[Article] [PubMed]11. Amsel SG, Hanukoglu A, Fried D, Wolyvovics M. Myocarditis after triple immunisation. Arch Dis Child 1986;61:403–405.
[Article] [PubMed] [PMC]12. Friedman RA, Duff DF, Schowengerdt KO Jr, Vallejo JG, Towbin JA. In: Feigin RD, Cherry JD, Demmler GJ, Kaplan SL,Myocarditis. editors. Textbook of pediatric infectious disease. 20045th ed. Philadelphia: Saunders, :390–413.13. Akhtar N, Ni J, Stromberg D, Rosenthal GL, Bowles NE, Towbin JA. Tracheal aspirate as a substate for polymerase chain reaction detection of viral genome in childhood pneumonia and myocarditis. Circulation 1999;99:2011–2018.
[Article] [PubMed]14. Knowlton KU, Lim B-K. Viral myocarditis: is infection of the heart required? J Am Coll Cardiol 2009;53:1227–1228.
[Article] [PubMed]15. Caforio AL, Goldman JH, Haven AJ, Baig KM, Libera LD, McKenna WJ. Circulating cardiac-specific autoantibodies as markers of autoimmunity in clinical and biopsy-proven myocarditis. The Myocarditis Treatment Trial Investigators. Eur Heart J 1997;18:270–275.
[Article] [PubMed]16. Seong IW, Choe SC, Jeon ES. Fulminant coxsackieviral myocarditis. N Engl J Med 2001;345:379
[Article] [PubMed]17. Friedman RA, Kearney DL, Moak JP, Fenrich FAL, Perry JC. Persistence of ventricular arrhythmia after resolution of occult myocarditis in children and young adults. J Am Coll Cardiol 1994;24:780–783.
[Article] [PubMed]18. Lauer B, Niederau C, Kuhl U, Schannwell M, Pauschinger M, Strauer B, et al. Cardiac troponin T in patients with clinically suspected myocarditis. J Am Coll Cardiol 1997;30:1354–1359.
[Article] [PubMed]19. Pinamonti B, Alberti E, Cigalotto A, Dreas L, Salvi A, Silvestri F, et al. Echocardiographic findings in myocarditis. Am J Cardiol 1988;62:285–291.
[Article] [PubMed]20. James KB, Lee K, Thomas JD, Hobbs RE, Rincon G, Bott-Silverman C, et al. Left ventricular diastolic dysfunction in lymphocytic myocarditis as assessed by Doppler echocardiography. Am J Cardiol 1994;73:282–285.
[Article] [PubMed]21. Lieback E, Hardouin I, Meyer R, Bellach J, Hetzer R. Clinical value of echocardiographic tissue characterization in the diagnosis of myocarditis. Eur Heart J 1996;17:135–142.
[Article] [PubMed]22. Felker GM, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Baughman KL, et al. Echocardiographic findings in fulminant and acute myocarditis. J Am Coll Cardiol 2000;36:227–232.
[Article] [PubMed]23. Cappola TP, Felker GM, Kao WHL, Hare JM, Baughman KL, Kasper EK. Pulmonary hypertension and risk of death in cardiomyopathy: patients with myocarditis are at higher risk. Circulation 2002;105:1663–1668.
[Article] [PubMed]24. Shanes JG, Gahli J, Billingham ME, Ferrans VJ, Fenoglio JJ, Edwards WD, et al. Interobserver variability in the pathologic interpretation of endomyocardial biopsy results. Circulation 1987;75:401–405.
[Article] [PubMed]25. Bowles NE, Ni J, Kearney DL, Pauschinger M, Schultheiss HP, McCarthy R, et al. Detection of viruses in myocardial tissues by polymerase chain reaction: evidence of adenovirus as a common cause of myocarditis in children and adults. J Am Coll Cardiol 2003;42:466–472.
[Article] [PubMed]26. Pankuweit S, Lamparter S, Schoppet M, Maisch B. Parvovirus B19 genome in endomyocardial biopsy specimens. Circulation 2004;109:e179
[Article] [PubMed]27. Cowie MR, Mendez GF. BNP and congestive heart failure. Curr Probl Cardiol 2003;28:264–311.
[Article]28. Cowie M, Journain P, Maisel A, Dahlstrom U, Follath F, Isnard R, et al. Clinical applications of B-type natriuretic peptide (BNP) testing. Eur Heart J 2003;24:1710–1718.
[Article] [PubMed]29. Mukoyama M, Nakao K, Saito Y, Ogawa Y, Hosoda K, Suga S, et al. Increased human brain natriuretic peptide in congestive heart failure. N Engl J Med 1990;323:757–758.
[Article] [PubMed]30. Ralli S, Horwich TB, Fonarow GC. Relationship between anemia, cardiac troponin I, and B-type natriuretic peptide levels and mortality in patients with advanced heart failure. Am Heart J 2005;150:1220–1227.
[Article] [PubMed]31. Androne AS, Katz SD, Lund L, LaManca J, Hudaihed A, Hryniewicz K, et al. Hemodilution is common in patients with advanced heart failure. Circulation 2003;107:226–229.
[Article] [PubMed]32. Kuhn B, Shaporo ED, Walls TA, Friedman AH. Predictors of outcome of myocarditis. Pediatr Cardiol 2004;25:379–384.
[PubMed]33. Kwon BS, Lee CH, Choi EY, Lee JH, Jin SM, Bae EJ, et al. Acute myocarditis in children: clinical aspects and outcomes. J Korean Pediatr Cardiol Soc 2005;9:132–139.34. Drucker NA, Colan SD, Lewis AB, Beiser AS, Wessel DL, Takahashi M, et al. γ-globulin treatment of acute myocarditis in the pediatric population. Circulation 1994;89:252–257.
[Article] [PubMed]

 About
About Browse articles
Browse articles For contributors
For contributors