All issues > Volume 53(12); 2010
Lung interstitial cells during alveolarization
- Corresponding author: Chang Won Choi, M.D. Department Pediatrics, Seoul National University Bundang Hospital, 166 Gumiro, Bundang-gu, Seongnam-si, Gyeonggi-do, 463-707, Korea. Tel: +82.31-787-7286, Fax: +82.31-787-4054, choicw@snu.ac.kr
- Received November 16, 2010 Accepted November 30, 2010
- Abstract
-
Recent progress in neonatal medicine has enabled survival of many extremely low-birth-weight infants. Prenatal steroids, surfactants, and non-invasive ventilation have helped reduce the incidence of the classical form of bronchopulmonary dysplasia characterized by marked fibrosis and emphysema. However, a new form of bronchopulmonary dysplasia marked by arrest of alveolarization remains a complication in the postnatal course of extremely low-birth-weight infants. To better understand this challenging complication, detailed alveolarization mechanisms should be delineated. Proper alveolarization involves the temporal and spatial coordination of a number of cells, mediators, and genes. Cross-talk between the mesenchyme and the epithelium through soluble and diffusible factors are key processes of alveolarization. Lung interstitial cells derived from the mesenchyme play a crucial role in alveolarization. Peak alveolar formation coincides with intense lung interstitial cell proliferation. Myofibroblasts are essential for secondary septation, a critical process of alveolarization, and localize to the front lines of alveologenesis. The differentiation and migration of myofibroblasts are strictly controlled by various mediators and genes. Disruption of this finely controlled mechanism leads to abnormal alveolarization. Since arrest in alveolarization is a hallmark of a new form of bronchopulmonary dysplasia, knowledge regarding the role of lung interstitial cells during alveolarization and their control mechanism will enable us to find more specific therapeutic strategies for bronchopulmonary dysplasia. In this review, the role of lung interstitial cells during alveolarization and control mechanisms of their differentiation and migration will be discussed.
- Introduction
- Introduction
Bronchopulmonary dysplasia (BPD) that develops after surfactant and non-invasive ventilation therapy is characterized by alveolar developmental arrest. In recent times, most preterm infants with BPD have been born between the late canalicular and early saccular stages, during which active acini and alveolar sac formation occurs. Preterm infants born in this period have to breathe with structurally and functionally immature lungs. In a majority of such cases, ventilation assistance and supplemental oxygen are required for survival. Lung development involves the temporal and spatial coordination of a number of transcription and growth factors and cell-cell interactions. This precise developmental process is disrupted in prematurely born infants by various means, including hyperoxia, mechanical stretch, and inflammation1-3).Until the saccular stage, alveolar sacs are made by dichotomous branching tubules4, 5). Further extension of the gas exchange surface from the alveolar sacs occurs through a different mechanism termed alveolar septation. Saccular walls are subdivided by the protrusion of secondary septa that grow perpendicularly into the air space6). Lung interstitial cells play crucial roles in secondary septa formation, and their number markedly increases during alveolarization and decreases thereafter7).
- Elastic fibers
- Elastic fibers
The lung consists of 3 interconnected elastic fiber systems8). Axial elastic fibers originate from the bronchiolar wall and form an outline of alveolar ducts. Peripheral elastic fibers are connected to the pleura and penetrate the area beneath alveolar acini. Septal elastic fibers appear as saccules and alveoli forms and are anchored to both axial and peripheral elastic fiber systems9, 10). Elastin is a very stable molecule and once interconnection of these elastic fiber systems is completed, the components retain their configuration11).
- Lung fibroblasts
- Lung fibroblasts
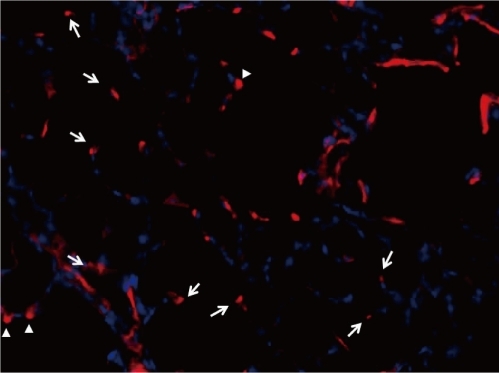
Two subsets of interstitial cells exist during lung development, including myofibroblasts or nonlipid lung interstitial cells and lipofibroblasts or lipid interstitial cells12), and appear to be derived from the same mesenchymal cells. However, the cells show varying growth rates at any age and are hypothesized to be separate populations13, 14). Lipofibroblasts contain lipid droplets containing triglycerides, cholesterol esters, and retinyl esters, and are present at the base of elongating septa during alveolar septation15, 16). Lipofibroblasts are thought to supply triglycerides for surfactant phospholipid synthesis15). More importantly, these cells are a source of retinoic acid, which has a major role in alveolarization.Myofibroblasts lack lipid droplets and express smooth muscle actin. They are contractile cells and the source of septal elastin17). Myofibroblasts are located in developing secondary crests and at septal tips during the alveolar stage of lung development and are thus called alveolar myofibroblasts18). They are dual positive for elastin and smooth muscle actin in immunostaining assays, suggesting a role in elastin formation19). Alveolar myofibroblasts have morphologic and biochemical characteristics intermediate to fibroblasts and smooth muscle cells. During the pseudogladular stage of lung development, progenitors of alveolar myofibroblasts exist as a population of lung mesenchymal cells expressing platelet derived growth factor receptor (PDGFR)-α around the distal lung epithelial tubules and buds20). During the canalicular and saccular stages, these PDGFR-α-positive cells spread from their location around the distal epithelial buds to the walls of prospective terminal saccules to eventually become alveolar myofibroblasts (Fig. 1). Alveolar myofibroblasts are critical for secondary septa formation. Their absence is associated with a lack of secondary septation and the alveolarization failure21). Dysregulated myofibroblast development has been implicated in BPD22). Alveolar myofibroblasts are abundant during alveolarization, but are absent in adult lungs23). Because an excess of myofibroblasts is implicated in fibrotic diseases, alveolar myofibroblast disappearance following alveolarization completion may be critical. However, the regulatory mechanism of survival during alveolarization and subsequent disappearance of alveolar myofibroblasts is poorly understood.
- Elastic fiber formation and alveolar septation
- Elastic fiber formation and alveolar septation
The force necessary for lifting the alveolar crest from the primary septa wall is thought to be produced by septal elastic fibers. First, elastic fibers accumulate in the thickened area of primary septa (septal crest). Secondary, this thickened area grows into secondary crest that protrudes perpendicularly from the saccular wall into air space. Finally, secondary crest further extends into secondary septa. During this process, elastic fiber deposits are always located at the fore-end of developing secondary septa (Fig. 2). This feature is universally observed in all species, including humans26). Mechanical stress to elastic fibers located along saccular wall bends is believed to cause the fibers to protrude from the saccular walls, leading to new septum formation6). However, another theory involves a repulsive signal to epithelial cells in the primary septum may push the secondary septum into air space. In this theory, myofibroblasts simply follow epithelial cells27).The essential role of elastic fibers in septation is supported by various studies. Elastin expression in cultured fibroblasts isolated from rat lung at various postnatal ages is consistent with the degree of septation28).Hyperoxia that inhibits alveolarization also significantly decreases elastin expression29). In vivo studies demonstrate that postnatal lysyl oxidase (LOX) inhibition or inactivation of the LOX gene, which interferes with elastin and collagen synthesis, leads to alveolar septation impairment30, 31). In various pathological conditions leading to impaired alveolarization, such as in a premature lamb BPD model32), a transgenic arrested alveolarization model in mice33), mechanically ventilated newborn mice34), and congenital diaphragmatic hernia35), elastin synthesis was consistently disrupted. Thick and tortuous elastic fibers formed disorganized meshwork along alveolar walls instead of their normal location at septal tips.
- Control of myofibroblast differentiation and migration
- Control of myofibroblast differentiation and migration
Transforming growth factor β1 (TGF-β1) plays a crucial role in lung myofibroblast differentiation36). In vitro TGF-β1 stimulates smooth muscle actin and tropoelastin expression in lung fibroblasts37). In rats, active TGF-β1 and TGF-β receptors increase before alveolar septation. Mice devoid of smad3, a major intracellular downstream signal transducer in the TGF-β1 pathway, show inhibited alveolarization with concomitant decreased expression of tropoelastin38, 39). As alveolar septation begins, expression and localization of TGF-β family members and bone morphogenetic proteins (BMPs) concurrently are changed40). This indicates that these proteins are involved in alveolar septation. TGF-β also plays a role in lung fibrosis development41). TGF-β is also increased in preterm infants with BPD and excessive TGF-β expression is associated with alveolarization inhibition in neonatal animals42, 43). Hyperoxia increases TGF-β expression and induces excessive myofibroblast differentiation, but impairs BMP signaling44, 45). These findings suggest that precise balance of control between TGF-β and BMP signaling is essential to alveolar septation.Platelet-derived growth factor A (PDGF-A) also plays a crucial role in alveolar septation. Disruption of the PDGF-A gene results in failure of elastic fiber deposition in saccular walls and secondary septation. PDGF-A is produced by epithelial cells and acts as a chemoattractant, allowing myofibroblast precursors expressing PDGFRα to migrate to peripheral locations46). Thus, PDGFRα expression by alveolar myofibroblasts is not only a marker, but also has functional consequences.Insulin-like growth factor I (IGF-I) released by epithelial cells is involved in myofibroblast proliferation, differentiation, and migration. Exogenous IGF-I enhanced migration and proliferation of fibroblasts in vitro and the extent of alveolar development was well correlated with IGF-I levels in animal models47, 48). IGF-I increases α-smooth muscle actin expression and collagen synthesis in developing lung fibroblasts49).
- Fibroblast growth factor (FGF) signaling in alveolarization
- Fibroblast growth factor (FGF) signaling in alveolarization
Fibroblast growth factors (FGFs) play crucial roles in various steps of lung development50) and are mediated by tyrosine kinase receptors (FGFR1-4)51). Alveolar septation coincides with increased FGFR3 and FGFR4 expression52). In mice devoid of both receptors, alveolar septation did not occur, but myofibroblasts were present and elastin formation occurred. However, elastin deposition occurred at atypical locations other than tip of growing septa and elastin formation failed to cease and contined to accumulate into adulthood53). FGF2 down-regulates elastin synthesis and LOX activity and is thus considered involved in septal elastogenesis arrest54, 55). Unlike FGF2, FGF18 appears to be involved in elastogenesis. An increased FGF18 level coincident with the beginning of alveolar septation has been observed in human fetal lung and postnatal rat lung56). FGF18 coordinately up-regulates tropoelastin and LOX expression in isolated rat lung fibroblasts56). FGF18 expression markedly decreases in alveolarization arrest animal models induced by hyperoxia57). FGF18 expression is also reduced in the hypoplastic lung of human fetuses with congenital diaphragmatic hernia58). Enhancement of lung growth coincides with the restoration of FGF18 expression, elastic fiber density and location, and alveolar septation58). FGF7 (keratinocyte growth factor) is expressed exclusively in interstitial cells, but its specific receptor, FGFR2IIIb, is found only in epithelial cells59, 60). This implies that FGF7 may be involved in pulmonary mesenchymal-epithelial interactions. Recently, FGF7 was reported to affect alveolar septation by enhancing vascular bed growth61). FGF9 controls mesenchymal cell proliferation in the prenatal lung and FGF9 signaling is necessary for distal lung capillary development62, 63).
- Alveolarization-related gene expression in myofibroblasts
- Alveolarization-related gene expression in myofibroblasts
It can be assumed that genes predominantly expressed in newly forming septa are involved in alveolarization. Galectin 1, a β-galactosidase-binding protein involved in regulation of cell proliferation, differentiation, and apoptosis, was concentrated in myofibroblasts located at the septal tip with peak level at the time of active alveolar septation64). This suggests an important role of galectin-1 in alveolarization. In fibroblasts isolated from developing rat lungs, 2 groups of genes showed markedly opposite expression patterns before, during, and after alveolar septation65). Genes up-regulated during septation and down-regulated afterward are the transcription factors Hoxa2, 4, 5, and retinoid X receptor γ (RXR γ), and 3 genes involved in Wnt signaling, Wnt5a, Norrie disease protein (Ndp), and the receptor frizzled 1 (Fzd1). Their protein products were detected in the septal crest and tips of growing septa. Fzd1 is reported to be involved in myofibroblast proliferation and differentiation66). Genes down-regulated during septation and up-regulated thereafter include cartilage oligomeric protein, osteopontin, osteoactivin, TnX, and schlafen 4. Their expression profiles suggest involvement in the alveolar wall thinning and microvascular maturation phases. Notably, expression of genes up- and down-regulated during septation decreased or was enhanced, respectively, in arrested alveolarization models65). This observation suggests that alveolarization not only involves up-regulation of specific genes but also requires down-regulation of other sets of genes.
- Conclusion
- Conclusion
Lung interstitial cells, especially alveolar myofibroblasts, are essential for secondary septation, a critical process in alveolarization. The locations of myofibroblasts during lung development and their disappearance after the completion of alveolarization imply their crucial role in the formation of new gas exchange units. The differentiation and migration of myofibroblasts is strictly controlled by various mediators and genes. Thus, any disruption in control pathways may lead to abnormal alveolarization. To increase the understanding of BPD, a representative disorder of disrupted alveolarization, fine mechanisms involved in survival, cell-cell interactions, and disappearance of lung myofibroblasts should be searched.
- References
- 1. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001;163:1723–1729.
[Article] [PubMed]2. Baraldi E, Filippone M. Chronic lung disease after premature birth. N Engl J Med 2007;357:1946–1955.
[Article] [PubMed]3. Watterberg KL, Demers LM, Scott SM, Murphy S. Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics 1996;97:210–215.
[Article] [PubMed]4. Hilfer SR. Morphogenesis of the lung: control of embryonic and fetal branching. Annu Rev Physiol 1996;58:93–113.
[Article] [PubMed]5. Metzger RJ, Klein OD, Martin GR, Krasnow MA. The branching programme of mouse lung development. Nature 2008;453:745–750.
[Article] [PubMed] [PMC]6. Burri PH. In: MacDonald JA,Structural aspects of prenatal and postnatal development and growth of the lung. editor. Lung growth and development. 1997New York: Marcel Dekker, :1–35.7. Kauffman SL, Burri PH, Weibel ER. The postnatal growth of the rat lung. II. Autoradiography. Anat Rec 1974;180:63–76.
[Article] [PubMed]8. Weibel ER. In: Macklem PT, Mead J,Functional morphology of lung parenchyma. editors. Handbook of Physiology. Section 3: The respiratory system. Vol III. Part 1. 1986Bethesda: American Physiological Society, :89–111.9. Weibel ER, Bachofen H. In: Crystal RG, West JB,The fiber scaffold of lung parenchyma. editors. The Lung: Scientific Foundations. 1991Vol 1. New York: Raven Press, :787–794.10. Burri PH, Weibel ER. In: Hodson WA,Ultrastructure and morphometry of the developing lung. editor. Lung Biology in Health and Disease. Development of the Lung. 1977Vol 6. New York: Marcel Dekker, :215–268.12. McGowan SE, Torday JS. The pulmonary lipofibroblast (lipid interstitial cell) and its contributions to alveolar development. Annu Rev Physiol 1997;59:43–62.
[Article] [PubMed]13. Brody JS, Kaplan NB. Proliferation of alveolar interstitial cells during postnatal lung growth. Evidence for two distinct populations of pulmonary fibroblasts. Am Rev Respir Dis 1983;127:763–770.
[PubMed]14. Awonusonu F, Srinivasan S, Strange J, Al-Jumaily W, Bruce MC. Developmental shift in the relative percentages of lung fibroblast subsets: role of apoptosis postseptation. Am J Physiol 1999;277(4 Pt 1): L848–L859.
[Article] [PubMed]15. Torday J, Hua J, Slavin R. Metabolism and fate of neutral lipids of fetal lung fibroblast origin. Biochim Biophys Acta 1995;1254:198–206.
[Article] [PubMed]16. Vaccaro C, Brody JS. Ultrastructure of developing alveoli. I. The role of the interstitial fibroblast. Anat Rec 1978;192:467–479.
[Article] [PubMed]17. Powell DW, Mifflin RC, Valentich JD, Crowe SE, Saada JI, West AB. Myofibroblasts. I. Paracrine cells important in health and disease. Am J Physiol 1999;277:C1–C9.
[Article] [PubMed]18. Dickie R, Wang YT, Butler JP, Schulz H, Tsuda A. Distribution and quantity of contractile tissue in postnatal development of rat alveolar interstitium. Anat Rec (Hoboken) 2008;291:83–93.
[Article] [PubMed]19. Noguchi A, Reddy R, Kursar JD, Parks WC, Mecham RP. Smooth muscle isoactin and elastin in fetal bovine lung. Exp Lung Res 1989;15:537–552.
[Article] [PubMed]20. Kim N, Vu TH. Parabronchial smooth muscle cells and alveolar myofibroblasts in lung development. Birth Defects Res C Embryo Today 2006;78:80–89.
[Article] [PubMed]21. Alejandre-Alcazar MA, Kwapiszewska G, Reiss I, Amarie OV, Marsh LM, Sevilla-Perez J, et al. Hyperoxia modulates TGF-beta/BMP signaling in a mouse model of bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol 2007;292:L537–L549.
[Article] [PubMed]22. Bland RD. Neonatal chronic lung disease in the post-surfactant era. Biol Neonate 2005;88:181–191.
[Article] [PubMed]23. Yamada M, Kurihara H, Kinoshita K, Sakai T. Temporal expression of alpha-smooth muscle actin and drebrin in septal interstitial cells during alveolar maturation. J Histochem Cytochem 2005;53:735–744.
[Article] [PubMed]24. Maksvytis HJ, Niles RM, Simanovsky L, Minassian IA, Richardson LL, Hamosh M, et al. In vitro characteristics of the lipid-filled interstitial cell associated with postnatal lung growth: evidence for fibroblast heterogeneity. J Cell Physiol 1984;118:113–123.
[Article] [PubMed]25. McGowan SE, Jackson SK, Doro MM, Olson PJ. Peroxisome proliferators alter lipid acquisition and elastin gene expression in neonatal rat lung fibroblasts. Am J Physiol 1997;273:L1249–L1257.
[Article] [PubMed]26. Nakamura Y, Fukuda S, Hashimoto T. Pulmonary elastic fibers in normal human development and in pathological conditions. Pediatr Pathol 1990;10:689–706.
[Article] [PubMed]27. Prodhan P, Kinane TB. Developmental paradigms in terminal lung development. Bioessays 2002;24:1052–1059.
[Article] [PubMed]28. Noguchi A, Firsching K, Kursar JD, Reddy R, Developmental changes. Developmental changes of tropoelastin synthesis by rat pulmonary fibroblasts and effects of dexamethasone. Pediatr Res 1990;28:379–382.
[Article] [PubMed]29. Bruce MC, Honaker CE. Transcriptional regulation of tropoelastin expression in rat lung fibroblasts: changes with age and hyperoxia. Am J Physiol 1998;274:L940–L950.
[Article] [PubMed]30. Kida K, Thurlbeck WM. The effects of beta-aminopropionitrile on the growing rat lung. Am J Pathol 1980;101:693–710.
[PubMed] [PMC]31. Maki JM, Sormunen R, Lippo S, Kaarteenaho-Wiik R, Soininen R, Myllyharju J. Lysyl oxidase is essential for normal development and function of the respiratory system and for the integrity of elastic and collagen fibers in various tissues. Am J Pathol 2005;167:927–936.
[Article] [PubMed] [PMC]32. Albertine KH, Jones GP, Starcher BC, Bohnsack JF, Davis PL, Cho SC, et al. Chronic lung injury in preterm lambs. Disordered respiratory tract development. Am J Respir Crit Care Med 1999;159:945–958.
[Article] [PubMed]33. Le Cras TD, Hardie WD, Deutsch GH, Albertine KH, Ikegami M, Whitsett JA, et al. Transient induction of TGF-alpha disrupts lung morphogenesis, causing pulmonary disease in adulthood. Am J Physiol Lung Cell Mol Physiol 2004;287:L718–L729.
[Article] [PubMed]34. Bland RD, Ertsey R, Mokres LM, Xu L, Jacobson BE, Jiang S, et al. Mechanical ventilation uncouples synthesis and assembly of elastin and increases apoptosis in lungs of newborn mice. Prelude to defective alveolar septation during lung development? Am J Physiol Lung Cell Mol Physiol 2008;294:L3–L14.
[Article] [PubMed]35. Benachi A, Delezoide AL, Chailley-Heu B, Preece M, Bourbon JR, Ryder T. Ultrastructural evaluation of lung maturation in a sheep model of diaphragmatic hernia and tracheal occlusion. Am J Respir Cell Mol Biol 1999;20:805–812.
[Article] [PubMed]36. Hashimoto S, Gon Y, Takeshita I, Matsumoto K, Maruoka S, Horie T. Transforming growth Factor-beta1 induces phenotypic modulation of human lung fibroblasts to myofibroblast through a c-Jun-NH2-terminal kinase-dependent pathway. Am J Respir Crit Care Med 2001;163:152–157.
[Article] [PubMed]37. McGowan SE, Jackson SK, Olson PJ, Parekh T, Gold LI. Exogenous and endogenous transforming growth factors-beta influence elastin gene expression in cultured lung fibroblasts. Am J Respir Cell Mol Biol 1997;17:25–35.
[Article] [PubMed]38. Bonniaud P, Kolb M, Galt T, Robertson J, Robbins C, Stampfli M, et al. Smad3 null mice develop airspace enlargement and are resistant to TGF-beta-mediated pulmonary fibrosis. J Immunol 2004;173:2099–2108.
[Article] [PubMed]39. Chen H, Sun J, Buckley S, Chen C, Warburton D, Wang XF, et al. Abnormal mouse lung alveolarization caused by Smad3 deficiency is a developmental antecedent of centrilobular emphysema. Am J Physiol Lung Cell Mol Physiol 2005;288:L683–L691.
[Article] [PubMed]40. Alejandre-Alcazar MA, Shalamanov PD, Amarie OV, Sevilla-Perez J, Seeger W, Eickelberg O, Morty RE. Temporal and spatial regulation of bone morphogenetic protein signaling in late lung development. Dev Dyn 2007;236:2825–2835.
[Article] [PubMed]41. Sime PJ, O'Reilly KM. Fibrosis of the lung and other tissues: new concepts in pathogenesis and treatment. Clin Immunol 2001;99:308–319.
[Article] [PubMed]42. Bartram U, Speer CP. The role of transforming growth factor beta in lung development and disease. Chest 2004;125:754–765.
[Article] [PubMed]43. Vicencio AG, Eickelberg O, Stankewich MC, Kashgarian M, Haddad GG. Regulation of TGF-beta ligand and receptor expression in neonatal rat lungs exposed to chronic hypoxia. J Appl Physiol 2002;93:1123–1130.
[Article] [PubMed]44. Rehan V, Torday J. Hyperoxia augments pulmonary lipofibroblast-to-myofibroblast transdifferentiation. Cell Biochem Biophys 2003;38:239–250.
[Article] [PubMed]45. Bostrom H, Willetts K, Pekny M, Leveen P, Lindahl P, Hedstrand H, et al. PDGF-A signaling is a critical event in lung alveolar myofibroblast development and alveogenesis. Cell 1996;85:863–873.
[Article] [PubMed]46. Lindahl P, Karlsson Hellstrom M, Gebre-Medhin S, Willetts K, Heath JK, Betsholtz C. Alveogenesis failure in PDGF-A-deficient mice is coupled to lack of distal spreading of alveolar smooth muscle cell progenitors during lung development. Development 1997;124:3943–3953.
[Article] [PubMed]47. Chetty A, Faber S, Nielsen HC. Epithelial-mesenchymal interaction and insulin-like growth factors in hyperoxic lung injury. Exp Lung Res 1999;25:701–718.
[Article] [PubMed]48. Liu H, Chang L, Rong Z, Zhu H, Zhang Q, Chen H, Li W. Association of insulin-like growth factors with lung development in neonatal rats. J Huazhong Univ Sci Technolog Med Sci 2004;24:162–165.
[Article] [PubMed]49. Chetty A, Cao GJ, Nielsen HC. Insulin-like Growth Factor-I signaling mechanisms, type I collagen and alpha smooth muscle actin in human fetal lung fibroblasts. Pediatr Res 2006;60:389–394.
[Article] [PubMed]50. Warburton D, Bellusci S. The molecular genetics of lung morphogenesis and injury repair. Paediatr Respir Rev 2004;5(Suppl A): S283–S287.
[Article] [PubMed]51. Itoh N. The Fgf families in humans, mice, and zebrafish: their evolutional processes and roles in development, metabolism, and disease. Biol Pharm Bull 2007;30:1819–1825.
[Article] [PubMed]52. Powell PP, Wang CC, Horinouchi H, Shepherd K, Jacobson M, Lipson M, et al. Differential expression of fibroblast growth factor receptors 1 to 4 and ligand genes in late fetal and early postnatal rat lung. Am J Respir Cell Mol Biol 1998;19:563–572.
[Article] [PubMed]53. Weinstein M, Xu X, Ohyama K, Deng CX. FGFR-3 and FGFR-4 function cooperatively to direct alveogenesis in the murine lung. Development 1998;125:3615–3623.
[Article] [PubMed]54. Rich CB, Fontanilla MR, Nugent M, Foster JA. Basic fibroblast growth factor decreases elastin gene transcription through an AP1/cAMP-response element hybrid site in the distal promoter. J Biol Chem 1999;274:33433–33439.
[Article] [PubMed]55. Feres-Filho EJ, Menassa GB, Trackman PC. Regulation of lysyl oxidase by basic fibroblast growth factor in osteoblastic MC3T3-E1 cells. J Biol Chem 1996;271:6411–6416.
[Article] [PubMed]56. Chailley-Heu B, Boucherat O, Barlier-Mur AM, Bourbon JR. FGF-18 is upregulated in the postnatal rat lung and enhances elastogenesis in myofibroblasts. Am J Physiol Lung Cell Mol Physiol 2005;288:L43–L51.
[Article] [PubMed]57. Wagenaar GT, ter Horst SA, van Gastelen MA, Leijser LM, Mauad T, van der Velden PA, et al. Gene expression profile and histopathology of experimental bronchopulmonary dysplasia induced by prolonged oxidative stress. Free Radic Biol Med 2004;36:782–801.
[Article] [PubMed]58. Boucherat O, Benachi A, Barlier-Mur AM, Franco-Montoya ML, Martinovic J, Thebaud B, et al. Decreased lung fibroblast growth factor 18 and elastin in human congenital diaphragmatic hernia and animal models. Am J Respir Crit Care Med 2007;175:1066–1077.
[Article] [PubMed]59. Aaronson SA, Bottaro DP, Miki T, Ron D, Finch PW, Fleming TP, et al. Keratinocyte growth factor. A fibroblast growth factor family member with unusual target cell specificity. Ann N Y Acad Sci 1991;638:62–77.
[Article] [PubMed]60. Orr-Urtreger A, Bedford MT, Burakova T, Arman E, Zimmer Y, Yayon A, et al. Developmental localization of the splicing alternatives of fibroblast growth factor receptor-2 (FGFR2). Dev Biol 1993;158:475–486.
[Article] [PubMed]61. Padela S, Yi M, Cabacungan J, Shek S, Belcastro R, Masood A, Jankov RP, Tanswell AK. A critical role for fibroblast growth factor-7 during early alveolar formation in the neonatal rat. Pediatr Res 2008;63:232–238.
[Article] [PubMed]62. Colvin JS, White AC, Pratt SJ, Ornitz DM. Lung hypoplasia and neonatal death in Fgf9-null mice identify this gene as an essential regulator of lung mesenchyme. Development 2001;128:2095–2106.
[Article] [PubMed]63. White AC, Lavine KJ, Ornitz DM. FGF9 and SHH regulate mesenchymal Vegfa expression and development of the pulmonary capillary network. Development 2007;134:3743–3752.
[Article] [PubMed]64. Foster JJ, Goss KL, George CL, Bangsund PJ, Snyder JM. Galectin-1 in secondary alveolar septae of neonatal mouse lung. Am J Physiol Lung Cell Mol Physiol 2006;291:L1142–L1149.
[Article] [PubMed]

 About
About Browse articles
Browse articles For contributors
For contributors