All issues > Volume 54(7); 2011
Nutritional management of breastfeeding infants for the prevention of common nutrient deficiencies and excesses
- Corresponding author: Jin Soo Moon, MD. Department of Pediatrics, Inje University Ilsan Paik Hospital, 2240 Daehwa-dong, Ilsnaseo-gu, Goyang 411-706, Korea. Tel: +82-31-910-7101, Fax: +82-31-910-7108, jsmoon@paik.ac.kr
- Received June 20, 2011 Accepted June 27, 2011
- Abstract
-
Breastfeeding is the best source of nutrition for every infant, and exclusive breastfeeding for 6 months is usually optimal in the common clinical situation. However, inappropriate complementary feeding could lead to a nutrient-deficient status, such as iron deficiency anemia, vitamin D deficiency, and growth faltering. The recent epidemic outbreak of obesity in Korean children emphasizes the need for us to control children's daily sedentary life style and their intakes of high caloric foods in order to prevent obesity. Recent assessment of breastfeeding in Korea has shown that the rate is between 63% and 89%; thus, up-to-dated evidence-based nutritional management of breastfeeding infants to prevent common nutrient deficiencies or excesses should be taught to all clinicians and health care providers.
- Introduction
- Introduction
The importance of breast milk feeding (BMF) has been emphasized by many academic bodies and health authorities in the world, including WHO and UNICEF1,2). For many years the Korean Pediatric Society has also been a strong advocate of the need to increase BMF in Korea3,4). The superior benefits of BMF compared to those of alternative nutritional sources for infants are well known, and include more optimal infantile neurobehavioral development, reduced tendency to catch infectious diseases, reduced tendency toward obesity, and fewer allergenic properties. Therefore, there is little need for similar additional comments in this review5-8). However, there is still much debate about the details of BMF in specific regions such as North and South Korea, particularly how long exclusive BMF should be maintained, and what type of dietary supplements could be helpful to BMF infants. Recently in Korea, we have encountered re-emerging nutritional problems in the era of increased BMF rates, such as iron deficiency anemia (IDA) and vitamin D deficiency rickets; thus, questions of how we can detect and manage nutritional deficiencies related to BMF should be addressed9). In this article, an overview of BMF status in Korea will be briefly summarized, and the practical aspects of nutritional management in BMF infants, focusing on recently emerging nutritional issues, will be discussed.
- Current epidemiology of breast milk feeding in Korea
- Current epidemiology of breast milk feeding in Korea
Breastfeeding rates in Korea have changed dramatically in recent decades, concomitant with socioeconomic advances (Fig. 1)3,10-12). Before 1970, BMF rates were very high, because there were few alternatives to breast milk. Then, many dairy products were introduced with commercial marketing, and cow's milk-based formulae became more and more popular in Korea. Eventually, BMF rates fell to approximately 10% in the early 1990s. Since the late 1990s, UNICEF, along with many Korean pediatricians, developed community-based movements to enhance BMF in Korea, and several programs, such as the "Baby-friendly hospital initiative," were launched with governmental support. A recent epidemiologic survey in 2009 showed that the overall BMF rate in Korea was 89.0% (±1.2 SE) and the exclusive BMF rate at 6 months of age was 49.3% (±2.0 SE)11).
- Common clinical problems associated with increased breastfeeding rates
- Common clinical problems associated with increased breastfeeding rates
- 1. Nutrient Deficiencies
- 1. Nutrient Deficiencies
1) Iron: iron deficiency anemia
1) Iron: iron deficiency anemia
IDA can be a relatively common problem encountered by clinicians in exclusively breastfed infants. Most infantile cases with mild IDA can easily recover to normal hemoglobin levels if appropriate complementary feeding is initiated, even with continued BMF13). However, many experts are concerned about IDA and iron deficiency without clinical symptoms, which may lead to detrimental neurodevelopment14-16). In order to avoid the possibility of IDA or iron deficiency, the American Academy of Pediatrics (AAP) recommends a prophylactic dose of oral iron (1 mg/kg/day) for infants who are exclusively breastfed after 4 months of age17). However, this guideline has been questioned by the Section on Breastfeeding in the AAP, due to concerns about unnecessary iron therapy and weak evidence13). In Korea, there is no consensus on the prophylactic use of iron supplements; however, many reports on IDA rates in breastfed infants have been published recently9,18).2) Vitamin D: vitamin D deficiency rickets
2) Vitamin D: vitamin D deficiency rickets
Normal vitamin D levels typically vary greatly according to ethnic groups, seasonal sun exposure, and dietary intake, and so on19,20). Therefore, it is very difficult to establish normal levels in children and determine the prevalence of vitamin D deficiency in this population. The AAP recommends a minimum intake of 200 IU of vitamin D per day for infants in the first 2 months of life21). Currently, there are no official prevalence data and clinical guidelines available for vitamin D deficiency in Korean children. According to the guidelines in developed countries, introduction of meats to the daily complementary foods may be helpful to prevent this vitamin deficiency and iron deficiency anemia.3) Calcium
3) Calcium
A recent nutritional survey report showed that the prevalence of low calcium intake over the age of 1 year was 71.1% (±0.4 SE)11). Although there are many sources of calcium in Korean foods, dairy products are the best source, especially in respect of the availability. Infants over the age of 1 year should be offered two cups of milk daily. Low-fat milk can be used if the child's body mass index (BMI) is above the 95th percentile according to standard growth charts. However, low-fat milk should not be given to an infant under 2 years of age22).4) Special conditions such as preterm infants and infants with chronic diseases
4) Special conditions such as preterm infants and infants with chronic diseases
Infants with chronic diseases and preterm babies with BMF may have relative nutritional deficiencies. Calories, calcium, vitamin D, iron, or zinc, etc., may be in short supply as a result of the disease. For these patients, several human milk fortifiers have been developed in Western countries; however, these are not currently available in Korea. In these situations, early introduction of complementary foods may be an option to supplement nutrient deficits. Multidisciplinary approaches with dieticians, nurses, and pharmacists may be a good solution to support patients with specific chronic problems.
- 2. Excessive nutrients
- 2. Excessive nutrients
1) Carbohydrates and energy
1) Carbohydrates and energy
In Korea, the prevalence of excessive energy intake in the general population is 13.9% (±0.3 SE)11). According to an AAP position paper published in 2009, fruit juice for infants should be limited to less than 180 mL (6 oz) per day. In the epidemic of obesity, carbohydrate excess including fruit juice over-consumption should be controlled to reduce discretionary calories. In addition, fruit juices are also a major cause of dental caries, functional gastrointestinal disorders, and chronic diarrhea. In a National Health Screening Program for Infants in Korea, fruit juices and beverages were also considered restricted foods for infants23).2) Obesity
2) Obesity
The global obesity epidemic is an ongoing problem. Several lines of evidence have shown that BMF itself is the best way to prevent obesity. Although there are few large-scale studies, BMF can reduce or prevent obesity in infants8). Before 6 months of age, normal weight gain in breastfed infants is usually considerably greater than in cow's milk-fed infants; thereafter, the breastfed group shows "faltering" even up to 12 to 15 months24). Nowadays, this phenomenon is accepted as normal to some extent according to extensive research studies by several groups, including WHO. However, recent research has shown that it is important to differentiate groups that require intervention25). Body Mass Index (BMI) or weight for height screening was not considered helpful in infants less than 2 years of age. However, recently, WHO has published new BMI charts for children less than 2 years of age for early intervention to prevent obesity26).Recent research in the US has shown that there are large differences in discretionary calorie allowance among sedentary, moderately active, and active children27). Energy intake needs to be moderated in less active children. It is very important for parents to encourage their children to exercise moderately for at least 1 hour per day and limit video screen time to less than 2 hours per day28).
- Nutritional guideline updates
- Nutritional guideline updates
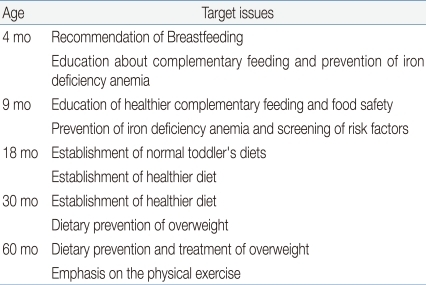
In 2007, the National Health Screening Program for Infant s was launched in Korea. The purpose of this government-driven program is to screen for failure of growth and development in children, Providing proper information about child health was also an important issue in this program. Nutritional guidelines are a key element for health education in the National Health Screening Program of Korea. The target issues in the nutritional guidelines are summarized in Table 1. This program is focused on exclusive breastfeeding for 6 months duration, restricting consumption of fruit juices and other beverages, teaching good dietary habits, preventing obesity, and encouraging exercise.Recent guidelines published in 2008 by the European Society of Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN), summarize new evidence on breastfeeding and complementary feeding7,8). ESPGHAN reported that the ideal period to start complementary feeding in European infants is between 17 and 26 weeks. They also stressed that there is very little evidence to restrict any type of food to prevent allergy in normal infants. Too many recommendations have been given for the restriction of complementary foods despite a lack of evidence, and anticipatory restriction without evidence can only lead to nutritional inadequacies.
- Summary
- Summary
- Exclusive breastfeeding for 6 months is usually optimal in a typical clinical situation.- Complementary feeding should be initiated at 6 months of age. ESPGHAN reported that the ideal period to start complementary feeding in European infants is between 17 and 26 weeks. Further research is needed to verify this recommendation in local regions.- There is very little evidence to support the restriction of any kind of food to prevent allergy in normal infants.- Routine iron supplementation for breastfed infants has not been supported by good quality evidence; thus, a personalized approach would be the best in this matter. Therefore, detailed guidelines for iron deficiency screening are urgently needed.- Infants over the age of 1 year should be offered two cups of whole milk daily.- To prevent obesity, moderate exercise of at least 1 hour per day, and restriction of TV viewing should be stressed to all parents.- Consumption of fruit juice and beverages in infants should be curtailed to prevent calorie excess, gastrointestinal discomfort, and dental caries.
- References
- 1. World Health Organization. Global strategy for infant and young child feeding. 2003;Geneva: World Health Organization.2. Dewey K. Guiding principles for complementary feeding of the breastfed child. 2001;World Health Organization.3. Kim JY, Hwang SJ, Park HK, Lee H, Kim NS. Analysis of online breast-feeding consultation on the website of the Korean Pediatric Society. Korean J Pediatr 2008;51:1152–1157.
[Article]4. Song KH, Lee YM, Chang JY, Park EY, Park SA, Cho NK, Bae CW. A report on operating a nationwide human milk bank in Korea. Korean J Pediatr 2010;53:488–494.
[Article]5. Brown KH. Breastfeeding and complementary feeding of children up to 2 years of age. Nestle Nutr Workshop Ser Pediatr Program 2007;60:1–10.
[PubMed]6. Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 2007;1–186.
[Article]7. Agostoni C, Decsi T, Fewtrell M, Goulet O, Kolacek S, Koletzko B, et al. Complementary feeding: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 2008;46:99–110.
[Article] [PubMed]8. Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, Michaelsen KF, et al. Breast-feeding: A commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 2009;49:112–125.
[Article] [PubMed]9. Choi EH, Jung SH, Jun YH, Lee YJ, Park JY, You JS, Chang KJ, Kim SK. Iron Deficiency Anemia and Vitamin D Deficiency in Breastfed Infants. Korean J Pediatr Gastroenterol Nutr 2010;13:164–171.
[Article]10. Kim HS, Seo JW, Kim YJ, Lee KH, Kim JY, Ko JS, Bae SH, Park HS. A Follow-up Survey of Mothers' Antenatal Breast-feeding Plans. J Korean Pediatr Soc 2003;46:635–641.11. Korea Health Statistics 2009: Korea NationalHealth and Nutrition Examination Survey (KNHANES IV-3). 2010;Seoul: Korea Center for Disease Control and Prevention, Ministry of Health and Welfare.12. Moon JS, Lee SY, Eun BL, Kim SW, Kim YK, Shin SM, et al. One year evaluation of National Health Screening Program for Infant and Children in Korea. Korean J Pediatr 2010;53:307–313.
[Article]13. Schanler RJ, Feldman-Winter L, Landers S, Noble L, et al. AAP Section on Breastfeeding. Executive Commitee. Concerns with early universal iron supplementation of breastfeeding infants. Pediatrics 2011;127:e1097
[Article] [PubMed]14. Idjradinata P, Pollitt E. Reversal of developmental delays in iron-deficientanaemic infants treated with iron. Lancet 1993;341:1–4.
[Article] [PubMed]15. Lozoff B, Jimenez E, Wolf AW. Long-term developmental outcome of infants with iron deficiency. N Engl J Med 1991;325:687–694.
[Article] [PubMed]16. Tran PV, Fretham SJ, Carlson ES, Georgieff MK. Long-term reduction of hippocampal brain-derived neurotrophic factor activity after fetalneonatal iron deficiency in adult rats. Pediatric research 2009;65:493–498.
[Article] [PubMed] [PMC]17. Baker RD, Greer FR. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age). Pediatrics 2010;126:1040–1050.
[Article] [PubMed]18. Kim BY, Choi EH, Kang SK, Jun YH, Hong YJ, Kim SK. Weaning Food Practice and Assessment in Children with Iron Deficiency Anemia. Korean J Pediatr Gastroenterol Nutr 2009;12:215–220.
[Article]19. Greer FR. Issues in establishing vitamin D recommendations for infants and children. Am J Clin Nutr 2004;80:1759S–1762S.
[Article] [PubMed]20. Rajakumar K, Holick MF, Jeong K, Moore CG, Chen TC, Olabopo F, et al. Impact of season and diet on vitamin d status of african american and caucasian children. Clinical pediatrics 2011;50:493–502.
[Article] [PubMed] [PMC]21. Gartner LM, Greer FR. Prevention of rickets and vitamin D deficiency: new guidelines for vitamin D intake. Pediatrics 2003;111:908–910.
[Article] [PubMed]22. United States. Dept. of Health and Human Services. United States. Dept. of Agriculture. United States. Dietary Guidelines Advisory Committee. Dietary guidelines for Americans, 2010. 2010;7th ed. Washington, D.C.: G.P.O., :xi:95HHS publication.23. Moon JS, Kim JY, Chang SH, Choi KH, Yang HR, Seo JK, et al. Development of nutrition questionnaire and guideline in the Korea national health screening program for infants and children. Korean J Pediatr Gastroenterol Nutr 2008;11:42–55.
[Article]24. Hernandez-Beltran M, Butte N, Villalpando S, Flores-Huerta S, Smith EO. Early growth faltering of rural Mesoamerindian breast-fed infants. Ann Hum Biol 1996;23:223–235.
[Article] [PubMed]25. Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 2010;125:e473–e480.
[Article] [PubMed]26. de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull 2004;25:S15–S26.
[Article] [PubMed]27. United States Department of Health and Human Services. United States Department of Agriculture. United States Dietary Guidelines Advisory Committee. Dietary guidelines for Americans. 2005;6th ed. Washington, D.C.: G.P.O., :ix:71
Fig. 1
The trend in breast milk feeding (BMF) rates has changed dramatically in Korea, accompanied by rapid socioeconomic advances. The boxes represent gross national income per capita, and the line represents the trend of BMF rates in Korea. Easy availability of cow's milk formulae and aggressive marketing might have contributed to the rapid fall in BMF rates nationwide. Recent survey data showed much-improved BMF rates after reinforced government regulations and community-based efforts to enhance BMF were applied. In 2009, the data showed that overall BMF rates recovered up to 89%. Gross national income per capita data were obtained from the Economic Statistics System, Bank of Korea (available at http://ecos.bok.or.kr/).
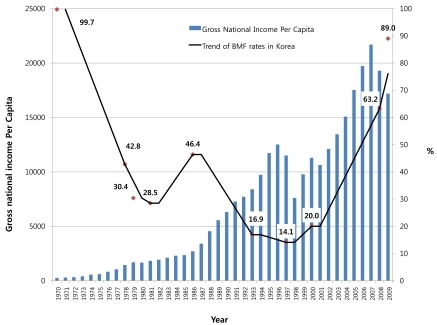
Table 1
Target Issues in the National Health Screening Program for Infants in Korea (Reprinted from Moon JS, Kim JY, Chang SH, Hae CK, Yang HR, Seo JK, et al. Korean J Pediatr Gastroenterol Nutr 2008;11:42-55, with permission of The Korean Society of Pediatric Gastroenterology, Hepatology and Nutrition23).)

 About
About Browse articles
Browse articles For contributors
For contributors
