All issues > Volume 59(5); 2016
Clinical features and prognostic factors in drowning children: a regional experience
- Corresponding author: Hee Joung Choi, MD. Department of Pediatrics, Keimyung University School of Medicine, 56 Dalseong-ro, Jung-gu, Daegu 41931, Korea. Tel: +82-53-250-7524, Fax: +82-53-250-7783, joung756@dsmc.or.kr
- Received August 07, 2015 Revised October 26, 2015 Accepted November 09, 2015
- Abstract
-
- Purpose
- Purpose
- This study aimed to evaluate the clinical features of children who have survived a water submersion incident, and to identify risk factors for prognosis.
- Methods
- Methods
- We retrospectively reviewed the medical records of patients who experienced submersion between January 2005 and December 2014. The patients were classified into 2 groups, according to complications, and prognostic factors were evaluated.
- Results
- Results
- During the study period, 29 children experienced submersion (20 boys and 9 girls; mean age, 83.8±46.4 months). Submersion occurred most commonly in the summer, with the peak incidence in August. The most frequent Szpilman clinical score was grade 5 (13 patients; 44.8%), followed by grade 6 (7 patients; 24.1%), and grades 1 or 2 (3 patients; 10.3%). Five children (17.2%) in the poor prognosis group died or had hypoxic ischemic encephalopathy, and the overall mortality rate was 6.9%. Poor prognosis after submersion was associated with lower consciousness levels (P=0.003), higher Szpilman scores (P=0.007), greater need for intubation and mechanical ventilator support (P=0.001), and longer duration of oxygen therapy (P=0.015). Poor prognosis was also associated with lower bicarbonate levels (P=0.038), as well as higher sodium, aspartate transaminase (AST), and alanine transaminase (ALT) levels (P=0.034, P=0.006, and P=0.005, respectively). Szpilman clinical scores were positively correlated with consciousness levels (r=0.489, P=0.002) and serum liver enzyme levels (AST and ALT; r=0.521, P=0.004).
- Conclusion
- Conclusion
- We characterized the prognostic factors associated with submersion outcomes, using the Szpilman clinical score, which is comparable to consciousness level for predicting mortality.
- Introduction
- Introduction
Drowning is one of the most common causes of accidental deaths in children throughout the world. The World Health Organization (WHO) reported the global burden of disease data that show that the global mortality rate from drowning is 6.8 per 100,000 person-years1). Furthermore, over half of global mortality cases occur in children younger than 15 years. It is the second leading cause of accidental deaths among children aged 1–14 years in the United Sates2). In South Korea, drowning is the third most common cause of accidental deaths among children between 1 and 9 years of age, with a drowning death rate of 0.7 per 100,000 population in 20133).In the past, a separate definition was used for patients who experienced submersion; that is, fetal cases were referred to as drowning, and nonfetal cases were referred to as near drowning. However, in 2002, a new definition was proposed by the First World Congress on Drowning and the WHO as follows: "Drowning is the process of experiencing respiratory impairment from submersion/immersion in liquid1)."The most important factor to determine the patient's outcome is neurological sequela caused by hypoxia. Many previous studies have investigated risk factors of neurological complication in drowning patients. The duration of submersion, the need of advanced life support at the site of the submersion, the duration of cardiopulmonary resuscitation (CPR), spontaneous breathing, and circulation on arrival at the emergency department are well-known factors associated to neurological outcome in drowning patients4). The initial mental status is an important factor of prognosis, but the objective parameter of consciousness such as the Glasgow Coma Scale (GCS) is not routinely used in pediatric patients. In 1997, the Szpilman clinical score system was proposed as a new classification algorithm to stratify the mortality of drowning5). However, few reports used this system to evaluate the prognosis of drowning children.In this study, we evaluated the clinical features of drowning children and identified the complications and risk factors of prognosis, including the Szpilman clinical score system.
- Materials and Methods
- Materials and Methods
- 1. Patients and data
- 1. Patients and data
We enrolled patients who experienced submersion and admitted to the Dongsan Medical Center and Kyungpook National University Hospital between January 2005 and December 2014. We retrospectively reviewed medical records and collected data, including the patients' characteristics, features of submersion events, physical examination and laboratory findings, medical treatments, complications, and outcome.The patients were classified into 6 subgroups according to the Szpilman clinical score system as follows: grade 1, normal pulmonary auscultation with coughing; grade 2, abnormal pulmonary auscultation with rales in some pulmonary fields; grade 3, pulmonary auscultation of acute pulmonary edema without arterial hypotension; grade 4, pulmonary auscultation of acute pulmonary edema with arterial hypotension; grade 5, isolated respiratory arrest; and grade 6, cardiopulmonary arrest5). Szpilman clinical score was determined at the accident site by 4 clinical parameters including breathing, arterial pulse, pulmonary auscultation, and blood pressure5). The GCS was not used because of insufficient data. Instead, the level of consciousness was described as alert, drowsy, stupor, semicoma, and coma.We divided the patients into 2 groups according to complication. The good prognosis group included patients who fully recovered without neurological impairment, and the poor prognosis group included patients who expired or were diagnosed with hypoxic ischemic encephalopathy (HIE). We also evaluated prognostic factors.- 2. Statistical analysis
- 2. Statistical analysis
All statistical analyses were performed by using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA), and all values were described as frequencies and mean±standard deviations. The chi-square test was used for categorical data, and the unpaired t test and Mann-Whitney U test were applied to compare continuous data between the 2 groups according to normality test. Logistic regression analysis was used to identify prognostic factors, and the results are presented as odds ratios (OR) with 95% confidence intervals. The Spearman rank correlation coefficient (r) was applied to analyze the correlation between the Szpilman clinical score and prognostic factors. A P<0.05 was considered statistically significant.- 3. Ethics statement
- 3. Ethics statement
This study was approved by the Institutional Review Board of the Keimyung University Dongsan Medical Center (approval number: 2014-12-057).
- Results
- Results
- 1. Demographic characteristics of the patients
- 1. Demographic characteristics of the patients
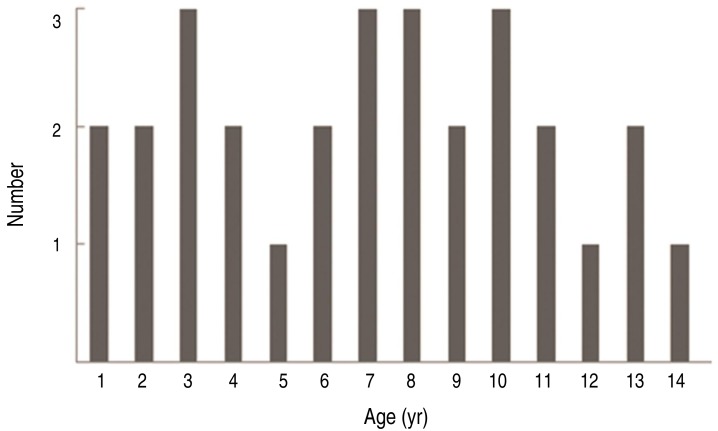
During the study period, 29 patients (20 boys and 9 girls) experienced submersion. The overall male-to-female ratio was 2.2:1. The mean patient age was 83.8±46.4 months (median, 87.0 months; range, 13–172 months). The age distribution of the patients is shown in Fig. 1. Age distribution did not predict clinical status.- 2. Characteristics of the submersion events
- 2. Characteristics of the submersion events
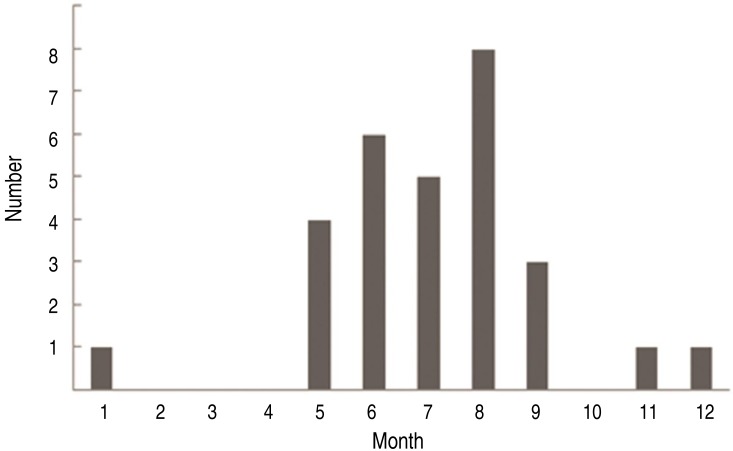
Submersion occurred most commonly in the summer (spring:summer:autumn:winter=4:19:4:2), with a peak incidence in August (Fig. 2). Six cases occurred in the morning, and 23 cases occurred in the afternoon. The overall event time was between 8:00 AM and 11:00 PM. Submersion occurred in indoor places in 9 patients and in outdoor places in 20 patients. The incidence of indoor accident was much higher in children younger than 4 years (77.8%), whereas the incidence of outdoor accident was much higher in children older than 4 years (90%; P=0.001). The specific places of submersion were river in 9, pool in 6, valley in 5, lake in 4, bathtub in 4, and sea in 1.The mean submersion time was 5.6±6.5 minutes (median, 4.5 minutes; range, 1–30 minutes). Eleven cases (38%) of submersion were witnessed by parents, friends, swimming teachers, and lifeguards. The persons who found the patients during submersion were described in 21 cases, who were parents in 10, lifeguards in 6, strangers in 4, and friends in 1. Seventeen patients performed CPR immediately after rescue at the site of the accident.- 3. In-hospital clinical findings
- 3. In-hospital clinical findings
The time of arrival to the hospital after rescue was described in medical records in only 8 patients, and the mean time of arrival to the hospital was 52.1±44.0 minutes (median, 40.0 minutes; range, 15–150 minutes). The patients' consciousness level on arrival at the hospital was alert in 13, drowsy in 6, stupor in 5, semicoma in 1, and coma in 4. The most frequent Szpilman clinical score was grade 5 in 13 patients (44.8%), grade 6 in 7 patients, and grades 1 and 2 in 3 patients. Seven patients required CPR at the time of arrival in the hospital, 3 of whom had no pupillary light reflex. Regarding initial vital signs in the hospital, 3 patients had hypotension, 1 patient had bradycardia, 6 patients had tachypnea, and 5 patients had fever with a body temperature higher than 38℃. Sixteen patients had abnormal lung auscultation such as rales and decreased aeration, and 11 patients were diagnosed as pulmonary edema on chest radiography.- 4. Management and prognosis
- 4. Management and prognosis
Nine patients needed mechanical ventilator support with endotracheal intubation, and the mean duration of mechanical ventilation was 4.7±4.1 days (median, 4.0 days; range, 1–15 days). Oxygen therapy was given to 21 patients, and the mean oxygen supply duration was 3.9±3.5 days (median, 3.0 days; range, 1–15 days). Seventeen patients had fever with a body temperature higher than 38.0℃, and 25 patients were treated with parenteral antibiotics for a suspected lung infection.The mean hospitalization duration was 6.1±4.0 days (median, 5.0 days; range, 2–21 days). Severe complications such as death and HIE were found in 5 patients. Four patients were diagnosed with HIE with abnormal findings on brain magnetic resonance imaging (MRI) and electroencephalography, such as diffuse cortical atrophy on MRI and depressed activity on electroencephalography. There were 2 cases of in-hospital death, resulting in an overall mortality rate of 6.9%. One death occurred within 24 hours of hospital admission because of multiorgan dysfunction, and the other case was brain death in an HIE patient on the 15th hospital day.- 5. Prognostic factors
- 5. Prognostic factors
The poor prognosis group included 5 patients, and the good prognosis group included 24 patients. Differences between the good and poor prognosis groups are shown in Tables 1 and 2. Age, sex, season, and place of submersion had no significant differences between the groups. The poor prognosis group showed a lower level of consciousness (P=0.003) and a higher Szpilman score (P=0.007) than the good prognosis group. All of the patients in the poor prognosis group needed intubation and mechanical ventilator support at a significantly higher incidence than that in the good prognosis group (P=0.001). In addition, the mean oxygen therapy duration was significantly longer in the poor prognosis group than in the good prognosis group (P=0.015).In laboratory findings, the mean bicarbonate (HCO3–) level was significantly lower in the poor prognosis group than in the good prognosis group (P=0.038). The mean sodium, aspartate transaminase (AST), and alanine transaminase (ALT) levels were significantly higher in the poor prognosis group than in the good prognosis group (P=0.034, P=0.006, and P=0.005, respectively).The multivariate logistic regression analysis of the risk factors of poor prognosis showed that no pupillary light reflex (OR, 15.3; P=0.046), hypotension (OR, 40.0; P=0.021), pH<7.2 (OR, 15.8; P=0.019), bicarbonate level<15 mEq/L (OR, 33.0; P=0.011), base excess<-10 mEq/L (OR, 42.0; P=0.005), glucose level>200 mg/dL (OR, 12.8; P=0.031), and liver enzyme levels (AST and ALT) >200 U/L (OR, 10.5; P=0.033) were significantly associated with poor prognosis (Table 3).The Szpilman clinical score of the patients had a significant positive correlation with the level of consciousness (r=0.489, P=0.002) and serum levels of liver enzyme (r=0.521, P=0.004). Though not statistically significant, the Szpilman clinical score positively correlated with serum glucose levels (r=0.303, P=0.150) but negatively correlated with pH level (r=-0.260, P=0.076) and base excess (r=-0.256, P=0.080).
- Discussion
- Discussion
Drowning is the third leading cause of accidental death among children in Korea, accounting for about 14% of the total accidental death rate among children 1–9 years of age3). Previous studies reported that the incidence of drowning peaked in children younger than 4 years and older than 10 years6,7). Boys tend to drown much more than girls, with an overall male-to-female ratio of 3.2–2.4:18,9). Drowning occurred throughout the year, but the incidence was highest in the summer, especially from June to August7,8). Although age distribution was not discriminative in the present study, drowning more frequently occurred in males and in the summer, with a peak incidence in August.The place of submersion differs by age, season, geographic location, and socioeconomic status8,10). The present study showed similar results to other previous studies that younger children (younger than 4–5 years) drowned in indoor water facilities such as bathtubs and artificial pools, whereas older children (older than 4–5 years of age) drowned in outdoor places such as rivers and valleys. We only found 1 case of submersion in seawater, and this low incidence was because of the geographic characteristics of the target region, which is located in a basin surrounded by mountains.Clinical outcome of drowning varies; that is, patients range from asymptomatic to severely distressed with multiorgan impairment11). Once submersion occurred, anoxia is the key point of damage and several organs such as the brain, kidneys, and lungs are mainly affected by hypoxia. Although lung injury is the primary complication in drowning, HIE is the most important complication that affects prognosis. Thus, drowning outcome should to be classified by neurological impairment12). In the present study, the poor prognosis group who died or had HIE included 5 patients (17.2%), and the overall mortality rate was 6.9%.Numerous studies have suggested prognostic factors of drowning. Recent studies in various countries reported that age of 1–3 years, male sex, need for resuscitation, submersion time >10 minutes, GCS score <3–5 points, hypothermia, and pupils without light reaction are common predictors of poor outcome8,9,13,14). In addition, laboratory values such as severe acidosis, low base excess, high blood sugar levels, and high lactate levels are usually signs of long submersion and may be related to poor outcome9,13). In South Korea, few studies reported that initial mental status, submersion time, mechanical ventilation need, pulmonary edema, initial blood glucose level, and initial pH are related to poor prognosis7,15,16). Similarly, we found that the patients with poor prognosis had lower levels of consciousness (P=0.003), higher Szpilman scores (P=0.007), greater need for intubation and mechanical ventilator support (P=0.001), longer oxygen therapy duration (P=0.015), lower bicarbonate level (P=0.038), and higher levels of sodium, AST, and ALT (P=0.034, P=0.006, and P=0.005).The submersion time of the poor prognosis group was longer than that of the good prognosis group in the present study, but it did not show statistical significance. Although submersion time is an essential factor of submersion accident, this information is estimated by eyewitnesses and it is difficult to get accurate information. Moreover, in the present study, 18 cases of accidents were not witnessed and the collected submersion time is somewhat inaccurate. Thus, we used the laboratory values that represent the severity of hypoxia, and we found that the patients with poor prognosis had lower level of bicarbonate (P=0.038), and higher levels of sodium, AST, and ALT (P=0.034, P=0.006, and P=0.005).Level of consciousness is an important prognostic factor in drowning. The most commonly and simply used assessment tools are ABC (awake, blunted, and comatose) score and the GCS score12). In the present study, the GCS was not used because of insufficient data. Instead, the level of consciousness was graded as alert, drowsy, stupor, semicoma, and coma, and we found that the poor prognosis group had significantly lower levels of consciousness (P=0.003). The application of the GCS has limitations in children, especially in those younger than 36 months, so the pupillary reflex can be used to evaluate brain damage because it is useful for gauging brain stem function. We also found that the patients with no pupillary light reflex had high risk of poor prognosis (OR, 15.3; P=0.046).The Szpilman clinical score assesses drowning patients according to 4 clinical parameters, namely breathing, arterial pulse, pulmonary auscultation, and blood pressure5). These parameters showed a strong correlation with mortality in a previous study5,8). We classified the patients by using the Szpilman clinical score system and found that the poor prognosis groups had significantly higher Szpilman scores (P=0.007). In addition, the Szpilman clinical score was positively correlated with level of consciousness (r=0.489, P=0.002) and serum liver enzyme level (r=0.521, P=0.004). Thus, we can identify a more accurate prognosis by using the Szpilman clinical score system together with the level of consciousness.As we know, fast rescue and prompt resuscitation are the first step to improve the outcome in drowning and drowning children are commonly rescued by nonprofessional bystanders. Thus, the proper education for parents, caregivers, and other guardians is highly important. Education should cover not only the prevention of submersion accidents but also appropriate assessment and treatment of victims of drowning, and should be in consideration of the forementioned risk factors. In drowning patients, it is important that resuscitation follow the traditional airway-breathing-circulation sequence, because hypoxia is primary cause of cardiac arrest17). And rescue breathing should be initiated while still in the water, if possible.The limitation of this study was its small-scale retrospective design and inadequate patient data from old medical records. For more numerous, precise, and valid data, nationwide guidelines for drowning will be needed.In conclusion, we confirmed the several prognostic factors in drowning together with the Szpilman clinical score. In addition, the Szpilman clinical score system according to initial clinical parameters can be as useful as level of consciousness to predict mortality. Education for prevention, appropriate assessment, and prompt treatment of patients who have drowned should be in consideration of these risk factors.
- Conflicts of interest
Conflict of interest: No potential conflict of interest relevant to this article was reported.
- References
- 1. van Beeck EF, Branche CM, Szpilman D, Modell JH, Bierens JJ. A new definition of drowning: towards documentation and prevention of a global public health problem. Bull World Health Organ 2005;83:853–856.
[PubMed] [PMC]2. Nasrullah M, Muazzam S. Drowning mortality in the United States, 1999-2006. J Community Health 2011;36:69–75.
[Article] [PubMed]3. Korea National Statistical office. 2013 Cause-deleted life-table [Internet]. Daejeon: Statistics Korea, 2015;cited 2015 May 20. Available from: http://kostat.go.kr/portal/korea/kor_ko/5/2/index.board?bmode=read&aSeq=330389.4. Suominen PK, Vähätalo R. Neurologic long term outcome after drowning in children. Scand J Trauma Resusc Emerg Med 2012;20:55
[Article] [PubMed] [PMC]5. Szpilman D. Near-drowning and drowning classification: a proposal to stratify mortality based on the analysis of 1,831 cases. Chest 1997;112:660–665.
[Article] [PubMed]6. Zuckerman GB, Conway EE Jr. Drowning and near drowning: a pediatric epidemic. Pediatr Ann 2000;29:360–366.
[Article] [PubMed]7. Kim KS, Joung JI, Han MK, Kim BS, Park KY, Lee JJ, et al. Clinical aspects and prognostic factors of near drowning children. J Korean Child Neurol Soc 2003;11:322–327.8. Guzel A, Duran L, Paksu S, Akdemir HU, Paksu MS, Katı C, et al. Drowning and near-drowning: experience of a university hospital in the Black Sea region. Turk J Pediatr 2013;55:620–627.
[PubMed]9. Mosayebi Z, Movahedian AH, Mousavi GA. Drowning in children in Iran: outcomes and prognostic factors. Med J Malaysia 2011;66:187–190.
[PubMed]10. Brenner RA, Trumble AC, Smith GS, Kessler EP, Overpeck MD. Where children drown, United States, 1995. Pediatrics 2001;108:85–89.
[Article] [PubMed]11. Burford AE, Ryan LM, Stone BJ, Hirshon JM, Klein BL. Drowning and near-drowning in children and adolescents: a succinct review for emergency physicians and nurses. Pediatr Emerg Care 2005;21:610–616.
[Article] [PubMed]12. Idris AH, Berg RA, Bierens J, Bossaert L, Branche CM, Gabrielli A, et al. Recommended guidelines for uniform reporting of data from drowning: the "Utstein style". Circulation 2003;108:2565–2574.
[Article] [PubMed]13. Bruning C, Siekmeyer W, Siekmeyer M, Merkenschlager A, Kiess W. Retrospective analysis of 44 childhood drowning accidents. Wien Klin Wochenschr 2010;122:405–412.
[Article] [PubMed]14. Ballesteros MA, Gutierrez-Cuadra M, Munoz P, Miñambres E. Prognostic factors and outcome after drowning in an adult population. Acta Anaesthesiol Scand 2009;53:935–940.
[Article] [PubMed]15. Jung DB, Kim CH, Kim YB, Cho SH, Cho NS, Yang ES, et al. Analysis of predictive factors in the assessment of near-drowning in children. J Korean Soc Emerg Med 1998;9:437–434.16. Woo HO, Park CH. Childhood near-drowning in Chinju. J Korean Pediatr Soc 1997;40:1588–1595.
Table 1
Clinical characteristics and in-hospital patient status
Values are presented as mean±standard deviation or number.
*P<0.05. †Grade 1, normal pulmonary auscultation with coughing; grade 2, abnormal pulmonary auscultation with rales in some pulmonary fields; grade 3, pulmonary auscultation of acute pulmonary edema without arterial hypotension; grade 4, pulmonary auscultation of acute pulmonary edema with arterial hypotension; grade 5, isolated respiratory arrest; grade 6, cardiopulmonary arrest.
Table 2
Laboratory data of study participants
Table 3
Multivariate logistic regression values for predictors of clinical prognosis

 About
About Browse articles
Browse articles For contributors
For contributors