All issues > Volume 59(7); 2016
Dietary habits and gastroesophageal reflux disease in preschool children
- Corresponding author: Su Jin Jeong, MD. Department of Pediatrics, Bundang CHA Medical Center, CHA University School of Medicine, 59 Yatap-ro, Bundang-gu, Seongnam 13496, Korea. Tel: +82-31-780-5230, Fax: +82-31-780-5239, jinped@cha.ac.kr
- Received February 05, 2016 Revised May 01, 2016 Accepted May 04, 2016
- Abstract
-
- Purpose
- Purpose
- To identify the relationship between dietary habits and childhood gastroesophageal reflux disease (GERD) in preschool children.
- Methods
- Methods
- We performed a questionnaire study to analyze the relationship between dietary habits and GERD in 85 preschool children with GERD and 117 healthy children of the same age.
- Results
- Results
- Irregular and picky eating were more p–revalent in the GERD group than in the control group (odds ratio [OR], 4.14; 95% confidence interval [CI], 1.37–12.54 and OR, 4.96; 95% CI, 1.88–13.14, respectively). The snack preferences and the late night eating habits were significantly more prevalent in the GERD group than in the control group (OR, 3.83; 95% CI, 1.23–11.87 and OR, 9.51; 95% CI, 2.55–35.49, respectively). A preference for liquid foods was significantly more prevalent in the GERD group (OR, 9.51; 95% CI, 2.548–35.485). The dinner-to-bedtime interval was significantly shorter in the GERD group than in the control group (157.06±48.47 vs. 174.62±55.10, P=0.020). In addition, the time between dinner and bedtime was shorter than 3 hours in 47 children (55.3%) of the GERD group and 44 (37.6%) of the control group. This difference was statistical significance (P=0.015).
- Conclusion
- Conclusion
- Dietary habits such as picky and irregular eating, snack preference, a preference of liquid foods, late night eating, and a shorter dinner-to-bedtime interval had a significant correlation with GERD. Further large-scale studies are necessary to confirm our results.
- Introduction
- Introduction
Gastroesophageal reflux disease (GERD) is a chronic condition that occurs the most commonly in children of all ages1,2,3). Although the clinical course of childhood GERD is unclear, previous studies have shown that childhood GERD is a significant risk factor of GERD in adolescents and young adults1,4,5). To date, however, few clinical studies have clarified risk factors of developing childhood GERD in a pediatric population6). There are a few well known risk factors of GERD that included neurologic disorders, congenital malformation and severe chronic pulmonary disorders during childhood4,6).Treatment modalities for childhood GERD include pharmacological treatments (e.g., proton pump inhibitors, antacids, H-2 blockers, and prokinetics), antireflux endoluminal therapies, fundoplication surgery and lifestyle modification7,8). But there is a possibility that children with GERD are vulnerable to relapse even after the treatment unless risk factors are removed, in contrast with infantile gastroesophageal reflux that spontaneously resolves without treatments by the second year of life4). Moreover, pharmacological treatments are not effective in completely treating long-term complications. It is therefore imperative that childhood GERD be prevented before its progression to adolescent or adult cases6,9).Childhood GERD may be influenced by numerous lifestyle factors4), there particularly include dietary habits that may strongly affect, other lifestyle factors after being settled during childhood. Also wrong dietary habits such as preference of snack or drink contribute to overweight or obesity that impact as risk factor of GERD in adulthood10,11). We have therefore speculated that childhood GERD would be prevented if there are efforts to correct wrong dietary habits considering that there is a possible relationship between children's dietary habit and childhood1). Given the above background, we conducted this case-control study to identify the relationship between dietary habits and childhood GERD in preschool children.
- Materials and methods
- Materials and methods
- 1. Study design
- 1. Study design
Between January 1, 2010 and December 31, 2013, 101 preschool children (between 3 and 6 years old) were diagnosed as GERD through esophagogastroduodenoscopy (EGD), or esophageal pH or multichannel intraluminal impedance test (n=20)11,12). The endoscopic assessment of esophageal change was performed according to the Los Angeles (LA) classification for endoscopic grading of esophagitis: grade A, one (or more) mucosal break no longer than 5 mm, that dose not extend between the tops of 2 mucosal folds; grade B, 1 (or more) mucosal break more than 5 mm long, that dose not extend between the tops of 2 mucosal folds; grade C, 1 (or more) mucosal break that is continuous between the tops of two or more mucosal folds but which involves less than 75% of the circumference; grade D, 1 (or more) mucosal break which involves at least 75% of the esophageal circumference13), and patients who had GERD with class A to D of LA classification were included (n=81). Data from esophageal pH or multichannel intraluminal impedence test was interpreted by the symptom association probability (SAP) that is the statistical relation between reflux and symptoms by Fisher extract test or reflux index (RI [% time pH<4]), and a SAP>95% or an RI>7% is considered positive14,15). We excluded patients with concurrently gastrointestinal diseases (e.g., gastric or duodenal ulcer, Helicobacter pylori infection, and eosinophilic esophagitis), food allergy, congenital problem, severe chronic health conditions (e.g., epilepsy, growth failure, allergic disease, or chronic lung problem such as bronchopulomary dysplasia or tracheomalacia).We therefore enrolled a total of 85 preschool children with GERD in the current study and then assigned them to the GERD group (n=85). Among 85 children, 74 of them were diagnosed through EGD (LA class A=61, B=11, and C=2), 11 through esophageal pH metry (n=5) or multichannel intraluminal impedence test (n=6). In addition, we also evaluated 117 healthy preschool children who visited us for a regular medical check-up in Korea national health screening program during the same period by physical examination and questionnaire and then assigned them to the control group. Children who were assessed to have gastrointestinal or respiratory symptoms or signs of GERD were excluded in control group. The children with GERD or healthy controls submitted a written informed consent that was waived due to the retrospective nature for the current study.- 2. Questionnaire study
- 2. Questionnaire study
We performed a questionnaire study to examine demographic characteristics (e.g., age and body mass index [BMI], dietary habits and sleep habits). Our questionnaire was based on a nutrition questionnaire and guidelines for the Korea national health screening program for infants and children that were developed by Korean national health insurance cooperation, and customized for preschool children16).- 3. Statistical analysis
- 3. Statistical analysis
We analyzed the data using the chi-square test and independent t test. Moreover, we also performed a multivariate logistic regression analysis to compare the data between the 2 groups. All continuous variables were expressed as mean±standard deviation (SD).BMI was calculated as weight in kilograms divided by height in square meters (kg/m2) and BMI percentile for age was assessed using the Center for Disease Control growth charts17). Overweight and obesity were defined as a BMI at or above the 85th percentile and below the 95th percentile and at or above 95th percentile for children of the same age and sex. A P value of <0.05 was considered statistically significant. Statistical analysis was performed using the IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). The current study was approved by the Institutional Review Board of Bundang CHA medical center (approval number: BD2014-200). Written informed consent was obtained from all subjects.
- Results
- Results
- 1. Baseline characteristics
- 1. Baseline characteristics
In the current study, we enrolled a total of 202 preschool children (104 boys [51.4%] and 98 girls [48.6%]). Baseline characteristics of the subjects are represented in Table 1. The mean age was 5.01±1.02 years in the GERD group and 4.09±0.98 years in the control group, and this difference reached statistical significance (P<0.001; odds ratio [OR], 1.13; 95% confidence interval [CI], 1.076–1.18, respectively). There was no significant difference in the male-to-female ratio and BMI percentile for age between the 2 groups. Moreover, appetite and the frequency of meal were significantly less prevalent and lower, respectively, in the GERD group as compared with the control group (P<0.001).As shown in Table 2, irregular eating and picky eating were more prevalent in the GERD group as compared with the control group (OR, 4.14; 95% CI, 1.37–12.54 and OR, 4.96; 95% CI, 1.88–13.14, respectively). But these trends were not seen for fatty food (P=0.127). The snack preference and the late night eating habit were significantly more prevalent in the GERD group as compared with the control group (OR, 3.83; 95% CI, 1.23–11.87 and OR, 9.51; 95% CI, 2.55–35.49, respectively). A multivariate analysis showed that a preference of liquid foods, such as milk product or sweet beverage was significantly more prevalent in the GERD group (OR, 9.51; 95% CI, 2.548–35.485). But these trends were not seen for the total amount of liquid or solid foods.- 2. Correlation between the amount or speed of eating and GERD
- 2. Correlation between the amount or speed of eating and GERD
There was no significant correlation between the small amount of eating and GERD. With regards to the length of meal time, the number of the children who responded that it was longer than 30 minutes was 18 (21.2%) in the GERD group and 1 (0.9%) in control group. There was a significant correlation between the length of meal time and GERD (P<0.001).- 3. Correlation between dietary habits and GERD
- 3. Correlation between dietary habits and GERD
The dinner-to-bedtime interval was shorter in the GERD group as compared with the control group (157.06±48.47 vs. 174.62±55.10, P=0.020). In addition, as shown in Fig. 1, the number of the children with a dinner-to-bedtime of shorter than 3 hours was 47 (55.3%) in the GERD group and 44 (37.6%) in the control group. This difference reached statistical significance (P=0.015).
- Discussion
- Discussion
This is the first study to examine the relationship between dietary habits and GERD in preschool children. Although many studies have been conducted in this series, there is a paucity of data regarding the above relationship4,6). Our results showed that GERD had a significant correlation with irregular and picky eating, the small amount of eating, snack preference, a preference of liquid foods and a shorter dinner-to-bedtime interval in preschool children.Previous adult studies have shown that risk factors of developing GERD include Caucasian race, male sex, obesity or overweight, H. pylori infection and lifestyle factors (e.g., smoking, alcohol, dietary fat or drugs such as nonsteroidal antiinflammatory drugs)11,18,19,20,21). Our results showed that the age was one of the risk factors of developing GERD (OR, 1.13; 95% CI, 1.076–1.18), which is consistent with studies in older children or adults10,20). But male sex and BMI were not risk factors of developing GERD. With regards to the BMI, it had a significant correlation with GERD. In this study, however there were no significant differences in BMI percentile for age and the number of overweight or obese children between our GERD and healthy preschool children. Presumably, this might be because there is no great sex-related variability in lifestyle and environmental factors, such as smoking or drinking, in children as compared with adults, furthermore BMI usually decreases during preschool period and increases into adulthood17). In more detail, obese adult men are at increased risks of developing GERD possibly due to wrong dietary habits during preschool days and a frequent exposure to smoking or drinking20).Despite many previous reports in this series, our results showed that overeating or fat intake were not risk factors of developing GERD in preschool children. In the current study, food refusal or anorexia rather than overeating were risk factors of developing GERD (P<0.001 vs. P=0.317). In addition, irregular eating and a prolonged meal time were more prevalent in the GERD group as compared with the control group. It is unclear, however, whether these findings are risk factors of developing GERD or its outcomes; an irregular, prolonged meal intake might induce the reflux of gastric juice and thereby cause a prolonged duration of gastric acid secretion and a shortened gastric emptying time22,23).There was a significant correlation between snack preference and GERD. Picky eating had a significant correlation with GERD. It is noteworthy that there was a larger number of the children who preferred milk product or sweet beverage to solid foods. It is generally known that it takes 12–24 months for childhood GERD to disappear in up to 95% of total cases2). By that time, infants undergo maturation of gastrointestinal tract and begin to wean and to eat solid foods3). Moreover, by the preschool age, children form dietary habits with the switch from liquid to solid foods10,24). Consequently, the preschool age of 3–6 years old is a period characterized by the lowest prevalence of GERD across all ages6). Until that time, however, liquid foods would lead to the increased occurrence of GERD.With regards to late night eating habits, there was a significant correlation between late night eating habits and GERD; the children with GERD had a shorter dinner-to-bedtime as compared with the control group. Recent adult studies have shown that a short dinner-to-bedtime had a significant correlation with not only occurrence but also recurrence of GERD7,19). In association with this, according to the guidelines from the American College of Gastroenterology, it is recommended that the dinner-to-bedtime interval be longer than three hours25). This is consistent with our results.There are several limitations of the current study. First, we failed to consider objective criteria for determining dietary habits. In addition, there might be a bias arising from the caregivers. Next, in the current study, we enrolled a relatively smaller number of the children. Finally we assigned the healthy children who visited us for a general health check-up. We cannot therefore completely rule out the possibility that we might have assigned the children with asymptomatic GERD to the control group.Our results showed that dietary habits, such as picky and irregular eating, snack preference, a preference of liquid foods, late night eating habit and a shorter dinner-to-bedtime interval, had a significant correlation with GERD. But further large-scale studies are warranted to establish our results. Therefore, in order to decrease the likelihood of GERD progressing to persistent GERD or Barrett's esophagus, caregivers of preschoolers should refrain from providing late-night snack; should provide a balance of solid and liquid foods; and should maintain a satisfactory time interval of at least three hours from dinner to bedtime.
- Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
- References
- 1. Gupta SK, Hassall E, Chiu YL, Amer F, Heyman MB. Presenting symptoms of nonerosive and erosive esophagitis in pediatric patients. Dig Dis Sci 2006;51:858–863.
[Article] [PubMed]2. Forbes D. Mewling and puking: infantile gastroesophageal reflux in the 21st century. J Paediatr Child Health 2013;49:259–263.
[Article] [PubMed]3. Nelson SP, Chen EH, Syniar GM, Christoffel KK. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med 1997;151:569–572.
[Article] [PubMed]4. El-Serag HB, Gilger M, Carter J, Genta RM, Rabeneck L. Childhood GERD is a risk factor for GERD in adolescents and young adults. Am J Gastroenterol 2004;99:806–812.
[Article] [PubMed]5. Eisen GM, Sandler RS, Murray S, Gottfried M. The relationship between gastroesophageal reflux disease and its complications with Barrett's esophagus. Am J Gastroenterol 1997;92:27–31.
[PubMed]6. Gilger MA, El-Serag HB, Gold BD, Dietrich CL, Tsou V, McDuffie A, et al. Prevalence of endoscopic findings of erosive esophagitis in children: a population-based study. J Pediatr Gastroenterol Nutr 2008;47:141–146.
[Article] [PubMed]7. Fujiwara Y, Machida A, Watanabe Y, Shiba M, Tominaga K, Watanabe T, et al. Association between dinner-to-bed time and gastro-esophageal reflux disease. Am J Gastroenterol 2005;100:2633–2636.
[Article] [PubMed]8. Lee JH, Kim MJ, Lee JS, Choe YH. The effects of three alternative treatment strategies after 8 weeks of proton pump inhibitor therapy for GERD in children. Arch Dis Child 2011;96:9–13.
[Article] [PubMed]9. Rudolph CD, Mazur LJ, Liptak GS, Baker RD, Boyle JT, Colletti RB, et al. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr 2001;32(Suppl 2): S1–S31.10. Nicklas T, Johnson R. American Dietetic Association. Position of the American Dietetic Association: dietary guidance for healthy children ages 2 to 11 years. J Am Diet Assoc 2004;104:660–677.
[Article] [PubMed]11. Kim N, Lee SW, Cho SI, Park CG, Yang CH, Kim HS, et al. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther 2008;27:173–185.
[Article] [PubMed]12. Sherman PM, Hassall E, Fagundes-Neto U, Gold BD, Kato S, Koletzko S, et al. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Arch Pediatr 2010;17:1586–1593.
[Article] [PubMed]13. Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 1999;45:172–180.
[Article] [PubMed] [PMC]14. Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr 2009;49:498–547.
[Article] [PubMed]15. Weusten BL, Roelofs JM, Akkermans LM, Van Berge-Henegouwen GP, Smout AJ. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology 1994;107:1741–1745.
[Article] [PubMed]16. Moon JS, Kim JY, Chang SH, Hae CK, Yang HR, Seo JK, et al. Development of a nutrition questionnaire and guidelines for the Korea National Health Screening Program for Infants and Children. Korean J Pediatr Gastroenterol Nutr 2008;11:42–55.
[Article]17. Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002;(246): 1–190.18. Nocon M, Labenz J, Willich SN. Lifestyle factors and symptoms of gastro-oesophageal reflux: a population-based study. Aliment Pharmacol Ther 2006;23:169–174.
[Article] [PubMed]19. Yang JH, Kang HS, Lee SY, Kim JH, Sung IK, Park HS, et al. Recurrence of gastroesophageal reflux disease correlated with a short dinner-to-bedtime interval. J Gastroenterol Hepatol 2014;29:730–735.
[Article] [PubMed]20. Dore MP, Maragkoudakis E, Fraley K, Pedroni A, Tadeu V, Realdi G, et al. Diet, lifestyle and gender in gastro-esophageal reflux disease. Dig Dis Sci 2008;53:2027–2032.
[Article] [PubMed]21. Robertson EV, Derakhshan MH, Wirz AA, Lee YY, Seenan JP, Ballantyne SA, et al. Central obesity in asymptomatic volunteers is associated with increased intrasphincteric acid reflux and lengthening of the cardiac mucosa. Gastroenterology 2013;145:730–739.
[Article] [PubMed]22. Caldaro T, Garganese MC, Torroni F, Ciofetta G, De Angelis P, di Abriola GF, et al. Delayed gastric emptying and typical scintigraphic gastric curves in children with gastroesophageal reflux disease: could pyloromyotomy improve this condition? J Pediatr Surg 2011;46:863–869.
[Article] [PubMed]23. Estevão-Costa J, Campos M, Dias JA, Trindade E, Medina AM, Carvalho JL. Delayed gastric emptying and gastroesophageal reflux: a pathophysiologic relationship. J Pediatr Gastroenterol Nutr 2001;32:471–474.
[Article] [PubMed]
Fig. 1
Percentage of children whose dinner-to-bed time was more or less than 3 hours when comparing gastroesophageal reflux disease (GERD) and control groups. In GERD patients, 55.3% of patients went to bed within 3 hours after dinner (n=47), compared with 37.6% in the control group (n=44).
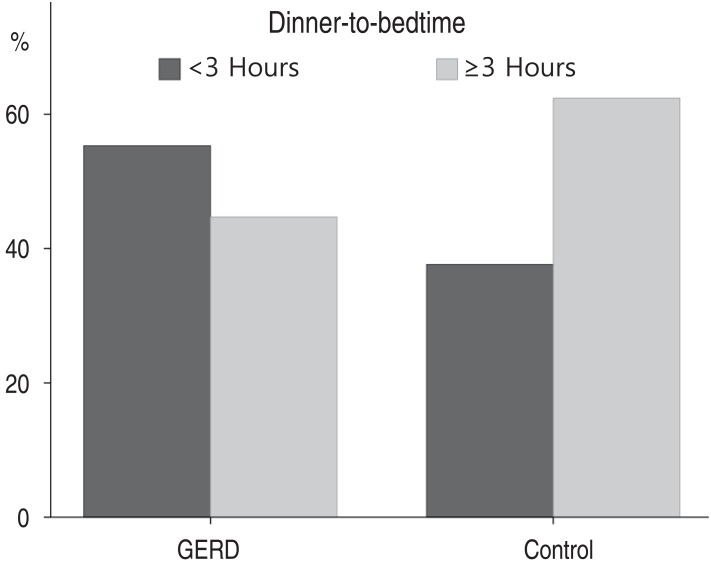
Table 1
Baseline characteristics of pediatric GERD patients in preschool
Table 2
Relationship between dietary habits and gastroesophageal reflux disease

 About
About Browse articles
Browse articles For contributors
For contributors
