All issues > Volume 60(5); 2017
Prognostic factors and treatment of pediatric acute lymphoblastic leukemia
- Corresponding author: Bin Cho, MD, PhD. Department of Pediatrics, Seoul St. Mary's Hospital, The Catholic University of Korea, College of Medicine, 222 Banpo-daero, Seocho-gu, Seoul 06591, Korea. Tel: +82-2-2258-6187, Fax: +82-2-537-4544, chobinkr@catholic.ac.kr
- Received February 16, 2017 Revised March 30, 2017 Accepted April 11, 2017
- Abstract
-
The event-free survival (EFS) for pediatric acute lymphoblastic leukemia (ALL) has shown remarkable improvement in the past several decades. In Korea also, a recent study showed 10-year EFS of 78.5%. Much of the improved outcome for pediatric ALL stems from the accurate identification of prognostic factors, the designation of risk group based on these factors, and treatment of appropriate duration and intensity according to risk group, done within the setting of cooperative clinical trials. The schema of first-line therapy for ALL remains mostly unchanged, although many groups have now reported on the elimination of cranial irradiation in all patients with low rates of central nervous system relapse. Specific high risk subgroups, such as Philadelphia chromosome-positive (Ph+) ALL and infant ALL continue to have significantly lower survival than other ALL patients. The introduction of tyrosine kinase inhibitors into therapy has led to enhanced outcome for Ph+ ALL patients. Infant ALL patients, particularly those with MLL rearrangements, continue to have poor outcome, despite treatment intensification including allogeneic hematopoietic cell transplantation. Relapsed ALL is a leading cause of mortality in pediatric cancer. Recent advances in immunotherapy targeting the CD19 of the ALL blast have shown remarkable efficacy in some of these relapsed and refractory patients. With improved survival, much of the current focus is on decreasing the long-term toxicities of treatment.
- Introduction
- Introduction
Acute lymphoblastic leukemia (ALL) is the most common cancer in the pediatric age group and is responsible for the most cancer-related deaths in children and adolescents. In Korea, the age-standardized incidence rate of ALL is approximately 28 patients per million in the 0–14 year old age group1). Whereas 50 years ago the survival for pediatric ALL was 10%–20%2), currently long-term overall survival (OS) rates are 80%–90%3,4,5). In Korea also, we reported a 10-year event-free survival (EFS) of 78.5% and OS of 81.9% for a large number of patients treated on CMCP-ALLL2005 and -ALL2008 regimens6). Much of the improvement in survival stems from the classification of patients into risk groups based on prognostic factors, and the adjustment of treatment intensity according to risk group, within the setting of national and multinational clinical trials. Current focus is on further understanding the biology of the disease and developing novel therapeutics in order to salvage patients who relapse or remain refractory to first-line treatment, as well as on minimizing the long-term adverse effects of chemotherapy.
- Prognostic factors
- Prognostic factors
- 1. Age and WBC count
- 1. Age and WBC count
In precursor B cell (Pre-B) ALL, patient age at diagnosis and presenting WBC count are independent prognostic factors. Patients diagnosed between the ages of 1 and 10 have a superior outcome compared with those <1 year old or ≥10 years old. Infant ALL is particularly known to have poor survival with a 4-year EFS of 47% according to a multinational study7). High WBC count at diagnosis is also an adverse factor, with patients presenting with WBC count≥50,000/mm3 having worse outcome. Age and WBC count at diagnosis are combined in the categorization of clinical risk group according to National Cancer Institute/Rome criteria, with patients between the ages of 1 and 9.99 years and having a WBC count<50,000/mm3 termed ‘standard risk,’ while the remainder are considered ‘high risk’8). In contrast to patients with Pre-B ALL, age and WBC count have less of a role in determining prognosis in patients with T cell ALL (T-ALL).- 2. Immunophenotype
- 2. Immunophenotype
The 10%–15% of patients with T-ALL had previously been considered to have worse outcome than those with Pre-B ALL. However, survival is now similar between the 2 patient groups with appropriate treatment intensification of T-ALL patients9).- 3. Genetic factors
- 3. Genetic factors
Genetic abnormalities of the leukemic blast, including aneuploidy and recurrent translocations and deletions, are important factors in the determination of risk group and outcome in Pre-B ALL. Those that predict excellent prognosis include ETV6-RUNX1 (t(12;21)(p13;q22)) and high hyperdiploidy, that is a chromosome number ≥5110,11). However, even within this favorable outcome subgroup, patients with detectable minimal residual disease (MRD) at the end of remission induction may have significantly lower survival than those who are MRD(-)12). In our institution, we found that ETV6-RUNX1(+) ALL patients who were MRD(+) at the end of remission induction had EFS of 33%, in contrast to the 91% EFS for those who were MRD(-)13).Recurrent genetic abnormalities associated with poor prognosis include BCR-ABL1 (t(9;22)(q34;q11.2)), that is Philadelphia chromosome-positive (Ph+) ALL, rearrangements of MLL (or KMT2A)(11q23), and hypodiploidy. MLL rearrangements are found in about 75% of infant ALL patients and predict a dismal outcome for this group of patients. Most patients with hypodiploid ALL have 45 chromosomes and their outcome has been reported to be similar to those with nonhypodiploid ALL14). In contrast, hypodiploid ALL patients with ≤44 chromosomes, including those with low hypodiploidy (32–39 chromosomes) and near haploidy (24–31 chromosomes), have significantly worse survival15). A recent study found that 91.2% patients with low hypodiploidy have TP53 mutations, many of whom also showed the mutations in nontumor cells, indicating that ALL patients with low hypodiploidy may have underlying Li-Fraumeni syndrome16). Hence, testing for TP53 mutations in patients with low hypodiploidy may allow for genetic counseling for those with germline mutations.Patients with E2A-PBX1 (t(1;19)(q23;p13.3)) had previously been considered to have poor prognosis. However, patients treated on intensive, contemporary therapy were found to have favorable outcome17), and this genetic abnormality is no longer deemed a risk factor by several treatment groups. In contrast, the rare patients with E2A-HLF (t(17;19)(q22;p13.3) rearrangement have extremely poor outcome18). Intrachromosomal amplification of chromosome 21 (iAMP21) is most often diagnosed by fluorescence in situ hybridization (FISH) for the RUNX1 gene, showing five or more signals per cell in total. Patients with iAMP21 were initially deemed to have unfavorable outcome, as evidenced by the five year EFS of 29% found in one study19). However, treatment of this group of patients with high risk therapy negates the low survival associated with this genetic abnormality20).Advances in next generation sequencing technology, including whole genome and whole exome sequencing, have aided in the identification of genetic abnormalities with prognostic relevance. One of the most critical abnormalities detected through these methods has been alteration of IKZF1, the gene for the lymphoid transcription factor IKAROS. A seminal study found IKZF1 deletion in 29% of high risk ALL patients, and confirmed that it was an independent prognostic factor for poor outcome21). Alterations of IKZF1 were frequent in patients with Ph+ ALL, as well as high risk patients with a mutational spectrum similar to that of Ph+ ALL but without the BCR-ABL1 translocation, that is Ph-like ALL. This disease subtype is known for abnormalities in kinase and cytokine receptor genes, and can be divided into those with ABL1-class rearrangements, including ABL1, ABL2, CSF1R and PDGFRB rearrangements, and those that activate JAK-STAT signaling, including JAK2, CRLF2 and EPOR rearrangements. Identification of these abnormalities is important as some of them respond to targeted therapy, with ABL1-class rearrangements responding to tyrosine kinase inhibitors (TKI) such as imatinib and dasatinib, and those with aberrant JAK-STAT signaling responding to JAK inhibitors such as ruxolitinib22). Although a simple and comprehensive method for the evaluation of these genetic abnormalities in the clinical setting is not yet readily available, some rearrangements, such as those of PDGFRB, can be detected through FISH, allowing for the identification of refractory patients who may be salvaged by TKI treatment23,24).The prognostic relevance of genetic abnormalities in T-ALL remains mostly unclear. In terms of incidence, NOTCH1 mutations are important, with over 50% of T-cell ALL patients harboring activating mutations of NOTCH125). An important subtype of T-ALL is early T-cell precursor (ETP)-ALL, characterized by an immature phenotype of CD1a (-), CD8 (-), CD5 weak, and expression of one or more myeloid or stem cell markers. The presence of FMS-like tyrosine kinase 3 (FLT3) mutations may also aid in the diagnosis of ETP-ALL. The initial study on this subtype indicated that patients with ETP-ALL had significantly worse outcome compared with other T-ALL patients26). However, ETP-ALL patients treated on UKALL 2003 had a nonsignificantly lower EFS and OS compared with other T-ALL patients27). Another study found that although ETP-ALL patients had an inferior response to initial therapy, as measured by prednisone response after one week of treatment and MRD levels, they had favorable survival, indicating that ETP status was not an independent prognostic factor when evaluated within the context of proven variables such as MRD status28). However, it is important to note that 18 of 49 patients received hematopoietic cell transplantation (HCT) in first complete remission (CR) in this study. Overall, the significance of the ETP phenotype remains unclear. However, intensive therapy including allogeneic transplant may be considered for patients who show a poor response to remission induction therapy.- 4. Response to treatment
- 4. Response to treatment
Early response to treatment may be measured by the clearance of peripheral blasts after one week of prophase steroid, which may be utilized in risk group assignment. Those with a good response to steroid, that is a peripheral blast count <1,000/mm3, have better survival compared with those with a poor response to steroid (a peripheral blast count ≥1,000/mm3)29).MRD remains the most important prognostic factor in pediatric ALL. Current methods of measuring MRD include polymerase chain reaction (PCR) for immunoglobulin (Ig)/T-cell receptor (TCR) rearrangements, flow cytometry to detect aberrant immunophenotypes, and PCR for recurrent genetic fusions such as real-time quantitative (RQ)-PCR for BCR-ABL1. Both measurement of PCR for Ig/TCR and flow cytometry have been accurate in determining post-treatment MRD30,31), with a cutoff level of >0.01% at end of induction according to flow cytometry based MRD predicting patients with significantly lower EFS12). Studies utilizing Ig/TCR PCR have also shown that MRD checked at both end of induction as well as end of consolidation is able to determine patients with significant residual disease and, hence, worse outcome32,33).
Well-established prognostic variables include patient factors such as age, initial presenting white blood cell (WBC) count, the genetic and immunophenotypic characteristics of the leukemic blast, and individual response to therapy.
- Outline of treatment
- Outline of treatment
- 1. Remission induction
- 1. Remission induction
Initial therapy consists of about 4 weeks of remission induction during which steroid (prednisolone or dexamethasone), vincristine, asparaginase, and intrathecal chemotherapy are given. An anthracycline, such as daunorubicin, may be administered to patients deemed high risk at diagnosis. The first intrathecal therapy, often consisting of triple therapy of methotrexate (MTX), cytarabine and hydrocortisone, is given immediately after diagnosis. This initial treatment, done to diagnose and treat central nervous system (CNS) leukemia as well as for CNS prophylaxis, is crucial to the long-term outcome of the patient as a traumatic lumbar puncture (TLP) at this step results in a greater incidence of relapse34). TLP may result in circulating leukemic blasts seeding the CNS and may also confound the diagnosis of initial CNS involvement. One study showed that delaying the initial intrathecal therapy for up to 1 week decreased the rate of TLP without adversely affecting long-term outcome35). Hence, a delay of the initial intrathecal chemotherapy for a maximum of 1 week may be considered in patients who are at high risk of experiencing TLP, such as patients with extreme hyperleukocytosis or obese adolescents with a significant number of peripheral blasts. After intrathecal administration, maintaining the patient in a prone position for one hour may increase the drug concentration in ventricular cerebrospinal fluid (CSF)36).Asparaginase toxicity is a major impediment to chemotherapy schedule adherence, especially for adolescent patients. Aside from drug hypersensitivity, major side effects include pancreatitis, hyperglycemia, hypertriglyceridemia, coagulopathy, and thrombosis. Besides patients who show clear toxicity, drug efficacy may be compromised in asymptomatic patients due to silent inactivation37). For patients who show hypersensitivity to native Escherichia coli asparaginase, switching to the pegylated form, or a different strain such as Erwinia asparaginase, may allow for continuation of asparaginase therapy.- 2. Consolidation and Intensification
- 2. Consolidation and Intensification
After remission induction, each patient should be classified into a risk group indicating the overall risk for relapse, based on the prognostic factors at diagnosis, and response to initial therapy, including prophase steroid response and MRD at the end of remission induction (Table 1). These risk groups predict survival, with low and standard risk groups having excellent EFS, while high risk patients have a more guarded prognosis (Fig. 1). The majority of patients will achieve CR after remission induction, subsequent to which all patients receive six months to one year of consolidation and intensification treatment, the duration and intensity of which depends on the patient risk group.The consolidation phase is marked by continued CNS prophylaxis. In the past, CNS treatment was done mostly with cranial irradiation. However, the long-term neurologic and endocrine complications associated with this method of treatment have led to the omission of cranial irradiation for the majority of patients. Instead, CNS treatment for most patients consists of intensive intrathecal and systemic therapy incorporating agents such as high dose MTX38). Several studies have reported on the elimination of cranial irradiation for all patients in first CR, even for those with CNS involvement5,39). At our institution, we have also treated all patients in first CR without cranial irradiation regardless of initial CNS status, resulting in a cumulative incidence of any CNS relapse of 2.3%6).Afterwards, patients receive an 8-week delayed intensification phase of treatment which utilizes drugs that were used in both remission induction and consolidation. The overall risk group of the patient is important in determining the number of intensification courses administered, with standard risk patients receiving one course of treatment to minimize toxicity40), while those with high risk features benefit from two courses of intensification41).- 3. Maintenance therapy
- 3. Maintenance therapy
The final phase of treatment is maintenance therapy which on average takes about 2 years for completion. The key component of this phase is antimetabolite therapy, including daily oral mercaptopurine and weekly oral MTX. Some institutions add pulses of vincristine and steroid every 4 weeks to this regimen. CNS prophylaxis should continue during maintenance therapy. As this period of treatment is prolonged and requires daily intake of medication, patient compliance is a critical issue, especially for adolescent patients. Patient noncompliance and high variability of metabolite levels within each patient, caused by varying drug doses and periods of treatment interruption, may result in an increased risk of relapse42). Patients should also continue to adhere to the Bactrim regimen of each institution, as failure to do so may result in Pneumocystis jiroveci pneumonia during this period.- 4. Allogeneic HCT in first CR
- 4. Allogeneic HCT in first CR
The number of patients receiving HCT in first CR is decreasing, with recent studies showing 1.2%–6.6% of patients treated with upfront HCT5,29). An important indication for allogeneic HCT in first CR would be the small number of patients who fail to achieve CR after the first attempt at remission induction. A multinational study of 1,041 patients with induction failure showed that allogeneic HCT improved outcomes in T-ALL patients43). The strategy at our institution is to undertake HCT in first CR for patients with induction failure, BCR-ABL1 (+) ALL, hypodiploid ALL, and infant ALL with MLL rearrangement if they have a human leukocyte antigen well-matched donor.
- Treatment of specific subgroups
- Treatment of specific subgroups
- 1. Ph+ ALL
- 1. Ph+ ALL
A study of a large number of patients enrolled in the UK Medical Research Council ALL97/99 trial showed a Ph+ ALL incidence of 3%11). Prior to TKI therapy, the mainstay of treatment was conventional chemotherapy combined with HCT, despite which outcome was extremely unfavorable44). The Children's Oncology Group (COG) AALL0031 trial incorporated imatinib at 340 mg/m2/day postinduction and found that continuous dosing of imatinib resulted in 5-year EFS rates comparable to those of patients who received either sibling or alternative donor bone marrow transplant45). In the EsPhALL study, based on intermittent imatinib dosing, the advantage of imatinib added to chemotherapy was less clear46). However, the study further confirmed that imatinib could safely be added to chemotherapy to improve outcomes of pediatric Ph+ ALL patients. Another study from the Spanish Cooperative Group showed that imatinib and chemotherapy followed by HCT significantly improved survival compared with historical controls47).Despite major improvement in survival, Ph+ ALL remains a very high risk subtype of ALL with increased risk of relapse either with or without transplant. Although the results of the COG study provide evidence that HCT may not be necessary in first CR for Ph+ ALL patients, further follow-up on a larger number of patients is necessary to clarify this issue. Data from adult patients show that MRD, as measured by RQ-PCR for BCR-ABL1 during the early period of treatment, may identify patients at high risk of treatment failure48). Screening for BCR-ABL1 kinase domain mutations at relapse may identify patients who develop mutations that confer resistance to imatinib49). Finally, the follow-up period for pediatric Ph+ ALL patients treated with imatinib has been relatively short, and the long-term adverse effects of prolonged TKI treatment require further study. The deleterious impact of imatinib on bone growth, as has been observed in patients with chronic myeloid leukemia, is of particular concern for the pediatric population50).- 2. Infant ALL
- 2. Infant ALL
Infant ALL continues to have dismal outcome despite chemotherapy intensification and treatment with HCT. Cooperative studies showed long-term EFS of less than 50%7,51). Important prognostic factors found in these studies include the presence of MLL rearrangement, hyperleukocytosis, age less than three to six months, and poor response to prednisone prophase as having a clear adverse impact on outcome. Whether allogeneic HCT in first CR improves survival is less clear. One study showed that high risk patients with MLL rearrangements who were treated with HCT in first CR showed EFS of less than 50%52). However, data from the Interfant-99 study showed that MLL rearranged infant ALL patients had significantly better survival when treated with HCT in first CR, although patients who benefited from HCT had other poor prognosis features such as younger age, poor response to steroids, and hyperleukocytosis53). At our institution, most infant ALL patients were treated without HCT in first CR, resulting in EFS of less than 40%6). This extremely poor outcome led to a revision of treatment strategy and we currently undertake HCT in first CR for infant ALL patients with MLL rearrangement. Despite the potential benefit of HCT, infants are highly susceptible to the long-term effects of HCT on growth, development and cognition, underscoring the need for close follow-up of these parameters.Infants without MLL rearrangement tend to be older than those with this genetic abnormality and have a more favorable outcome54). Hence, these patients may be treated with high risk chemotherapy while avoiding HCT in first CR.- 3. Adolescents and young adults
- 3. Adolescents and young adults
Patients aged 15 and above face special issues compared with other ALL patients. Depending on the medical department to which they are transferred for care, these patients may be treated under high risk pediatric ALL protocols, or may be given chemotherapy commonly administered by adult hematologists. Although this age group may be more susceptible to the side effects of chemotherapy than younger patients, several studies have shown superior EFS compared with historical controls with acceptable toxicity when treated with pediatric regimens55). Important toxicities that are more pertinent to adolescents include steroid-related osteonecrosis, the incidence of which is significantly higher in teenagers compared with children56). Checking for medication compliance in adolescents is critical for optimal outcome, as data suggest that a significant portion of adolescent patients have difficulties in adhering to treatment schedule57).- 4. ALL patients with Down syndrome
- 4. ALL patients with Down syndrome
Children with Down Syndrome (DS) have a 20 fold greater risk for ALL compared with non-DS children58). Important aspects of the molecular pathogenesis of DS-ALL include CRLF2 overexpression, found in the majority of DS-ALL patients, and JAK2 mutations resulting in aberrant JAK-STAT signaling59). Outcome in DS-ALL patients is lower than in other ALL patients due to both increased rates of relapse and treatment-related mortality60). With regard to chemotherapy side effects, DS-ALL patients are more likely to develop MTX-induced toxicity, especially gastrointestinal toxicity, necessitating dose reductions of high dose MTX therapy61).
- Relapsed ALL
- Relapsed ALL
- 1. Blinatumomab
- 1. Blinatumomab
As current therapeutics fail a significant portion of relapsed patients, novel treatment strategies may be the best option for this group of patients. Immunotherapy has proven to be an effective and highly promising approach for both relapsed and refractory patients, with survival rates superior to those observed with conventional chemotherapy, although longer follow-up is necessary. One of the most important agents in this regard is blinatumomab, a bispecific T-cell engager antibody that directs CD3+ effector memory T cells to CD19+ target cells including Pre-B ALL blasts65). A large study on adult ALL patients with relapsed or refractory disease showed that 43% of patients achieved CR or CR with incomplete hematologic recovery with single agent blinatumomab therapy, many of whom received subsequent allogeneic HCT66). Important adverse events in this study included neurologic events which occurred in 52% of patients, including 13% with grade 3 or above, and cytokine release syndrome (CRS). A phase I/II study was also undertaken in 70 pediatric patients with extremely poor prognosis, including refractory patients, first relapse patients unresponsive to salvage chemotherapy, and those in second or later relapse. After the first 2 cycles of treatment, 39% of patients achieved CR, half of whom were MRD negative, demonstrating that blinatumomab is an effective therapeutic option for pediatric patients with relapsed or refractory ALL67).- 2. Chimeric antigen receptor (CAR) T cells
- 2. Chimeric antigen receptor (CAR) T cells
Immunotherapy utilizing autologous T cells transduced to express a receptor with specificity for CD19 has been extremely effective in relapsed/refractory ALL patients. Reported rates of CR after CAR T-cell therapy in this group of patients range from 70%–90%68,69). The Children's Hospital of Philadelphia reported a 6-month EFS of 67%, with 19 out of 27 patients who achieved CR maintaining remission, most without any further therapy69). Important side effects of CAR T-cell therapy include prolonged B-cell aplasia requiring intravenous immune globulin treatment, encephalopathy and, most importantly CRS, the degree of which corresponds to leukemia burden at treatment. CRS shows laboratory findings consistent with macrophage activation syndrome, and increased levels of interleukin-6 (IL-6), allowing for treatment of this complication with the IL-6 receptor inhibitor tocilizumab. The duration of CAR T-cell efficacy most likely affects long-term EFS, with one study reporting 68% probability of CAR T cell persistence 6 months postinfusion69). An important method of CAR T cell treatment failure has been loss of CD19 expression by the leukemic blast after therapy. Such immunologic escape can be countered by the production of CAR T cells with dual targets, such as both CD19 and IL-3 receptor α-chain (CD123) as shown in a recent study70). Some of the CD19-relapsed patients have also shown the new expression of myeloid markers, or blasts consistent with acute myeloid leukemia, underscoring lineage switch as a means of evading T-cell surveillance71).
Relapse is the most important cause of treatment failure in ALL, and a leading cause of cancer-related death in children. Long-term follow-up of a large number of relapsed patients showed survival rates ranging from 10% to over 50% depending on important prognostic factors such as site of relapse, duration of first remission, and initial risk group62,63). Relapsed patients with high risk of subsequent treatment failure may be treated with allogeneic HCT in second CR, but the outcome still remains poor64).
- Long-term effects of treatment
- Long-term effects of treatment
With the remarkable improvement in survival of pediatric ALL compared to the past, much of the current focus is on maintaining high survival rates while limiting the long-term toxicities of treatment. Significant long-term effects include neurocognitive impairment, endocrine complications, cardiac dysfunction, and the risk for secondary malignancies72).Neurocognitive sequelae will have a profound effect on the adult survivor's ability to function in society. The decrease in the dose of cranial irradiation currently administered compared to the past, and the elimination of cranial irradiation in many patients contribute to lessening such toxicities. One study found that patients who received 18-Gy cranial irradiation and intrathecal chemotherapy had similar neurocognitive complications to those who received intensive triple intrathecal chemotherapy with omission of cranial irradiation73). However, a study done in our cohort of survivors showed that patients who completed treatment including 18-Gy cranial irradiation performed significantly worse on standardized tests for intelligence than patients who did not receive cranial irradiation74). Regardless of the potential additional impact of CNS radiation, studies have shown that patients given other means of CNS therapy, such as multiple intrathecal infusions and systemic treatment such as high dose MTX, have also performed poorly on neurocognitive tests after treatment completion75).Endocrine complications, such as the metabolic syndrome and short stature, may result from the use of steroids, as well as cranial irradiation. Again, the elimination of cranial irradiation in many patients may aid in minimizing these toxicities. In our study of patients treated with dexamethasone-based chemotherapy and without cranial irradiation, random glucose and body mass index decreased significantly at 12 months posttreatment completion compared to values measured during chemotherapy76). Although limited by short-term follow-up, our study did not find evidence for either long-term glucose intolerance or potential obesity during the aftermath of therapy for patients treated without allogeneic HCT and cranial irradiation. One debilitating complication of steroid therapy is osteonecrosis, with one study reporting that 60% of patients followed for 5 years since diagnosis of osteonecrosis continued to show symptoms related to this complication56).Although patients treated on current protocols receive less of a cumulative anthracycline dose than in the past, these patients are still at risk for asymptomatic abnormalities of cardiac function that may progress to overt heart dysfunction with long-term follow-up77). Patients who have completed a treatment regimen that included anthracyclines should undergo periodic evaluation of heart function. Administering the cardioprotectant dexrazoxane along with anthracyclines may limit long-term cardiac effects78).
- Conclusions
- Conclusions
The findings from large cooperative trials have resulted in a remarkably improved survival rate for children with ALL. The key areas for future work should include studies to improve the outcome of high risk ALL, including Ph+ ALL and infant ALL, the implementation of novel therapies to treat patients who relapse, whose outcome still remains extremely poor, and the attempt to identify and minimize long-term toxicities from treatment.
- Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
- References
- 1. Park HJ, Moon EK, Yoon JY, Oh CM, Jung KW, Park BK, et al. Incidence and Survival of Childhood Cancer in Korea. Cancer Res Treat 2016;48:869–882.
[Article] [PubMed] [PMC]2. George P, Hernandez K, Hustu O, Borella L, Holton C, Pinkel D. A study of “total therapy” of acute lymphocytic leukemia in children. J Pediatr 1968;72:399–408.
[Article] [PubMed]3. Möricke A, Reiter A, Zimmermann M, Gadner H, Stanulla M, Dördelmann M, et al. Risk-adjusted therapy of acute lymphoblastic leukemia can decrease treatment burden and improve survival: treatment results of 2169 unselected pediatric and adolescent patients enrolled in the trial ALL-BFM 95. Blood 2008;111:4477–4489.
[Article] [PubMed]4. Hunger SP, Lu X, Devidas M, Camitta BM, Gaynon PS, Winick NJ, et al. Improved survival for children and adolescents with acute lymphoblastic leukemia between 1990 and 2005: a report from the children's oncology group. J Clin Oncol 2012;30:1663–1669.
[Article] [PubMed] [PMC]5. Pui CH, Campana D, Pei D, Bowman WP, Sandlund JT, Kaste SC, et al. Treating childhood acute lymphoblastic leukemia without cranial irradiation. N Engl J Med 2009;360:2730–2741.
[Article] [PubMed] [PMC]6. Lee JW, Kim SK, Jang PS, Jeong DC, Chung NG, Cho B, et al. Treatment of children with acute lymphoblastic leukemia with risk group based intensification and omission of cranial irradiation: A Korean study of 295 patients. Pediatr Blood Cancer 2016;63:1966–1973.
[Article] [PubMed]7. Pieters R, Schrappe M, De Lorenzo P, Hann I, De Rossi G, Felice M, et al. A treatment protocol for infants younger than 1 year with acute lymphoblastic leukaemia (Interfant-99): an observational study and a multicentre randomised trial. Lancet 2007;370:240–250.
[Article] [PubMed]8. Smith M, Arthur D, Camitta B, Carroll AJ, Crist W, Gaynon P, et al. Uniform approach to risk classification and treatment assignment for children with acute lymphoblastic leukemia. J Clin Oncol 1996;14:18–24.
[Article] [PubMed]9. Yeoh AE, Ariffin H, Chai EL, Kwok CS, Chan YH, Ponnudurai K, et al. Minimal residual disease-guided treatment deintensification for children with acute lymphoblastic leukemia: results from the Malaysia-Singapore acute lymphoblastic leukemia 2003 study. J Clin Oncol 2012;30:2384–2392.
[Article] [PubMed]10. Bhojwani D, Pei D, Sandlund JT, Jeha S, Ribeiro RC, Rubnitz JE, et al. ETV6-RUNX1-positive childhood acute lymphoblastic leukemia: improved outcome with contemporary therapy. Leukemia 2012;26:265–270.
[Article] [PubMed]11. Moorman AV, Ensor HM, Richards SM, Chilton L, Schwab C, Kinsey SE, et al. Prognostic effect of chromosomal abnormalities in childhood B-cell precursor acute lymphoblastic leukaemia: results from the UK Medical Research Council ALL97/99 randomised trial. Lancet Oncol 2010;11:429–438.
[Article] [PubMed]12. Borowitz MJ, Devidas M, Hunger SP, Bowman WP, Carroll AJ, Carroll WL, et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia and its relationship to other prognostic factors: a Children's Oncology Group study. Blood 2008;111:5477–5485.
[Article] [PubMed] [PMC]13. Lee JW, Kim SK, Jang PS, Chung NG, Jeong DC, Kim M, et al. Outcome and Prognostic Factors for ETV6/RUNX1 Positive Pediatric Acute Lymphoblastic Leukemia Treated at a Single Institution in Korea. Cancer Res Treat 2017;49:446–453.
[Article] [PubMed]14. Harrison CJ, Moorman AV, Broadfield ZJ, Cheung KL, Harris RL, Reza Jalali G, et al. Three distinct subgroups of hypodiploidy in acute lymphoblastic leukaemia. Br J Haematol 2004;125:552–559.
[Article] [PubMed]15. Nachman JB, Heerema NA, Sather H, Camitta B, Forestier E, Harrison CJ, et al. Outcome of treatment in children with hypodiploid acute lymphoblastic leukemia. Blood 2007;110:1112–1115.
[Article] [PubMed] [PMC]16. Holmfeldt L, Wei L, Diaz-Flores E, Walsh M, Zhang J, Ding L, et al. The genomic landscape of hypodiploid acute lymphoblastic leukemia. Nat Genet 2013;45:242–252.
[Article] [PubMed] [PMC]17. Jeha S, Pei D, Raimondi SC, Onciu M, Campana D, Cheng C, et al. Increased risk for CNS relapse in pre-B cell leukemia with the t(1;19)/TCF3-PBX1. Leukemia 2009;23:1406–1409.
[Article] [PubMed] [PMC]18. Inukai T, Hirose K, Inaba T, Kurosawa H, Hama A, Inada H, et al. Hypercalcemia in childhood acute lymphoblastic leukemia: frequent implication of parathyroid hormone-related peptide and E2A-HLF from translocation 17;19. Leukemia 2007;21:288–296.
[Article] [PubMed]19. Moorman AV, Richards SM, Robinson HM, Strefford JC, Gibson BE, Kinsey SE, et al. Prognosis of children with acute lymphoblastic leukemia (ALL) and intrachromosomal amplification of chromosome 21 (iAMP21). Blood 2007;109:2327–2330.
[Article] [PubMed]20. Moorman AV, Robinson H, Schwab C, Richards SM, Hancock J, Mitchell CD, et al. Risk-directed treatment intensification significantly reduces the risk of relapse among children and adolescents with acute lymphoblastic leukemia and intrachromosomal amplification of chromosome 21: a comparison of the MRC ALL97/99 and UKALL2003 trials. J Clin Oncol 2013;31:3389–3396.
[Article] [PubMed]21. Mullighan CG, Su X, Zhang J, Radtke I, Phillips LA, Miller CB, et al. Deletion of IKZF1 and prognosis in acute lymphoblastic leukemia. N Engl J Med 2009;360:470–480.
[Article] [PubMed] [PMC]22. Roberts KG, Li Y, Payne-Turner D, Harvey RC, Yang YL, Pei D, et al. Targetable kinase-activating lesions in Ph-like acute lymphoblastic leukemia. N Engl J Med 2014;371:1005–1015.
[Article] [PubMed] [PMC]23. Weston BW, Hayden MA, Roberts KG, Bowyer S, Hsu J, Fedoriw G, et al. Tyrosine kinase inhibitor therapy induces remission in a patient with refractory EBF1-PDGFRB-positive acute lymphoblastic leukemia. J Clin Oncol 2013;31:e413–e416.
[Article] [PubMed]24. Lengline E, Beldjord K, Dombret H, Soulier J, Boissel N, Clappier E. Successful tyrosine kinase inhibitor therapy in a refractory B-cell precursor acute lymphoblastic leukemia with EBF1-PDGFRB fusion. Haematologica 2013;98:e146–e148.
[Article] [PubMed] [PMC]25. Ferrando AA. The role of NOTCH1 signaling in T-ALL. Hematology Am Soc Hematol Educ Program. 2009;:353–361.26. Coustan-Smith E, Mullighan CG, Onciu M, Behm FG, Raimondi SC, Pei D, et al. Early T-cell precursor leukaemia: a subtype of very high-risk acute lymphoblastic leukaemia. Lancet Oncol 2009;10:147–156.
[Article] [PubMed] [PMC]27. Patrick K, Wade R, Goulden N, Mitchell C, Moorman AV, Rowntree C, et al. Outcome for children and young people with Early T-cell precursor acute lymphoblastic leukaemia treated on a contemporary protocol, UKALL 2003. Br J Haematol 2014;166:421–424.
[Article] [PubMed]28. Conter V, Valsecchi MG, Buldini B, Parasole R, Locatelli F, Colombini A, et al. Early T-cell precursor acute lymphoblastic leukaemia in children treated in AIEOP centres with AIEOP-BFM protocols: a retrospective analysis. Lancet Haematol 2016;3:e80–e86.
[Article] [PubMed]29. Möricke A, Zimmermann M, Reiter A, Henze G, Schrauder A, Gadner H, et al. Long-term results of five consecutive trials in childhood acute lymphoblastic leukemia performed by the ALL-BFM study group from 1981 to 2000. Leukemia 2010;24:265–284.
[Article] [PubMed]30. Brüggemann M, Schrauder A, Raff T, Pfeifer H, Dworzak M, Ottmann OG, et al. Standardized MRD quantification in European ALL trials: proceedings of the Second International Symposium on MRD assessment in Kiel, Germany, 18-20 September 2008. Leukemia 2010;24:521–535.
[Article] [PubMed]31. Coustan-Smith E, Sancho J, Hancock ML, Boyett JM, Behm FG, Raimondi SC, et al. Clinical importance of minimal residual disease in childhood acute lymphoblastic leukemia. Blood 2000;96:2691–2696.
[Article] [PubMed]32. Conter V, Bartram CR, Valsecchi MG, Schrauder A, Panzer-Grümayer R, Möricke A, et al. Molecular response to treatment redefines all prognostic factors in children and adolescents with B-cell precursor acute lymphoblastic leukemia: results in 3184 patients of the AIEOP-BFM ALL 2000 study. Blood 2010;115:3206–3214.
[Article] [PubMed]33. Schrappe M, Valsecchi MG, Bartram CR, Schrauder A, Panzer-Grümayer R, Möricke A, et al. Late MRD response determines relapse risk overall and in subsets of childhood T-cell ALL: results of the AIEOP-BFM-ALL 2000 study. Blood 2011;118:2077–2084.
[Article] [PubMed]34. Gajjar A, Harrison PL, Sandlund JT, Rivera GK, Ribeiro RC, Rubnitz JE, et al. Traumatic lumbar puncture at diagnosis adversely affects outcome in childhood acute lymphoblastic leukemia. Blood 2000;96:3381–3384.
[Article] [PubMed]35. Hasegawa D, Manabe A, Ohara A, Kikuchi A, Koh K, Kiyokawa N, et al. The utility of performing the initial lumbar puncture on day 8 in remission induction therapy for childhood acute lymphoblastic leukemia: TCCSG L99-15 study. Pediatr Blood Cancer 2012;58:23–30.
[Article] [PubMed]36. Blaney SM, Poplack DG, Godwin K, McCully CL, Murphy R, Balis FM. Effect of body position on ventricular CSF methotrexate concentration following intralumbar administration. J Clin Oncol 1995;13:177–179.
[Article] [PubMed]37. Vrooman LM, Stevenson KE, Supko JG, O'Brien J, Dahlberg SE, Asselin BL, et al. Postinduction dexamethasone and individualized dosing of Escherichia Coli L-asparaginase each improve outcome of children and adolescents with newly diagnosed acute lymphoblastic leukemia: results from a randomized study--Dana-Farber Cancer Institute ALL Consortium Protocol 00-01. J Clin Oncol 2013;31:1202–1210.
[Article] [PubMed] [PMC]38. Schrappe M, Reiter A, Zimmermann M, Harbott J, Ludwig WD, Henze G, et al. Long-term results of four consecutive trials in childhood ALL performed by the ALL-BFM study group from 1981 to 1995. Berlin-Frankfurt-Münster. Leukemia 2000;14:2205–2222.
[Article] [PubMed]39. Veerman AJ, Kamps WA, van den Berg H, van den Berg E, Bökkerink JP, Bruin MC, et al. Dexamethasone-based therapy for childhood acute lymphoblastic leukaemia: results of the prospective Dutch Childhood Oncology Group (DCOG) protocol ALL-9 (1997-2004). Lancet Oncol 2009;10:957–966.
[Article] [PubMed]40. Vora A, Goulden N, Wade R, Mitchell C, Hancock J, Hough R, et al. Treatment reduction for children and young adults with low-risk acute lymphoblastic leukaemia defined by minimal residual disease (UKALL 2003): a randomised controlled trial. Lancet Oncol 2013;14:199–209.
[Article] [PubMed]41. Nachman JB, Sather HN, Sensel MG, Trigg ME, Cherlow JM, Lukens JN, et al. Augmented post-induction therapy for children with high-risk acute lymphoblastic leukemia and a slow response to initial therapy. N Engl J Med 1998;338:1663–1671.
[Article] [PubMed]42. Bhatia S, Landier W, Hageman L, Chen Y, Kim H, Sun CL, et al. Systemic exposure to thiopurines and risk of relapse in children with acute lymphoblastic leukemia: a children's oncology group study. JAMA Oncol 2015;1:287–295.
[Article] [PubMed] [PMC]43. Schrappe M, Hunger SP, Pui CH, Saha V, Gaynon PS, Baruchel A, et al. Outcomes after induction failure in childhood acute lymphoblastic leukemia. N Engl J Med 2012;366:1371–1381.
[Article] [PubMed] [PMC]44. Aricò M, Valsecchi MG, Camitta B, Schrappe M, Chessells J, Baruchel A, et al. Outcome of treatment in children with Philadelphia chromosome-positive acute lymphoblastic leukemia. N Engl J Med 2000;342:998–1006.
[Article] [PubMed]45. Schultz KR, Carroll A, Heerema NA, Bowman WP, Aledo A, Slayton WB, et al. Long-term follow-up of imatinib in pediatric Philadelphia chromosome-positive acute lymphoblastic leukemia: Children's Oncology Group study AALL0031. Leukemia 2014;28:1467–1471.
[Article] [PubMed] [PMC]46. Biondi A, Schrappe M, De Lorenzo P, Castor A, Lucchini G, Gandemer V, et al. Imatinib after induction for treatment of children and adolescents with Philadelphia-chromosome-positive acute lymphoblastic leukaemia (EsPhALL): a randomised, open-label, intergroup study. Lancet Oncol 2012;13:936–945.
[Article] [PubMed]47. Rives S, Estella J, Gómez P, López-Duarte M, de Miguel PG, Verdeguer A, et al. Intermediate dose of imatinib in combination with chemotherapy followed by allogeneic stem cell transplantation improves early outcome in paediatric Philadelphia chromosome-positive acute lymphoblastic leukaemia (ALL): results of the Spanish Cooperative Group SHOP studies ALL-94, ALL-99 and ALL-2005. Br J Haematol 2011;154:600–611.
[Article] [PubMed]48. Lee S, Kim YJ, Chung NG, Lim J, Lee DG, Kim HJ, et al. The extent of minimal residual disease reduction after the first 4-week imatinib therapy determines outcome of allogeneic stem cell transplantation in adults with Philadelphia chromosome-positive acute lymphoblastic leukemia. Cancer 2009;115:561–570.
[Article] [PubMed]49. Aoe M, Shimada A, Muraoka M, Washio K, Nakamura Y, Takahashi T, et al. ABL kinase mutation and relapse in 4 pediatric Philadelphia chromosome-positive acute lymphoblastic leukemia cases. Int J Hematol 2014;99:609–615.
[Article] [PubMed]50. Bansal D, Shava U, Varma N, Trehan A, Marwaha RK. Imatinib has adverse effect on growth in children with chronic myeloid leukemia. Pediatr Blood Cancer 2012;59:481–484.
[Article] [PubMed]51. Dreyer ZE, Hilden JM, Jones TL, Devidas M, Winick NJ, Willman CL, et al. Intensified chemotherapy without SCT in infant ALL: results from COG P9407 (Cohort 3). Pediatr Blood Cancer 2015;62:419–426.
[Article] [PubMed]52. Koh K, Tomizawa D, Moriya Saito A, Watanabe T, Miyamura T, Hirayama M, et al. Early use of allogeneic hematopoietic stem cell transplantation for infants with MLL gene-rearrangement-positive acute lymphoblastic leukemia. Leukemia 2015;29:290–296.
[Article] [PubMed]53. Mann G, Attarbaschi A, Schrappe M, De Lorenzo P, Peters C, Hann I, et al. Improved outcome with hematopoietic stem cell transplantation in a poor prognostic subgroup of infants with mixed-lineage-leukemia (MLL)-rearranged acute lymphoblastic leukemia: results from the Interfant-99 Study. Blood 2010;116:2644–2650.
[Article] [PubMed]54. Nagayama J, Tomizawa D, Koh K, Nagatoshi Y, Hotta N, Kishimoto T, et al. Infants with acute lymphoblastic leukemia and a germline MLL gene are highly curable with use of chemotherapy alone: results from the Japan Infant Leukemia Study Group. Blood 2006;107:4663–4665.
[Article] [PubMed]55. Ram R, Wolach O, Vidal L, Gafter-Gvili A, Shpilberg O, Raanani P. Adolescents and young adults with acute lymphoblastic leukemia have a better outcome when treated with pediatric-inspired regimens: systematic review and meta-analysis. Am J Hematol 2012;87:472–478.
[Article] [PubMed]56. te Winkel ML, Pieters R, Hop WC, de Groot-Kruseman HA, Lequin MH, van der Sluis IM, et al. Prospective study on incidence, risk factors, and long-term outcome of osteonecrosis in pediatric acute lymphoblastic leukemia. J Clin Oncol 2011;29:4143–4150.
[Article] [PubMed]57. Kondryn HJ, Edmondson CL, Hill J, Eden TO. Treatment non-adherence in teenage and young adult patients with cancer. Lancet Oncol 2011;12:100–108.
[Article] [PubMed]58. Lee P, Bhansali R, Izraeli S, Hijiya N, Crispino JD. The biology, pathogenesis and clinical aspects of acute lymphoblastic leukemia in children with Down syndrome. Leukemia 2016;30:1816–1823.
[Article] [PubMed] [PMC]59. Hertzberg L, Vendramini E, Ganmore I, Cazzaniga G, Schmitz M, Chalker J, et al. Down syndrome acute lymphoblastic leukemia, a highly heterogeneous disease in which aberrant expression of CRLF2 is associated with mutated JAK2: a report from the International BFM Study Group. Blood 2010;115:1006–1017.
[Article] [PubMed]60. Buitenkamp TD, Izraeli S, Zimmermann M, Forestier E, Heerema NA, van den Heuvel-Eibrink MM, et al. Acute lymphoblastic leukemia in children with Down syndrome: a retrospective analysis from the Ponte di Legno study group. Blood 2014;123:70–77.
[Article] [PubMed] [PMC]61. Buitenkamp TD, Mathôt RA, de Haas V, Pieters R, Zwaan CM. Methotrexate-induced side effects are not due to differences in pharmacokinetics in children with Down syndrome and acute lymphoblastic leukemia. Haematologica 2010;95:1106–1113.
[Article] [PubMed] [PMC]62. Nguyen K, Devidas M, Cheng SC, La M, Raetz EA, Carroll WL, et al. Factors influencing survival after relapse from acute lymphoblastic leukemia: a Children's Oncology Group study. Leukemia 2008;22:2142–2150.
[Article] [PubMed] [PMC]63. Oskarsson T, Söderhäll S, Arvidson J, Forestier E, Montgomery S, Bottai M, et al. Relapsed childhood acute lymphoblastic leukemia in the Nordic countries: prognostic factors, treatment and outcome. Haematologica 2016;101:68–76.
[Article] [PubMed] [PMC]64. Lee EJ, Han JY, Lee JW, Jang PS, Chung NG, Jeong DC, et al. Outcome of allogeneic hematopoietic stem cell transplantation for childhood acute lymphoblastic leukemia in second complete remission: a single institution study. Korean J Pediatr 2012;55:100–106.
[Article] [PubMed] [PMC]65. Löffler A, Kufer P, Lutterbüse R, Zettl F, Daniel PT, Schwenkenbecher JM, et al. A recombinant bispecific single-chain antibody, CD19 x CD3, induces rapid and high lymphoma-directed cytotoxicity by unstimulated T lymphocytes. Blood 2000;95:2098–2103.
[Article] [PubMed]66. Topp MS, Gökbuget N, Stein AS, Zugmaier G, O'Brien S, Bargou RC, et al. Safety and activity of blinatumomab for adult patients with relapsed or refractory B-precursor acute lymphoblastic leukaemia: a multicentre, single-arm, phase 2 study. Lancet Oncol 2015;16:57–66.
[Article] [PubMed]67. von Stackelberg A, Locatelli F, Zugmaier G, Handgretinger R, Trippett TM, Rizzari C, et al. Phase I/Phase II Study of Blinatumomab in Pediatric Patients With Relapsed/Refractory Acute Lymphoblastic Leukemia. J Clin Oncol 2016;34:4381–4389.
[Article] [PubMed]68. Lee DW, Kochenderfer JN, Stetler-Stevenson M, Cui YK, Delbrook C, Feldman SA, et al. T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet 2015;385:517–528.
[Article] [PubMed]69. Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med 2014;371:1507–1517.
[Article] [PubMed] [PMC]70. Ruella M, Barrett DM, Kenderian SS, Shestova O, Hofmann TJ, Perazzelli J, et al. Dual CD19 and CD123 targeting prevents antigen-loss relapses after CD19-directed immunotherapies. J Clin Invest 2016;126:3814–3826.
[Article] [PubMed] [PMC]71. Gardner R, Wu D, Cherian S, Fang M, Hanafi LA, Finney O, et al. Acquisition of a CD19-negative myeloid phenotype allows immune escape of MLL-rearranged B-ALL from CD19 CAR-T-cell therapy. Blood 2016;127:2406–2410.
[Article] [PubMed] [PMC]72. Silverman LB. Balancing cure and long-term risks in acute lymphoblastic leukemia. Hematology Am Soc Hematol Educ Program 2014;2014:190–197.
[Article] [PubMed]73. Waber DP, Turek J, Catania L, Stevenson K, Robaey P, Romero I, et al. Neuropsychological outcomes from a randomized trial of triple intrathecal chemotherapy compared with 18 Gy cranial radiation as CNS treatment in acute lymphoblastic leukemia: findings from Dana-Farber Cancer Institute ALL Consortium Protocol 95-01. J Clin Oncol 2007;25:4914–4921.
[Article] [PubMed]74. Kim SJ, Park MH, Lee JW, Chung NG, Cho B, Lee IG, et al. Neurocognitive outcome in survivors of childhood acute lymphoblastic leukemia: experience at a tertiary care hospital in Korea. J Korean Med Sci 2015;30:463–469.
[Article] [PubMed] [PMC]75. Krull KR, Brinkman TM, Li C, Armstrong GT, Ness KK, Srivastava DK, et al. Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic leukemia: a report from the St Jude lifetime cohort study. J Clin Oncol 2013;31:4407–4415.
[Article] [PubMed] [PMC]76. Bang KW, Seo SY, Lee JW, Jang PS, Jung MH, Chung NG, et al. Evaluation of changes in random blood glucose and body mass index during and after completion of chemotherapy in children with acute lymphoblastic leukemia. Korean J Pediatr 2012;55:121–127.
[Article] [PubMed] [PMC]77. Lipshultz SE, Lipsitz SR, Sallan SE, Dalton VM, Mone SM, Gelber RD, et al. Chronic progressive cardiac dysfunction years after doxorubicin therapy for childhood acute lymphoblastic leukemia. J Clin Oncol 2005;23:2629–2636.
[Article] [PubMed]78. Lipshultz SE, Scully RE, Lipsitz SR, Sallan SE, Silverman LB, Miller TL, et al. Assessment of dexrazoxane as a cardioprotectant in doxorubicin-treated children with high-risk acute lymphoblastic leukaemia: long-term follow-up of a prospective, randomised, multicentre trial. Lancet Oncol 2010;11:950–961.
[Article] [PubMed] [PMC]
Fig. 1
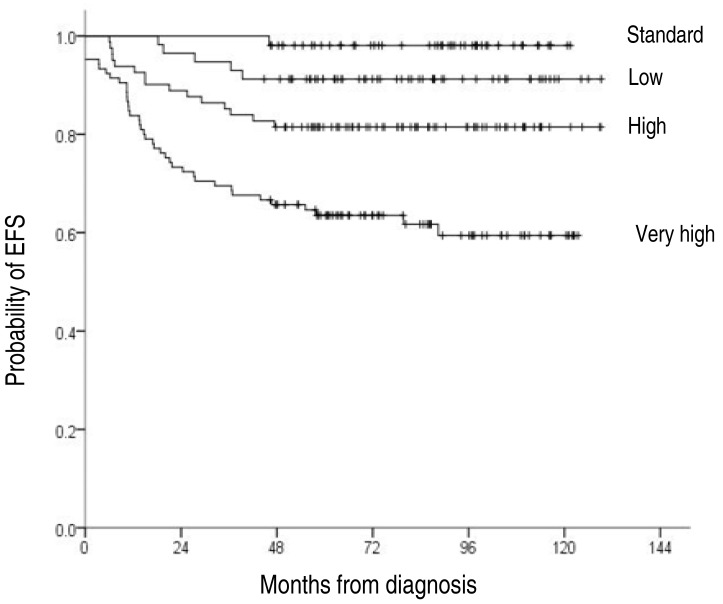
Table 1
ALL, acute lymphoblastic leukemia; WBC, white blood cell; CNS, central nervous system; MRD, minimal residual disease; CR, complete remission.
*CNS 3 (elevated CSF WBC (≥5 cells/µL) and cytology showing lymphoblasts) is the criterion for diagnosis of CNS involvement. †Poor prephase steroid response indicates a peripheral blast count ≥1,000/mm3 after 7 days of steroid treatment. ‡MRD not measured for all patients, but measured using reverse trancription-polymerase chain reaction or real-time quantitative-polymerase chain reaction for patients with recurrent genetic abnormalities.

 About
About Browse articles
Browse articles For contributors
For contributors
