All issues > Volume 61(1); 2018
C-reactive protein and N-terminal pro-brain natriuretic peptide discrepancy: a differentiation of adenoviral pharyngoconjunctival fever from Kawasaki disease
- Corresponding author: Sejung Sohn, MD. Department of Pediatrics, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, 1071 Anyangcheon-ro, Yangcheon-gu, Seoul 07985, Korea. Tel: +82-2650-5579, Fax: +82-2653-3718, sohn@ewha.ac.kr
- Received December 28, 2017 Revised January 04, 2018 Accepted January 05, 2018
- Abstract
-
- Purpose
- Purpose
- To differentiate adenoviral pharyngoconjunctival fever (PCF) from acute Kawasaki disease (KD) using laboratory tests before results of virus-real time polymerase chain reaction and ophthalmologic examination are obtained.
- Methods
- Methods
- Baseline patient characteristics and laboratory measurements were compared between 40 patients with adenovirus infection and 123 patients with KD.
- Results
- Results
- The patients with adenovirus infection were generally older than those with KD (median: 3.9 years vs. 2 years, P=0.000). White blood cell and, platelet count, and aspartate aminotransferase, alanine aminotransferase, and N-terminal pro-brain natriuretic peptide (NT-proBNP) levels showed significant differences between the 2 groups, but the C-reactive protein (CRP) levels did not (6.8±3.0 mg/dL vs. 8.3±5.8 mg/dL, P=0.126). In the adenovirus infection group, the CRP levels were <1, <3, <10, and ≥10 mg/dL in 2 (5%), 3 (7.5%), 30 (75%), and 5 patients (12.5%), respectively. The cutoff NT-proBNP level was 265 pg/mL. Discrepancy was defined as CRP and NT-proBNP levels of ≥3 or <3 mg/dL, and <265 or ≥265 pg/mL, respectively. Among the 35 patients with adenovirus infection whose CRP levels were ≥3 mg/dL, 29 (82.9%) showed a discrepancy. Conversely, of the 103 patients with KD whose CRP levels were ≥3 mg/dL, 83 (80.6%) showed no discrepancy. Between the groups, a significant difference in discrepancy rate was observed (P=0.000). None of the patients with adenovirus infection had CRP and NT-proBNP levels of <3 mg/dL and ≥265 pg/mL, respectively.
- Conclusion
- Conclusion
- With a sensitivity of 82.9% and a specificity of 80.6%, CRP and NT-proBNP levels may differentiate between adenoviral PCF and acute KD.
- Introduction
- Introduction
Among the protean manifestations of adenovirus infection, pharyngoconjunctival fever (PCF) is likely to be misdiagnosed as Kawasaki disease (KD) due to many similar clinical presentation, including fever, conjunctival injection, pharyngitis, or skin rashes. PCF, however, has some distinct symptoms: the occurrence of conjunctivitis with or without pharyngitis or respiratory symptoms. It usually begins in one eye and spreads contralaterally, despite the possibility of simultaneous infection. Mild pain or discomfort, pruritus, and morning crusting may also be common. Uveitis is not present, and tonsillar exudate may be associated. Nonetheless, we often experience difficulty in differentiating between KD and PCF at the early phase of the disease. Therefore, we sought to determine which laboratory tests may be best suited for differentiating adenoviral PCF from acute KD, before needing to obtain the results of virus-real time polymerase chain reaction (PCR) and ophthalmologic examination.
- Materials and methods
- Materials and methods
- 1. Definition
- 1. Definition
The duration of fever was defined as the number of days (24-hour period) elapsed from the onset of disease to presentation. Fever was defined as a temperature≥38℃. The definition of discrepancy was described in the results section.- 2. Statistical analysis
- 2. Statistical analysis
The IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA) was used to compared the 2 groups. Data are presented as the median, as well as the mean±standard deviation, or as numbers and percentages of patients. Continuous variables between the groups were compared using Student t test. When the variables in either group are not normally distributed, Mann-Whitney test was used. Categorical variables were compared using the chi-square test. To determine the cutoff values of parameters, a receiver operating characteristic (ROC) curve was used. Multivariate logistic regression analysis was performed using age plus laboratory variables that had been selected by univariate analysis to determine the independent parameters in differentiating the groups, and the results were expressed as an odds ratio with a 95% confidence interval (CI). A 95% CI that did not include 1.0 was interpreted to indicate statistical significance. A 2-tailed P<0.05 was considered to have statistical significance.The study was approved by the Institutional Review Board of Ewha Womans University (#2017-09-033-001). Written informed consent by the patients was waived due to a retrospective nature of our study.
During the period between May 2016 and July 2016, a total of 135 children were clinically diagnosed with adenovirus infection. Patients were excluded when (1) adenovirus was not identified by real-time PCR in nasopharyngeal secretions, (2) coinfection was present with other respiratory viruses, (3) antimycoplasma antibody IgM was positive in the serum, (4) uveitis was detected by a slit-lamp examination, and (5) laboratory tests were omitted. Finally, a total of 40 patients were retrospectively enrolled in the adenovirus infection group.During the 23-month period (November 2008–September 2010), a total of 123 children who met the diagnostic criteria for KD1) were enrolled in the KD group. This group of patients was reported as subjects in a previous study.2)We measured the white blood cell (WBC) count, percentage of neutrophils in WBCs (% neutrophils), hemoglobin, hematocrit, platelet counts, serum sodium, aspartate aminotransferase (AST), alanine aminotransferase (ALT), protein, albumin, C-reactive protein (CRP), and N-terminal pro-brain natriuretic peptide (NT-proBNP) at presentation.We compared the basic patient characteristics and laboratory values between KD and adenovirus patients.
- Results
- Results
- 1. Adenovirus patients
- 1. Adenovirus patients
The median age of adenovirus patients at presentation was 3.9 years (interquartile range, 3.2–5.0). They were older than KD patients (P=0.000). They had a fever for a median duration of 4 days. There was no difference in the fever duration between the 2 groups (P=0.514). Conjunctival injection was present in 23 patients, tonsillar exudate in 7, skin rashes in 8, and cervical lymphadenopathy in 2. All adenovirus patients were proved by a positive real-time PCR result in nasopharyngeal secretions, without any evidence of uveitis. A comparison of basic patient characteristics between KD and adenovirus patients is shown in Table 1.- 2. Comparison in laboratory values between KD and adenovirus patients
- 2. Comparison in laboratory values between KD and adenovirus patients
KD and adenovirus patients did not differ in the percentage of neutrophils, hemoglobin, hematocrit, serum sodium, protein, and albumin. No difference in CRP was found (P=0.126), although the mean values of CRP were elevated in both groups. However, there were significant differences between the 2 groups with respect to WBC (P=0.000), platelet (P=0.000), AST (v=0.001), ALT (P=0.000), and NT-proBNP (P=0.000). The mean values of these 5 parameters in adenovirus patients were lower than those in KD patients (Table 2).- 3. Independent parameters for differentiation of adenovirus PCF from KD
- 3. Independent parameters for differentiation of adenovirus PCF from KD
A multivariate logistic regression analysis included age, WBC, platelet, AST, ALT, and NT-proBNP. Among them, WBC, platelet, and NT-proBNP proved to be the independent parameters for differentiation (Table 3).The cutoff value for these parameters was determined by the ROC curve: the WBC cutoff value of 10,820/mm3 provided a sensitivity of 72.5% and a specificity of 75.6%, with an area under the curve (AUC) of 0.77 (95% CI, 0.68–0.87; P=0.000); the platelet cutoff value of 300,500/mm3 provided a sensitivity of 80% and a specificity of 58.5% (AUC=0.74; 95% CI, 0.66–0.83; P=0.000); and the NT-proBNP cutoff value of 265 pg/mL yielded a sensitivity of 85% and a specificity of 75.6% (AUC=0.89; 95% CI, 0.83–0.94; P=0.000).- 4. CRP and NT-proBNP in KD and adenovirus patients
- 4. CRP and NT-proBNP in KD and adenovirus patients
The values of CRP and NT-proBNP in both groups of patients are shown in Table 4 and plotted in Fig. 1. In 40 adenovirus patients, the CRP levels of <1 mg/dL, <3 mg/dL, <10 mg/dL, and ≥10 mg/dL were found in 2 (5%), 3 (7.5%), 30 (75%), and 5 (12.5%), respectively. Almost 90% of adenovirus patients had a CRP level of ≥3 mg/dL. Therefore, we arbitrarily defined the diagnostic value for adenoviral PCF as a CRP level of 3 mg/dL, and this value matched the criterion of the American Heart Association for the evaluation of suspected incomplete KD.3)Using a CRP level of 3 mg/dL and a NT-proBNP cutoff value of 265 pg/mL, the discrepancy was defined as CRP≥3 mg/dL and NT-proBNP<265 pg/mL, or as CRP<3 mg/dL and NT-proBNP≥265 pg/mL. The discrepancy rate was 72.5% (29 of 40) and 24.4% (30 of 123) in adenovirus patients and KD patients, respectively (P=0.000). Among the 35 adenovirus patients with CRP≥3 mg/dL, 29 patients (82.9%) showed a discrepancy and 6 showed no discrepancy. Conversely, out of the 103 KD patients with CRP≥3 mg/dL, 83 (80.6%) showed no discrepancy and only 20 showed discrepancy. Between the groups of patients with CRP≥3 mg/dL, there was also a significant difference in the discrepancy rate (P=0.000). There was no adenovirus patient with CRP<3 mg/dL and NT-proBNP≥265 pg/mL (Table 5). There were 6 adenovirus patients who had CRP≥3 mg/dL and NT-proBNP≥265 pg/mL. They were clinically diagnosed as having adenovirus infection rather than KD with characteristic eye findings such as unilateral involvement, discharge, or eyelid swelling and no presence of uveitis, and were proved by a positive real-time PCR. With a sensitivity of 82.9% and a specificity of 80.6%, adenoviral PCF might be differentiated from acute KD by discrepancies of CRP and NT-proBNP.
- Discussion
- Discussion
Recently, there has been an increase in the proportion of patients with incomplete KD without fulfilling the diagnostic criteria.4) These patients are at increased risk of developing coronary artery lesions due to a delay in the diagnosis. As a possible differential diagnosis, adenoviral PCF with similar clinical features is considered.Adenovirus infection is strongly indicated by unilateral conjunctivitis, no presence of uveitis, presence of exudative tonsillitis, and positive virus-PCR; however, in clinical practice, differentiation between KD and PCF is often difficult.In this study, of the 40 patients who were diagnosed as adenoviral PCF during the 3-month epidemic period, conjunctival injection was present in 23 patients. This group of patients may be criticized as not PCF patients. By definition, PCF is a syndrome characterized by fever, pharyngitis, and conjunctivitis. However, not all patients have the complete syndrome triad during epidemics.5)It has been well established that exposure to adenovirus evokes increased CRP responses in contrast to other common viruses.6,7) Appenzeller et al.7) showed that CRP concentrations by adenovirus infection were not related to age, duration of fever, and severity of illness. To date, reasons for adenovirus infection to result in increased CRP concentration have not been fully elucidated. However, previous studies8,9,10) demonstrated that interleukin-6 and tumor necrosis factor-α, both being major inducers of hepatic synthesis of CRP, were elevated in an early stage of adenovirus infection, indicating that adenovirus triggers an immediate inflammatory host response resembling invasive bacterial infection.We have also noticed that adenovirus infections are associated with elevated CRP concentrations, but not increased NT-proBNP levels. This finding is quite different from that in KD. Therefore, we postulated that this CRP and NT-proBNP discrepancy is likely to be useful in differentiating between KD and adenoviral PCF.In adenovirus patients, the median CRP level was 7.5 mg/dL, and 87.5% of patients had CRP levels of ≥3 mg/dL. CRP levels did not differ in either adenovirus or KD patients. On the contrary, the median NT-proBNP level of 125 pg/mL in adenovirus patients was significantly lower than that (480 pg/mL) in KD patients.We had already proposed 260 pg/mL as the cutoff value of NT-proBNP discriminating acute KD from other acute febrile diseases with similar clinical features.11) A cutoff value of 265 pg/mL in the present study was nearly the same as that in our previous study.Regarding CRP and NT-proBNP discrepancy, a CRP level of <3 mg/dL, regardless of the NT-proBNP levels, indicates mild inflammation with no clinical significance. Moreover, there was no adenovirus patient with low CRP and high NT-proBNP. Therefore, we focused on patients with CRP≥3 mg/dL. Of the adenovirus patients, 87.5% had CRP≥3 mg/dL; of the KD patients, 83.7% had CRP≥3 mg/dL. Although CRP levels were elevated in most patients in both groups and not differ with each other, NT-proBNP levels were significantly different between the 2 groups: decreased or within the normal range (<265 pg/mL) in 82.9% of adenovirus patients versus increased range (≥265 pg/mL) in 80.6% of KD patients. The rate of CRP and NT-proBNP discrepancy significantly differed between the 2 groups.Only NT-proBNP value may be useful to discriminate between the 2 diseases,11,12) with a sensitivity of 85% and a specificity of 75.6%. However, considering both CRP and NT-proBNP simultaneously may result in easier and more rapid differentiation, with a sensitivity of 82.9% and a little higher specificity. For example, if a patient with fever, conjunctivitis, and similar clinical features to KD has CRP≥3 mg/dL and NT-proBNP<265 pg/mL, this patient is more likely to be diagnosed with adenoviral PCF rather than KD.Limitations of this study include a small number of adenovirus subjects and the retrospective nature of this study, which may lead to case exclusion due to data omission. The study was performed at different times in each group. Because we did not performed adenovirus PCR study in KD patients, the possibility remains that KD patients with coexistent adenovirus infection may be included in this group of patients. Finally, adenovirus serotypes were not identified.In conclusion, CRP and NT-proBNP discrepancy may simply and quickly discriminate adenoviral PCF from acute KD, with a sensitivity of 82.9% and a specificity of 80.6%. We cautiously propose the use of CRP and NT-proBNP discrepancy in the differential diagnosis to distinguish between incomplete KD and adenoviral PCF. A further study with a larger sample size is warranted to clarify our proposal.
- Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
- References
- 1. Dajani AS, Taubert KA, Gerber MA, Shulman ST, Ferrieri P, Freed M, et al. Diagnosis and therapy of Kawasaki disease in children. Circulation 1993;87:1776–1780.
[Article] [PubMed]2. Lee YS, Lee J, Hong YM, Sohn S. protein and erythrocyte sedimentation rate discrepancies and variations after intravenous immunoglobulin therapy in Kawasaki disease. Pediatr Infect Vaccine 2016;23:25–30.
[Article]3. Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 2004;110:2747–2771.
[Article] [PubMed]4. Ghelani SJ, Sable C, Wiedermann BL, Spurney CF. Increased incidence of incomplete Kawasaki disease at a pediatric hospital after publication of the 2004 American Heart Association guidelines. Pediatr Cardiol 2012;33:1097–1103.
[Article] [PubMed]5. Cherry JD, Nadipuram S. Adenoviruses. In: Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, editors. Feigin and Cherry's textbook of pediatric infectious diseases. 7th ed. Philadelphia: Elsevier Saunders, 2014:1888–1911.6. Putto A, Meurman O, Ruuskanen O. C-reactive protein in viral and bacterial infections. Pediatr Res 1985;19:1103
[Article]7. Appenzeller C, Ammann RA, Duppenthaler A, Gorgievski-Hrisoho M, Aebi C. Serum C-reactive protein in children with adenovirus infection. Swiss Med Wkly 2002;132:345–350.
[PubMed]8. Mistchenko AS, Diez RA, Mariani AL, Robaldo J, Maffey AF, Bayley-Bustamante G, et al. Cytokines in adenoviral disease in children: association of interleukin-6, interleukin-8, and tumor necrosis factor alpha levels with clinical outcome. J Pediatr 1994;124(5 Pt 1): 714–720.
[Article] [PubMed]9. Kawasaki Y, Hosoya M, Katayose M, Suzuki H. Correlation between serum interleukin 6 and C-reactive protein concentrations in patients with adenoviral respiratory infection. Pediatr Infect Dis J 2002;21:370–374.
[Article] [PubMed]10. Zsengellér Z, Otake K, Hossain SA, Berclaz PY, Trapnell BC. Internalization of adenovirus by alveolar macrophages initiates early proinflammatory signaling during acute respiratory tract infection. J Virol 2000;74:9655–9667.
[Article] [PubMed] [PMC]11. Lee H, Kim H, Kim HS, Sohn S. NT-proBNP: a new diagnostic screening tool for Kawasaki disease. Korean J Pediatr 2006;49:539–544.
[Article]
Fig. 1
A Log-scattergram of C-reactive protein (CRP) and N-terminal pro-brain natriuretic peptide (NT-proBNP) level in patients with Kawasaki disease (KD) and adenovirus infection (Adeno).
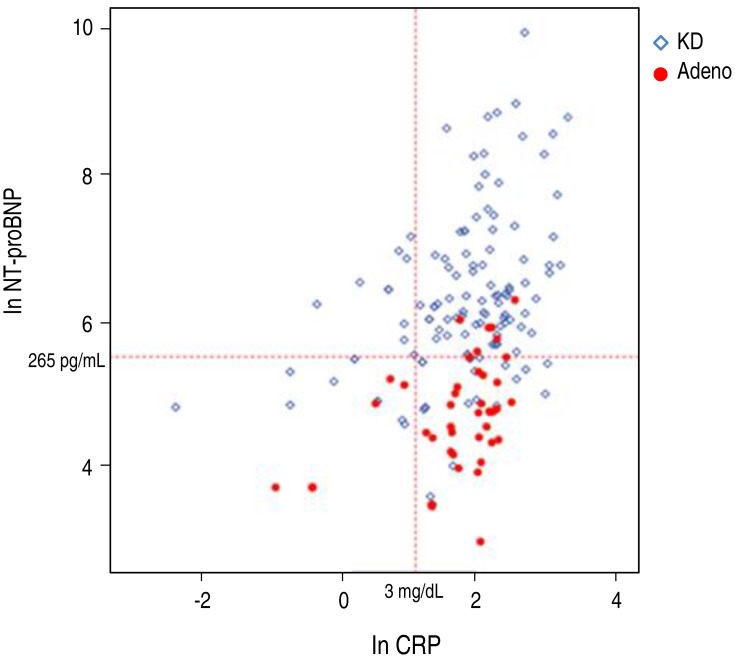
Table 1
Comparison of the basic characteristics of the patients with KD and adenovirus infection
Table 2
Comparison of laboratory values between the patients with KD and adenovirus infection
Table 3
Multivariate logistic analysis for the differentiation of adenovirus Infection from KD
| Variable | P value | Odds ratio | 95% CI |
|---|---|---|---|
| WBC (×103/mm3) | 0.014 | 0.819 | 0.698–0.961 |
| Platelet (×103/mm3) | 0.014 | 0.987 | 0.974–0.997 |
| NT-proBNP (pg/mL) | 0.000 | 0.992 | 0.988–0.996 |
KD, Kawasaki disease; CI, confidence interval; WBC, white blood cell; NT-proBNP, N-terminal pro-brain natriuretic peptide.
Age, aspartate aminotransferase, and alanine aminotransferase in addition to 3 variables in this table (WBC, platelet, and NT-proBNP) were included in the multivariate logistic analysis.
Table 4
CRP and NT-proBNP levels in the KD and adenovirus groups

 About
About Browse articles
Browse articles For contributors
For contributors
