All issues > Volume 59(Suppl 1); 2016
Type I Chiari malformation presenting orthostatic syncope who treated with decompressive surgery
- Corresponding author: Joon Soo Lee, MD, PHD. Division of Pediatric Neurology, Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea. Tel: +82-2-2228-2063, Fax: +82-2-393-9118, JOONSL96@yuhs.ac
- Received September 04, 2014 Revised October 06, 2014 Accepted October 20, 2014
- Abstract
-
Chiari malformations are a congenital anomaly of the hindbrain. The most common, Chiari malformation type I (CM-I), is characterized by herniation of the cerebellar tonsils extending at least 3 mm below the plane of the foramen magnum. Consequently, CM-I is associated with hydrocephalus and symptoms involving compression of the cervicomedullary junction by ectopic tonsils. Several studies have reported the clinical symptoms associated with CM-I, including suboccipital headache, weakness in the upper extremities, facial numbness, loss of temperature sensation, ataxia, diplopia, dysarthria, dysphagia, vomiting, vertigo, nystagmus, and tinnitus. Syncope is one of the rarest presentations in patients with CM-I. There are many hypotheses regarding the causes of syncope in patients with CM-I; however, the mechanisms are not clearly understood. Although surgical decompression for CM-I in patients with syncope has yielded good clinical results in some studies, such cases are rarely reported. We report a case of orthostatic syncope in a patient with CM-I who was treated with surgical intervention.
- Introduction
- Introduction
Chiari malformation is a congenital anomaly of the hindbrain. Chiari malformation type I (CM-I), the most common, is characterized by herniation of cerebellar tonsils through the foramen magnum1). CM-I is defined as cerebellar tonsilar herniation 3 to 5 mm below the level of the foramen magnum2). Consequently, CM-I is associated with hydrocephalus and symptoms with compression of the cervicomedullary junction by ectopic tonsils3). There are many reports on clinical symptoms associated with CM-I, including suboccipital headache, weakness in upper extremities, facial numbness, loss of temperature sensation, ataxia, diplopia, dysarthria, dysphagia, vomiting, vertigo, nystagmus, and tinnitus1,4,5). There are only a few reports of syncope associated with CM-I6). Various pathophysiological mechanisms such as compression of the midbrain ascending reticular system and vertebrobasilar artery have been reported. Also, hypotension secondary to cardiorespiratory center have been proposed, however, the exact cause of CM-I related syncope is still not well understood7).We report on a case of orthostatic syncope in a patient with CM-I who was treated with surgical intervention.
- Case report
- Case report
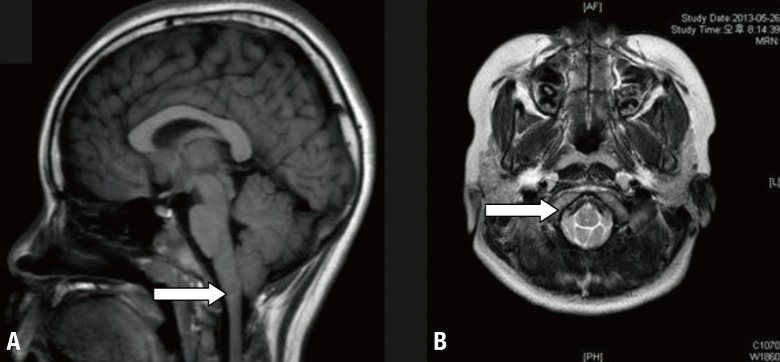
An 11-year-old girl, with no birth history and no history of significant illness, was admitted to our clinic for evaluation of 5 episodes of syncope. She presented with her first syncopal episode at the age of 9. During a 2-year period, she experienced five episodes of syncope. The symptoms occurred while she was walking and while bending her head back during hot showers, which were preceded by dizziness, nausea, and blackout and followed by fatigue, headache. Duration of unconsciousness in each episode was less than 1 minute. These episodes caused her traumatic injury and recovery from symptoms took approximately 1 hour.Her neurologic examination was normal. Initial routine work-up including laboratory test, chest X-ray, and electrocardiogram was not remarkable. Head up tilt test was done after lying on a bed in a recumbent position quietly at least for 10 minutes. Then table was tilted from the resting recumbent position to 70° head-up. She showed reduction of systolic and diastolic blood pressure within three minutes in head up tilt test from 120/59 mmHg to 76/39 mmHg with dizziness and nausea (Table 1).She was diagnosed as orthostatic hypotension. However, due to frequent episodes and traumatic injury caused by loss of consciousness despite medical treatment with midodrine, further evaluation of electroencephalography (EEG) and brain magnetic resonance imaging (MRI) were performed. EEG was normal. However, brain MRI demonstrated a 5-mm herniation of the cerebellar tonsils consistent with a diagnosis of CM-I (Fig. 1). After 6 months, due to repetitive traumatic syncopal episodes refractory to medication therapy, the patient was referred to a neurosurgeon and posterior fossa decompression was performed. Six months after surgery, she remained asymptomatic.
- Discussion
- Discussion
Orthostatic hypotension is defined as a reduction of systolic blood pressure >20 mmHg or diastolic blood pressure >10 mmHg within 3 minutes of standing up or head tilt to >60°8). Neurogenic orthostatic hypotension can be caused by other conditions that induce autonomic dysfunction, such as Guillain-Barre syndrome, familial dysautonomia, and as a secondary aspect of systemic disease. Postural syncope is caused by systemic hypotension, and reduced cerebral blood flow. These diseases lead to autonomic failure caused by inadequate release of norepinephrine.A nonpharmacologic option, such as avoiding rapid changes of body position from supine to standing and increasing water and salt intake, is the first choice for treatment of syncope9). Agents such as fludrocortisone, midodrine, and selective serotonin reuptake inhibitors may also be helpful. Treatment also includes correcting reversible causes and discontinuing responsible medications10).Brain imaging is not required for uncomplicated cases of syncope. However, for conditions incorrectly diagnosed as syncope, including epilepsy, vertebrobasilar transient ischemic attack, neuroimaging studies have to be considered in unusual cases.This patient was diagnosed as orthostatic syncope by head up tilt test. However, as she showed complete loss of consciousness in specific situations, such as bending her neck, Valsalva maneuver, we had to consider vascular lesions in the central nervous system.Symptoms occurring in patients with CM-I are believed to result from relatively narrow posterior fossa due to displacement of the inferior tonsil of the cerebellum. However, not only the descending cerebellar tonsil, but developmental bony anomalies itself was also attributed to narrow posterior fossa space in patients with CM-I. Straus D et al.11) reported that approximately 50% of patients with atlanto-occipital assimilation have CM-I.Syncope is one of the rarest presentations in patients with CM-I patients. Some authors have reported that syncope presents as a symptom in only 3% of CM-I patients12). Classically, patients with CM-I present with pain, weakness, sensory loss, dizziness, gait disturbances, and cranial nerve palsies.Numerous hypothetical pathophysiological mechanisms explaining orthostatic syncope in patients with CM-I, such as dysautonomia, vertebral insufficiency causing transient ischemia and syncope and transient ascending reticular activating system dysfunction have been proposed. Some authors reported that among seven CM-I patients with syncope, only 3 patients had a positive tilt table tilt test. However, although the tilt test is used in diagnosis of neurogenic orthostatic hypotension, there is no gold standard test for diagnosis of neurogenic orthostatic hypotension11).There are some reports of patients with severe respiratory dysfunction, orthopnea, and cough with syncope11). Central apnea can be explained by similar hypothetic mechanisms of compression of the ascending reticular system, which is improved by decompressive surgery.Although decompression of CM-I in patients with syncope has led to good clinical results in some reports, reported cases of surgical treatment in patients with syncope and CM-I are rare.Because we report good clinical outcome of surgical treatment in patients with CM-I presenting with syncope, we suggest that clinicians have to consider central nervous system evaluation in patients with severe orthostatic syncope despite the low incidence rate.
- Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
- References
- 1. Dones J, De Jesús O, Colen CB, Toledo MM, Delgado M. Clinical outcomes in patients with Chiari I malformation: a review of 27 cases. Surg Neurol 2003;60:142–147.
[Article] [PubMed]2. Mueller DM, Oro' JJ. Prospective analysis of presenting symptoms among 265 patients with radiographic evidence of Chiari malformation type I with or without syringomyelia. J Am Acad Nurse Pract 2004;16:134–138.
[Article] [PubMed]3. Tarani L, Del Balzo F, Costantino F, Properzi E, D'Eufemia P, Liberati N, et al. Chiari type I malformation, syncope, headache, hypoglycemia and hepatic steatosis in an 8-year old girl: a causal association? Pediatr Rep 2010;2:e8
[Article] [PubMed] [PMC]4. Bindal AK, Dunsker SB, Tew JM Jr. Chiari I malformation: classification and management. Neurosurgery 1995;37:1069–1074.
[Article] [PubMed]5. Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, et al. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 1999;44:1005–1017.
[Article] [PubMed]6. Prilipko O, Dehdashti AR, Zaim S, Seeck M. Orthostatic intolerance and syncope associated with Chiari type I malformation. J Neurol Neurosurg Psychiatry 2005;76:1034–1036.
[Article] [PubMed] [PMC]7. Garland EM, Robertson D. Chiari I malformation as a cause of orthostatic intolerance symptoms: a media myth? Am J Med 2001;111:546–552.
[Article] [PubMed]8. Stewart JM. Update on the theory and management of orthostatic intolerance and related syndromes in adolescents and children. Expert Rev Cardiovasc Ther 2012;10:1387–1399.
[Article] [PubMed] [PMC]9. Lahrmann H, Cortelli P, Hilz M, Mathias CJ, Struhal W, Tassinari M. EFNS guidelines on the diagnosis and management of orthostatic hypotension. Eur J Neurol 2006;13:930–936.
[Article] [PubMed]10. Medow MS, Stewart JM, Sanyal S, Mumtaz A, Sica D, Frishman WH. Pathophysiology, diagnosis, and treatment of orthostatic hypotension and vasovagal syncope. Cardiol Rev 2008;16:4–20.
[Article] [PubMed]
Fig. 1
Brain magnetic resonance iamging findings. (A) The arrow shows downward displacement of the cerebellar tonsil by approximately 5 mm, consistent with Chiari malformation type I. (B) The arrow shows brain stem in the center of the foramen magnum which is not circular due to compression by the tonsil.

 About
About Browse articles
Browse articles For contributors
For contributors
