All issues > Volume 59(Suppl 1); 2016
Congenital miliary tuberculosis in an 18-day-old boy
- Corresponding author: Young Yoo, MD. Department of Pediatrics, Korea University Anam Hospital, 73 Inchon-ro, Seongbuk-gu, Seoul 02841, Korea. Tel: +82-2-920-5090, Fax: +82-2-922-7476, yoolina@korea.ac.kr
- Received April 14, 2015 Revised April 14, 2015 Accepted May 15, 2015
- Abstract
-
Congenital tuberculosis (TB) is a rare disease that is associated with high mortality. Mycobacterium tuberculosis, the causative agent, may be transmitted from the infected mother to the fetus by the transplacental route or by aspiration of infected amniotic fluid. Clinical symptoms and signs are not specific. Miliary patterns are the most common findings in the chest X-rays of many infants with congenital TB. In this case, an 18-day-old boy had jaundice on the fifth day of birth, and fever and respiratory distress appeared on the 18th day. Chest X-ray showed diffuse fine bilateral infiltration. Clinically, pneumonia or sepsis was suspected. Respiratory symptoms and chest X-ray findings worsened despite empirical antibiotic therapy. The lungs showed miliary infiltration suggestive of TB. Gastric aspirates were positive for M. tuberculosis. Respiratory distress and fever were gradually improved after anti-TB medication. Congenital TB is difficult to detect because of minimal or no symptoms during pregnancy and nonspecific symptoms in neonates. Hence, clinicians should suspect the possibility of TB infection even if neonates have non-specific symptoms. Early diagnosis and meticulous treatment are required for the survival of neonates with TB.
- Introduction
- Introduction
Congenital tuberculosis (TB) is a rare disease but has a mortality of up to 44%1). Hematogenous spread of Mycobacterium tuberculosis from the infected mother to the fetus during pregnancy or aspiration of infected amniotic fluid leads to congenital TB2). The number of TB patients is notable in women of reproductive age in Korea3). Since most of the pregnant women who have active TB are symptomless, diagnosis of TB is usually delayed2,4). Congenital TB present with nonspecific signs and symptoms, such as fever, lethargy, respiratory distress, and hepatosplenomegaly, at 2–3 weeks of age. Nonspecific clinical manifestations make it difficult to distinguish TB from bacterial sepsis or intrauterine viral infection. Thus, high suspicion is needed for early diagnosis and meticulous treatment. Miliary patterns are common imaging finding in many infants with congenital TB1). The prognosis is fair after proper anti-TB treatment2). We present herein a neonate with congenital miliary TB who had fever and respiratory distress in the first few weeks of life.
- Case report
- Case report
An 18-day-old boy was admitted to Korea University Anam Hospital with a 1-day history of fever and tachypnea. On physical examination, his body temperature was 38.2℃, and heart rate 180 beats/min. He had a mild degree of respiratory distress with a respiratory rate of 62 breaths/min. Breathing sounds were smooth, and no crackles or wheezing were audible through both lung fields. He was born to a Chinese mother at 37 weeks of gestation and weighing 3,800 g by vaginal delivery. One week prior to admission, he had jaundice but improved after a 4-day course of photo-therapy. Venous blood gas analysis showed pH, 7.429; PCO2, 32.2 mmHg; PO2, 43.5 mmHg; HCO3, 21.5 mmol/L; base excess, −1.8 mmol/L. The complete blood count showed hemoglobin, 9.6 g/dL; white blood cells, 16,500/mm3 with segmented neutrophils of 53.9%; and platelets, 520,000/mm3. C-reactive protein (CRP) level was 7.22 mg/L. Liver function tests showed normal levels of aspartate aminotransferase (19 IU/L) and alanine aminotransferase (9 IU/L). Chest X-ray revealed diffuse fine infiltration in both lung fields (Fig. 1A).After admission, fever persisted and respiratory distress worsened with moderate chest-wall retraction, dyspnea, and tachypnea. Follow-up chest X-ray showed numerous interstitial nodules throughout both lungs (Fig. 1B). Neonatal sepsis or pneumonia was suspected, and empirical intravenous antibiotic therapy was started. However, he was still febrile, and the CRP level increased up to 123.3 mg/L. His chest computed tomography demonstrated numerous fine nodules in the entire lung (Fig. 2).Blood, urine, and cerebrospinal fluid (CSF) cultures were negative for bacteria and fungi. No virus was detected in the polymerase chain reaction (PCR) of nasopharyngeal aspirates, urine, and CSF. Despite broad-spectrum antibiotic therapy and supportive care, respiratory distress continued to worsen over the next 48 hours, and chest X-ray infiltration did not improve.Based on the poor response to the conventional management of pneumonia, other etiologies, such as pulmonary TB, viral intrauterine infection, atypical or aspiration pneumonia were suspected. The tuberculin skin test (TST) was negative with an induration of 0 mm, but PCR and culture of gastric aspirates were positive for M. tuberculosis. The screening test results were negative for atypical pneumonia and viral intrauterine infection. No M. tuberculosis was detected in urine or CSF. We stopped intravenous antibiotic therapy and started a combination therapy of isoniazid, rifampicin, pyrazinamide, and ethambutol along with an oral corticosteroid. The respiratory distress gradually improved, and his body temperature returned to normal after TB treatment.His mother was screened for TB. She is Chinese and did not receive bacillus Calmette-Guerin vaccination. She had a few days' history of fever and mild cough during the second trimester of pregnancy. The TST was positive with an induration of 15 mm and chest X-ray showed focally increased opacity in the left upper lung and small amounts of pleural effusion in the right thoracic cavity. Bronchoscopy detected no M. tuberculosis. A combination anti-TB therapy of isoniazid, rifampin, pyrazinamide and ethambutol was started.Further work-up results of 2-dimensional echocardiogram, abdominal sonography, and brain magnetic resonance imaging for congenital TB were no additional information. Two weeks after anti-TB medication, the respiratory distress completely disappeared. After 8 months, chest X-ray showed remarkably resolved lung infiltration (Fig. 3). The patient and his mother were well with no symptoms or signs suggesting TB.
- Discussion
- Discussion
TB remains a significant public health problem in Korea3) and worldwide2). A notable prevalence of TB in women of child-bearing age is reported5,6). TB during pregnancy increases the occurrence of preterm labor, low birth weight, and stillbirth7). Neonatal TB can be transmitted either congenitally by acquisition in utero or neonatally by postnatal direct contact. Congenital TB is considered an intrauterine infection with M. tuberculosis by hematogenous spread through the umbilical vein or by ingestion of infected amniotic fluid2). Disseminated miliary and meningeal forms of TB occur frequently in congenital TB, which may be attributed to the intrinsic immaturity of the immune system8). The negative TST result and nonspecific clinical manifestations make it difficult to diagnose TB in many infected neonates2),8). It is also difficult to suspect TB in pregnant women due to nonspecific nature of symptoms and reluctance to undergo radiography during pregnancy9). Thus, many mothers are only diagnosed as having TB following diagnosis in their babies as in our case. Pregnant women should be clinical screening for TB during routine prenatal examination10).Clinical signs and symptoms of congenital TB usually develop at 2–3 weeks of age, which include fever, respiratory distress, hepatosplenomegaly, or feeding problems as seen in other neonatal infections1). TB should be suspected and examined if; (1) neonates do not respond to conventional treatment for pneumonia or sepsis, particularly in those born to nonvaccinated mothers, (2) mothers are diagnosed as having TB and their babies have nonspecific symptoms, and (3) neonates have unexplained fever and hepatosplenomegaly at 2–3 weeks of age11). Diagnosis of congenital TB in neonates is based on the TST result, which is often negative, chest X-ray, and other radiologic study results if symptoms are suggestive of TB. Microbiological specimens such as gastric aspirate, ascitic fluid, endotracheal aspirate and CSF should be obtained for the detection of M. tuberculosis12).In our case, after the boy was diagnosed as having miliary TB, his mother was also diagnosed as having TB. His mother had fever and cough for a few days during the second trimester, but she was not suspected of having TB at that time. We did not perform endometrial biopsy from his mother for definite diagnosis of congenital TB. However, it is thought that the patient's TB was transmitted by hematogenous spread rather than by postnatal contact because AFB staining of bronchial aspirates from his mother was negative for M. tuberculosis. In our case, AFB staining for M. tuberculosis was positive in gastric aspirates but negative in CSF. Fever and other respiratory distress signs were gradually improved after anti-TB treatment. Complications of late treatment of congenital miliary TB include meningitis, otitis media, seizures, deafness, and death.If congenital TB is left untreated or its treatment is delayed, it may result in fatal outcome1,2). Without doubt, early detection and appropriate administration of antituberculous therapy influence the outcome of TB in neonates. Skevaki and Kafetzis2) have recommended a standard 2-month treatment course of 4 drugs, followed by a 4- to10-month treatment course of 2 drugs for complete recovery of congenital TB. Corticosteroids are recommended in cases of TB meningitis, miliary TB, and endobronchial TB with accompanied obstruction8). Although the optimal duration of therapy has not yet been established, many experts treat infants with congenital TB for 9 to 12 months because of a low immunologic function in young infants.We reported a favorable case of congenital miliary TB whose mother had pulmonary TB and who recovered after anti-TB treatment. Congenital TB is extremely rare and difficult to diagnose due to minimal symptoms in neonates. Clinicians should suspect TB infection if neonates have nonspecific symptoms. Early diagnosis and meticulous treatment are required for the survival of neonates with congenital TB.
- Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
- References
- 1. Peng W, Yang J, Liu E. Analysis of 170 cases of congenital TB reported in the literature between 1946 and 2009. Pediatr Pulmonol 2011;46:1215–1224.
[Article] [PubMed]2. Skevaki CL, Kafetzis DA. Tuberculosis in neonates and infants: epidemiology, pathogenesis, clinical manifestations, diagnosis, and management issues. Paediatr Drugs 2005;7:219–234.
[Article] [PubMed]3. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korean guidelines for tuberculosis. 2nd ed. Cheongju: Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention, 2014.4. Diar H, Velaphi S. Congenital tuberculosis as a proxy to maternal tuberculosis: a case report. J Perinatol 2009;29:709–711.
[Article] [PubMed]5. Cantwell MF, Shehab ZM, Costello AM, Sands L, Green WF, Ewing EP Jr, et al. Brief report: congenital tuberculosis. N Engl J Med 1994;330:1051–1054.
[Article] [PubMed]6. Llewelyn M, Cropley I, Wilkinson RJ, Davidson RN. Tuberculosis diagnosed during pregnancy: a prospective study from London. Thorax 2000;55:129–132.
[Article] [PubMed] [PMC]7. Ormerod P. Tuberculosis in pregnancy and the puerperium. Thorax 2001;56:494–499.
[Article] [PubMed] [PMC]8. Whittaker E, Kampmann B. Perinatal tuberculosis: new challenges in the diagnosis and treatment of tuberculosis in infants and the newborn. Early Hum Dev 2008;84:795–799.
[Article] [PubMed]9. Nakbanpot S, Rattanawong P. Congenital tuberculosis because of misdiagnosed maternal pulmonary tuberculosis during pregnancy. Jpn J Infect Dis 2013;66:327–330.
[Article] [PubMed]10. Chanta C, Jariyapongpaibul Y, Triratanapa K. Congenital tuberculosis presenting as sepsis syndrome. J Med Assoc Thai 2004;87:573–577.
[PubMed]
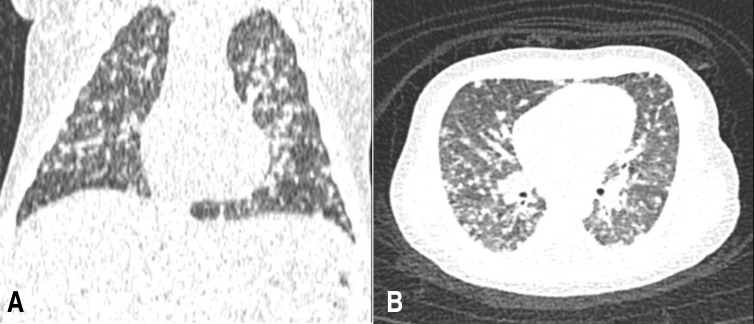
Fig. 1
Chest X-ray shows fine scanty nodules in both the lungs on the first day of hospitalization (A) and numerous interstitial nodules throughout both the lungs on the next day (B).


 About
About Browse articles
Browse articles For contributors
For contributors