All issues > Volume 55(9); 2012
The use of ketogenic diet in special situations: expanding use in intractable epilepsy and other neurologic disorders
- Corresponding author: Munhyang Lee, MD, PhD. Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 135-710, Korea. Tel: +82-2-3410-3539, Fax: +82-2-3410-0043, mhlee091@skku.edu
- Received June 15, 2012 Accepted July 24, 2012
- Abstract
-
The ketogenic diet has been widely used and proved to be effective for intractable epilepsy. Although the mechanisms underlying its anti-epileptic effects remain to be proven, there are increasing experimental evidences for its neuroprotective effects along with many researches about expanding use of the diet in other neurologic disorders. The first success was reported in glucose transporter type 1 deficiency syndrome, in which the diet served as an alternative metabolic source. Many neurologic disorders share some of the common pathologic mechanisms such as mitochondrial dysfunction, altered neurotransmitter function and synaptic transmission, or abnormal regulation of reactive oxygen species, and the role of the ketogenic diet has been postulated in these mechanisms. In this article, we introduce an overview about the expanding use and emerging trials of the ketogenic diet in various neurologic disorders excluding intractable epilepsy and provide explanations of the mechanisms in that usage.
- Introduction
- Introduction
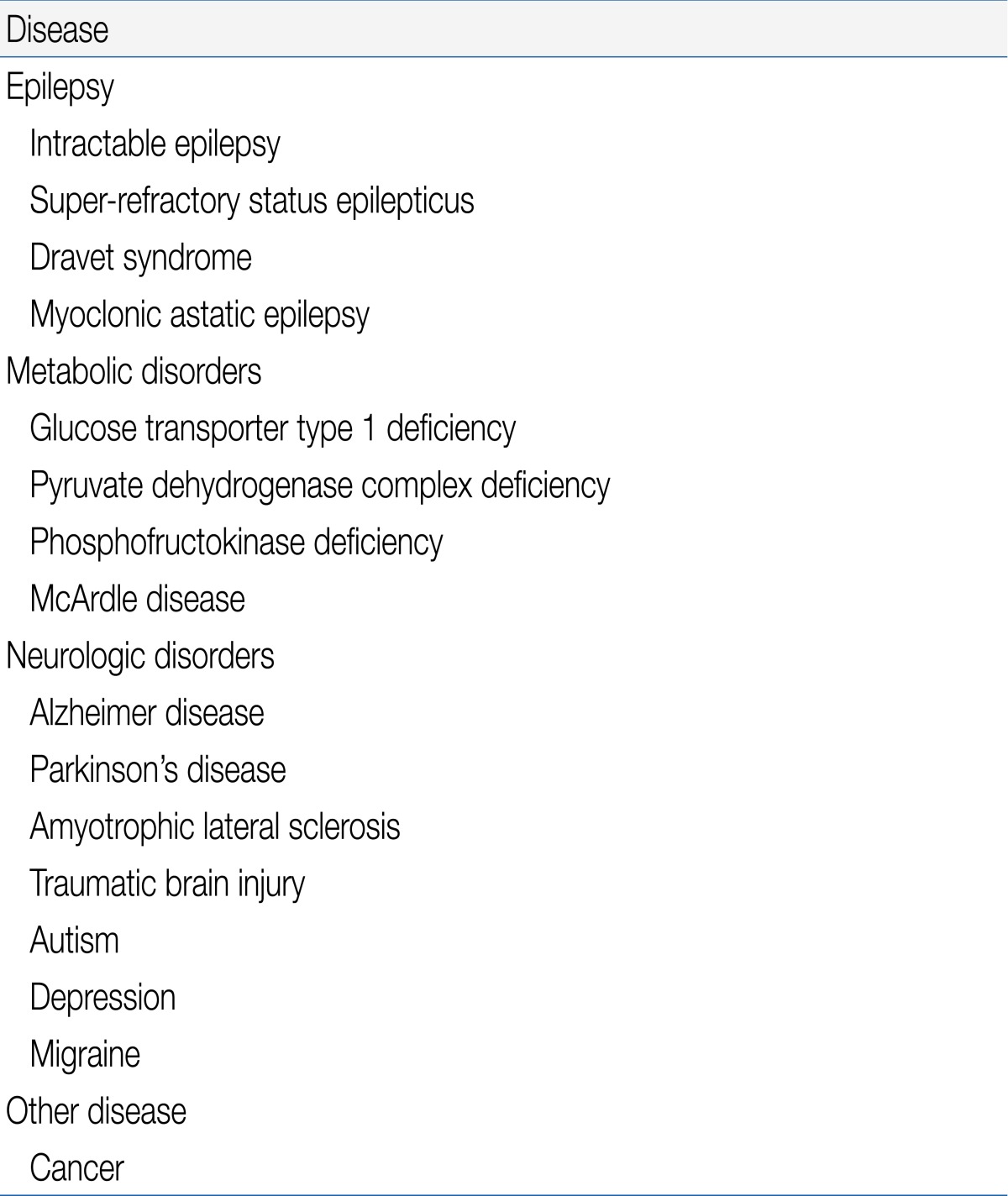
The ketogenic diet was first introduced in the 1920s from the observation that starvation resulted in a decrease of seizure frequency1). The diet became less popular after the appearance of antiepileptic drugs such as diphenylhydantoin and phenobarbital. However, the ketogenic diet reappeared after one of well-known broadcasting company aired a program on the treatment of epilepsy using it1). Since then, many researches have proven the efficacy of the ketogenic diet in intractable epilepsy of adults and pediatric patients including infants2-6).There have been several hypotheses about the mechanisms of antiepileptic effects by the ketogenic diet and some are described as follows7-10): the ketogenic diet alters the energy metabolism in the brain, therefore altering brain excitability; it leads to changes in cell (neuronal and perhaps glial) properties thereby reducing excitability; it enhances alterations in synaptic transmission; it is associated with changes in a variety of circulating factors which act as neuromodulators that can regulate central nervous system excitability; and it alters the extracellular environment of the brain, which helps to decrease the neuronal excitability and synchrony10).The main stream of those proposed mechanisms of ketogenic diet is that it changes the normal metabolism of neurons, resulting in varying neuronal excitability and plasticity, as well as modifying neural circuits and cellular properties to enhance and normalize neuronal function. From this point of view, the ketogenic diet can be applied to various neurologic disorders other than epilepsy. An alternative use of the ketogenic diet has been tried in various conditions (Table 1). This review will cover the areas of established evidence and dietary treatments in neurologic disorders other than epilepsy and summarize the clinical researches to date.
- Use of ketogenic diet in metabolic disorders
- Use of ketogenic diet in metabolic disorders
- 1. GLUT1 deficiency syndrome
- 1. GLUT1 deficiency syndrome
GLUT1 deficiency syndrome (OMIM #606777) is a disease of cerebral energy metabolism caused by impaired GLUT1 mediated glucose transport into the brain14). It was first reported from the observation of low cerebrospinal glucose concentration (hypoglycorrhachia) with low cerebrospinal fluid lactate and normoglycemia as the diagnostic criteria. GLUT1 deficiency syndrome is characterized by an infantile-onset epileptic encephalopathy, mental retardation, deceleration of head growth, acquired microcephaly, incoordination, and spasticity. A defect in glucose transport across the blood-brain barrier is the major pathomechanism15,16).Currently, the ketogenic diet is regarded as the sole treatment method. The concept of maintaining ketosis in GLUT1 deficiency syndrome is clear in the treatment of the disease; the early restoration of brain energy metabolism by supplying ketones as an alternative fuel benefits both the seizure control and development17). Brain energy metabolism is unique especially in infancy when 80% of glucose is consumed by the brain. Additionally, the ability of the brain to extract and utilize ketone bodies in infancy is four times higher than in adults and the effect of the ketogenic diet is most effective between 2 to 5 years of age17,18). In one prospective study, fifteen patients with GLUT1 deficiency syndrome were treated with the ketogenic diet for 2 to 5.5 years. As a result, two-thirds of the patients who were on the ketogenic diet without antiepileptic drugs were found seizure-free. The others showed remarkable seizure reduction with add-on drugs. There were no serious adverse effects, and the parental satisfaction with the ketogenic diet was high19). There have been continuing reports about the successful use of the ketogenic diet or modified Atkins diet in the treatment of GLUT1 deficiency syndrome20-22).- 2. PDHC deficiency
- 2. PDHC deficiency
Mitochondrial PDHC catalyzes the rate-limiting step in the aerobic glucose oxidation and it comprises multiple copies of three enzymatic subunits: pyruvate dehydrogenase (E1), dihydrolipoamide transacetylase (E2), and dihydrolipoamide dehydrogenase (E3), as well as an E3 binding protein. Patients with PDHC deficiency manifest poor feeding, lethargy, and tachypnea in early infancy, developmental delay, growth retardation, intractable seizures, ataxia, episodic dystonia, and abnormal eye movements23). Although there have been no controlled trials that have prospectively evaluated the ketogenic diet in the treatment of PDHC deficiency, there have been several case reports with some success23-25). The use of the ketogenic diet bypasses the metabolic block, by providing a direct source of acetyl-CoA, leading to amelioration of some symptoms23).- 3. Mitochondrial disorders
- 3. Mitochondrial disorders
There has been increasing evidence showing that the ketogenic diet enhances mitochondrial functioning and biogenesis9,26,27). During short-term fasting, the ratio of glucose to ketones in the brain can shift to 70:30, and during prolonged starvation, it may shift to 30:70. During the ketogenic diet, the brain utilizes the ketone body as a major fuel and this reduces oxidative stress and increases antioxidant enzymes28). This is the result of shifting of metabolism from the glucose-based state to a more fatty acid oxidation-based mitochondrial metabolism28,29). According to a previous study, the ketogenic diet was safe and effective in 14 pediatric patients with mitochondrial defect in complexes I, II, and IV, all of whom had intractable epilepsy30). In that study, half of the patients became seizure-free with the ketogenic diet. However, the ketogenic diet is not recommended for patients with primary carnitine deficiencies including carnitine palmitoyl transferase deficiencies I or II and mitochondrial translocase and fatty acid beta-oxidation abnormalities9,31). The reason for this is that the defect of those enzymes prevents introducing the fatty acid into the mitochondria.- 4. Other metabolic disorders
- 4. Other metabolic disorders
The use of the ketogenic diet was demonstrated in other rare metabolic disorders. One is phosphofructokinase deficiency. Phosphofructokinase is the rate limiting enzyme in glycolysis for the conversion of fructose-6-phosphate to fructose-1, 6-bisphosphate. There was one case report, in which the patient with phosphofructokinase deficiency showed a marked gain in muscle strength and improvement in development after treatment with the ketogenic diet11,32). Another example is glycogenosis type V (McArdle disease) which is caused by a defect in the muscle-specific isoenzyme of glycogen phosphorylase. In healthy individuals, glycogen gets decomposed into glucose for use as a fuel in muscles. When the ketogenic diet was applied to a patient with the disorder, providing an alternative source of energy production, the patient's exercise tolerance improved11,33).
The ketogenic diet has been used in various metabolic disorders9,11,12). The most strongly suggested mechanism of action is providing an alternative method for some metabolic disorders such as glucose transporter type 1 (GLUT1) deficiency syndrome and pyruvate dehydrogenase complex (PDHC) deficiency9,11). Also, another possible explanation is that the ketogenic diet reduces oxidative stress induced by reactive oxygen and nitrogen species. One example is that the diet activates an adaptive pathway by enhancing the glutathione antioxidant system via a protective transcription factor, NF E2-related factor 213).
- Use of ketogenic diet in epilepsy for expanding uses
- Use of ketogenic diet in epilepsy for expanding uses
- 1. Dravet syndrome
- 1. Dravet syndrome
Dravet syndrome (OMIM #607208) is an infantile-onset catastrophic epilepsy and its prevalence is estimated at about 1 in 20,000 to 40,000 children with male preponderance38). Patients show normal development initially and experience febrile and afebrile generalized tonic-clonic seizures before one year of age. Some patients manifest various type of seizures; focal, absence, and myoclonus. Additionally, they show developmental delay, ataxia, and recurrent status epilepticus38). Dravet syndrome is due to genetic defect in the SCN1A, SCN2A, SCN9A and GABRG2 genes39).The first large study using the ketogenic diet to Dravet syndrome was reported in 2005. The study included 52 patients who met the diagnostic criteria for Dravet syndrome. Twenty patients were given the diet and thirteen continued on the diet for at least one year. There was more than 75% reduction in seizures in ten children with two who became seizure-free40). Other studies have also reported similar results41,42). A prospective study was done with 15 Dravet syndrome patients who received stiripentol, clobazam, and valproate for more than six months while being on the ketogenic diet. Ten patients showed more than 75% seizure reduction and one patient became seizure-free at three months into the study period. Five patients continued to show more than 75% seizure reduction at one year. Additionally, 56% of the patients revealed an improvement in hyperactivity and inattention and 28% of them in impulsivity and aggression43).- 2. MAE
- 2. MAE
MAE was first described by Doose et al.44) in 1970. It is characterized by a combination of seizure types including myoclonic, myoclonic-atonic, or atonic seizures between the ages of seven months and six years. Patients also have absence, clonic, generalized tonic clonic seizures, and frequent status epilepticus and are usually refractory to medical treatments37,45).Several studies have provided clinical evidence for using the ketogenic diet in MAE. Oguni et al.46) reported that myoclonic-atonic seizures stopped in 89% of the patients within 1 to 3 years while generalized tonic clonic or clonic seizures persisted. According to the study by Laux et al.47), seven of ten patients with MAE showed excellent outcome of being seizure free or >90% seizure reduction with the ketogenic diet37). Another prospective study assessed the efficacy of the ketogenic diet in patients with MAE. The study included 11 patients treated with the ketogenic diet for at least 18 months. A total of six patients remained on the diet and two patients became seizure free and another two showed more than 75% seizure reduction. All of these studies showed the effectiveness of the ketogenic diet in MAE.- 3. Super-refractory status epilepticus
- 3. Super-refractory status epilepticus
Super-refractory status epilepticus is defined as status epilepticus that continues or recurs for 24 hours or more after the onset of anaesthetic therapy, including those cases that recur on the reduction or withdrawal of anaesthesia35). Super-refractory status epilepticus is not uncommonly encountered in the neuro-intensive care unit. Retrospective studies have shown that 12 to 43% of the cases with status epilepticus became refractory35,48,49). In the study of Holtkamp et al.48), 20% of the patients recurred within five days of tapering the anaesthetic agent and in all other studies, at least 50% of those requiring anaesthesia became super-refractory. It can be estimated that approximately 15% of all cases of status epilepticus admitted to the hospital will become super-refractory35).The use of the ketogenic diet in super-refractory status epilepticus have mostly been reported in children. The first report was conducted with six children with super-refractory status epilepticus responding to the diet. In 2010, Nabbout et al.50) reported that nine children with super-refractory status epilepticus responded to the diet and the patients were regarded as having fever induced refractory epileptic encephalopathy in school age children. Recently, Nam et al.36), reported the successful use of the ketogenic diet in five patients with super-refractory status epilepticus.- 4. Mechanisms of ketogenic diet showing anti-epileptic activity
- 4. Mechanisms of ketogenic diet showing anti-epileptic activity
Ketosis has been regarded as the key feature of the ketogenic diet, and the proposed hypotheses for anti-epileptic activity of the ketogenic diet are as follows: 1) change in the nature and degree of energy metabolism in the brain, 2) change in neuronal cellular properties, and 3) change in neurotransmitter function and synaptic transmission10). The efficacy of the ketogenic diet develops gradually over a period of 1 to 3 weeks, suggesting that adaptive changes in gene expression are involved in its anticonvulsant effects51,52). In an animal study, an up-regulation of transcripts encoding energy metabolism enzymes and a 46% increase in the density of mitochondria were observed in the neuronal processes. Additionally, an increased phosphocreatine: creatine energy-store ratio was found, which indicated increased energy reserves. The hippocampal synaptic transmission in the ketogenic diet-fed animals was maintained for more than 50% longer than the controls after exposure to a metabolic stressor, suggesting that the brain tissue became more resistant to the metabolic stressor52). Bough52) postulated that the observed ketogenic diet-induced production of energy metabolism compensates for the interictal metabolic deficits within epileptic foci and transient failures of gamma-aminobutyric acid-ergic inhibition.
There has been a great amount of evidence that the ketogenic diet is effective in various intractable epilepsy syndromes. Recently, some studies proposed the proofs for the treatment of specific intractable epilepsy syndromes such as Dravet syndrome, myoclonic astatic epilepsy (MAE), and refractory status epilepticus34-37).
- Use of ketogenic diet in other neurologic disorders
- Use of ketogenic diet in other neurologic disorders
- 1. The ketogenic diet in Alzheimer's disease
- 1. The ketogenic diet in Alzheimer's disease
The major pathological mechanism of Alzheimer's disease is neuronal degeneration with accumulation of abnormal cellular products such as fibrillary plaques and tangles. According to a recent observation, an alteration in the function of extant neural circuits and mitochondrial homeostasis may have a pathologic role in Alzheimer's disease9,53). Therefore, the hypothesis that the ketogenic diet might produce beneficial effects to patients with Alzheimer's disease was introduced54). The results of the clinical studies have been controversial. A randomized double-blind, placebo-controlled trial of a medium chain triglyceride based ketogenic diet showed significant improvement of cognitive function in APOε4-negative patients with Alzheimer's disease. The researchers postulated that the results may be due to improved mitochondrial function, since ketone bodies have the capability to protect against the toxic effects of beta amyloid on neurons in cultured cells55,56). In a recent animal study, the infusion of 2-deoxy-D-glucose, a compound known to induce ketogenesis to female triple transgenic mouse model of Alzheimer's disease, resulted in a shift towards a non-amyloidogenic status and maintenance of mitochondrial bioenergetics paralleled by simultaneous reduction in oxidative stress9,57). There is increasing evidence that the ketogenic diet may be effective for the treatment of Alzheimer's disease through various mechanisms that reduce oxidative stress and enhance mitochondrial function9). The age-associated differences in the production and use of ketones and its potential side effects need to be elucidated in future studies.- 2. The ketogenic diet in Parkinson's disease
- 2. The ketogenic diet in Parkinson's disease
The pathogenesis of Parkinson's disease involves excitotoxic degeneration of dopaminergic neurons residing in the substantia nigra, resulting in the abnormal movement, dysfunctions in cognition and other cortical functions. The impairment of mitochondrial complex I activity is hypothesized to play a role in the death of the dopaminergic neurons. It has been postulated that ketones could bypass complex I and provide an alternative fuel source. Also, enhancing mitochondrial function and increasing energy reserve might protect cells from various insults requiring high levels of energy9,11). There is one case series of Vanitallie et al.58) in which the ketogenic diet was provided to seven patients with Parkinson's disease; five of them completed the study and the scores for Unified Parkinson Disease Rating Scale decreased by 43.4%. With this result, future studies on the ketogenic diet in Parkinson's disease are expected.
The ketogenic diet is thought to enhance mitochondria function via many possible mechanisms. Considering the possible mitochondrial dysfunction in many neurodegenerative diseases, it can be possible to suitably adjust the ketogenic diet to the Alzheimer's disease or Parkinson disease.
- Conclusion
- Conclusion
The ketogenic diet is well established as an alternative therapy for intractable epilepsy, especially in pediatric patients. Recently, there has been increasing evidence for the use in specific intractable epilepsy syndromes such as Dravet syndrome, MAE, and super-refractory status epilepticus. The diet should be considered as primary therapy in GLUT1 deficiency and PDHC deficiency because it serves as an alternative metabolic source. Also, the ketogenic diet can be considered in the treatment of other metabolic disorders, Alzheimer's disease, other neurodegenerative disorders, although more evidence is required. The use of the ketogenic diet in various conditions is mainly based on the idea that alterations in metabolism may have a neuroprotective effect or changes in neuronal excitability as well as metabolic source. However, the exact mechanisms of action await further investigations; with those, the more expanding use of ketogenic diet will be possible in the future.
- References
- 2. Coppola G, Veggiotti P, Cusmai R, Bertoli S, Cardinali S, Dionisi-Vici C, et al. The ketogenic diet in children, adolescents and young adults with refractory epilepsy: an Italian multicentric experience. Epilepsy Res 2002;48:221–227.
[Article] [PubMed]3. Than KD, Kossoff EH, Rubenstein JE, Pyzik PL, McGrogan JR, Vining EP. Can you predict an immediate, complete, and sustained response to the ketogenic diet? Epilepsia 2005;46:580–582.
[Article] [PubMed]4. Payne NE, Cross JH, Sander JW, Sisodiya SM. The ketogenic and related diets in adolescents and adults--a review. Epilepsia 2011;52:1941–1948.
[Article] [PubMed]5. Nordli DR Jr, Kuroda MM, Carroll J, Koenigsberger DY, Hirsch LJ, Bruner HJ, et al. Experience with the ketogenic diet in infants. Pediatrics 2001;108:129–133.
[Article] [PubMed]6. Neal EG, Chaffe H, Schwartz RH, Lawson MS, Edwards N, Fitzsimmons G, et al. The ketogenic diet for the treatment of childhood epilepsy: a randomised controlled trial. Lancet Neurol 2008;7:500–506.
[Article] [PubMed]7. Hartman AL, Gasior M, Vining EP, Rogawski MA. The neuropharmacology of the ketogenic diet. Pediatr Neurol 2007;36:281–292.
[Article] [PubMed] [PMC]8. Bough KJ, Rho JM. Anticonvulsant mechanisms of the ketogenic diet. Epilepsia 2007;48:43–58.
[Article] [PubMed]9. Stafstrom CE, Rho JM. The ketogenic diet as a treatment paradigm for diverse neurological disorders. Front Pharmacol 2012;3:59
[PubMed] [PMC]10. Schwartzkroin PA. Mechanisms underlying the anti-epileptic efficacy of the ketogenic diet. Epilepsy Res 1999;37:171–180.
[Article] [PubMed]11. Baranano KW, Hartman AL. The ketogenic diet: uses in epilepsy and other neurologic illnesses. Curr Treat Options Neurol 2008;10:410–419.
[Article] [PubMed] [PMC]12. Kossoff EH, Zupec-Kania BA, Rho JM. Ketogenic diets: an update for child neurologists. J Child Neurol 2009;24:979–988.
[Article] [PubMed]13. Milder J, Patel M. Modulation of oxidative stress and mitochondrial function by the ketogenic diet. Epilepsy Res 2012;100:295–303.
[Article] [PubMed]14. De Vivo DC, Trifiletti RR, Jacobson RI, Ronen GM, Behmand RA, Harik SI. Defective glucose transport across the blood-brain barrier as a cause of persistent hypoglycorrhachia, seizures, and developmental delay. N Engl J Med 1991;325:703–709.
[Article] [PubMed]15. Wang D, Pascual JM, Yang H, Engelstad K, Jhung S, Sun RP, et al. Glut-1 deficiency syndrome: clinical, genetic, and therapeutic aspects. Ann Neurol 2005;57:111–118.
[Article] [PubMed]16. De Vivo DC, Leary L, Wang D. Glucose transporter 1 deficiency syndrome and other glycolytic defects. J Child Neurol 2002;17(Suppl 3): 3S15–3S23.
[Article] [PubMed]17. Klepper J, Leiendecker B, Bredahl R, Athanassopoulos S, Heinen F, Gertsen E, et al. Introduction of a ketogenic diet in young infants. J Inherit Metab Dis 2002;25:449–460.
[Article] [PubMed]18. Wheless JW. The ketogenic diet: Fa(c)t or fiction. J Child Neurol 1995;10:419–423.
[Article] [PubMed]19. Klepper J, Scheffer H, Leiendecker B, Gertsen E, Binder S, Leferink M, et al. Seizure control and acceptance of the ketogenic diet in GLUT1 deficiency syndrome: a 2- to 5-year follow-up of 15 children enrolled prospectively. Neuropediatrics 2005;36:302–308.
[Article] [PubMed]20. Pons R, Collins A, Rotstein M, Engelstad K, De Vivo DC. The spectrum of movement disorders in Glut-1 deficiency. Mov Disord 2010;25:275–281.
[Article] [PubMed]21. Veggiotti P, Teutonico F, Alfei E, Nardocci N, Zorzi G, Tagliabue A, et al. Glucose transporter type 1 deficiency: ketogenic diet in three patients with atypical phenotype. Brain Dev 2010;32:404–408.
[Article] [PubMed]22. Roulet-Perez E, Ballhausen D, Bonafe L, Cronel-Ohayon S, Maeder-Ingvar M. Glut-1 deficiency syndrome masquerading as idiopathic generalized epilepsy. Epilepsia 2008;49:1955–1958.
[Article] [PubMed]23. Patel KP, O'Brien TW, Subramony SH, Shuster J, Stacpoole PW. The spectrum of pyruvate dehydrogenase complex deficiency: clinical, biochemical and genetic features in 371 patients. Mol Genet Metab 2012;105:34–43.
[Article] [PubMed]24. Wexler ID, Hemalatha SG, McConnell J, Buist NR, Dahl HH, Berry SA, et al. Outcome of pyruvate dehydrogenase deficiency treated with ketogenic diets. Studies in patients with identical mutations. Neurology 1997;49:1655–1661.
[Article] [PubMed]25. Naito E, Ito M, Yokota I, Saijo T, Chen S, Maehara M, et al. Concomitant administration of sodium dichloroacetate and thiamine in west syndrome caused by thiamine-responsive pyruvate dehydrogenase complex deficiency. J Neurol Sci 1999;171:56–59.
[Article] [PubMed]26. Bough KJ, Wetherington J, Hassel B, Pare JF, Gawryluk JW, Greene JG, et al. Mitochondrial biogenesis in the anticonvulsant mechanism of the ketogenic diet. Ann Neurol 2006;60:223–235.
[Article] [PubMed]27. Kim do Y, Vallejo J, Rho JM. Ketones prevent synaptic dysfunction induced by mitochondrial respiratory complex inhibitors. J Neurochem 2010;114:130–141.
[Article] [PubMed] [PMC]28. Wallace DC, Fan W, Procaccio V. Mitochondrial energetics and therapeutics. Annu Rev Pathol 2010;5:297–348.
[Article] [PubMed] [PMC]29. Wallace DC. A mitochondrial paradigm of metabolic and degenerative diseases, aging, and cancer: a dawn for evolutionary medicine. Annu Rev Genet 2005;39:359–407.
[Article] [PubMed] [PMC]30. Kang HC, Lee YM, Kim HD, Lee JS, Slama A. Safe and effective use of the ketogenic diet in children with epilepsy and mitochondrial respiratory chain complex defects. Epilepsia 2007;48:82–88.
[Article]31. Kossoff EH, Rho JM. Ketogenic diets: evidence for short- and long-term efficacy. Neurotherapeutics 2009;6:406–414.
[Article] [PubMed] [PMC]32. Swoboda KJ, Specht L, Jones HR, Shapiro F, DiMauro S, Korson M. Infantile phosphofructokinase deficiency with arthrogryposis: clinical benefit of a ketogenic diet. J Pediatr 1997;131:932–934.
[Article] [PubMed]33. Busch V, Gempel K, Hack A, Müller K, Vorgerd M, Lochmüller H, et al. Treatment of glycogenosis type V with ketogenic diet. Ann Neurol 2005;58:341
[Article]34. Nabbout R, Vezzani A, Dulac O, Chiron C. Acute encephalopathy with inflammation-mediated status epilepticus. Lancet Neurol 2011;10:99–108.
[Article] [PubMed]35. Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain 2011;134(Pt 10): 2802–2818.
[Article] [PubMed]36. Nam SH, Lee BL, Lee CG, Yu HJ, Joo EY, Lee J, et al. The role of ketogenic diet in the treatment of refractory status epilepticus. Epilepsia 2011;52:e181–e184.
[Article] [PubMed]37. Nangia S, Caraballo RH, Kang HC, Nordli DR, Scheffer IE. Is the ketogenic diet effective in specific epilepsy syndromes? Epilepsy Res 2012;100:252–257.
[Article] [PubMed]39. Mastrangelo M, Leuzzi V. Genes of early-onset epileptic encephalopathies: from genotype to phenotype. Pediatr Neurol 2012;46:24–31.
[Article] [PubMed]40. Caraballo RH, Cersósimo RO, Sakr D, Cresta A, Escobal N, Fejerman N. Ketogenic diet in patients with Dravet syndrome. Epilepsia 2005;46:1539–1544.
[Article] [PubMed]41. Caraballo R, Vaccarezza M, Cersosimo R, Rios V, Soraru A, Arroyo H, et al. Long-term follow-up of the ketogenic diet for refractory epilepsy: multicenter Argentinean experience in 216 pediatric patients. Seizure 2011;20:640–645.
[Article] [PubMed]42. Kang HC, Kim YJ, Kim DW, Kim HD. Efficacy and safety of the ketogenic diet for intractable childhood epilepsy: Korean multicentric experience. Epilepsia 2005;46:272–279.
[Article] [PubMed]43. Nabbout R, Copioli C, Chipaux M, Chemaly N, Desguerre I, Dulac O, et al. Ketogenic diet also benefits Dravet syndrome patients receiving stiripentol: a prospective pilot study. Epilepsia 2011;52:e54–e57.
[Article] [PubMed]44. Doose H, Gerken H, Leonhardt R, Volzke E, Volz C. Centrencephalic myoclonic-astatic petit mal. Clinical and genetic investigation. Neuropadiatrie 1970;2:59–78.
[Article] [PubMed]45. Kelley SA, Kossoff EH. Doose syndrome (myoclonic-astatic epilepsy): 40 years of progress. Dev Med Child Neurol 2010;52:988–993.
[Article] [PubMed]46. Oguni H, Tanaka T, Hayashi K, Funatsuka M, Sakauchi M, Shirakawa S, et al. Treatment and long-term prognosis of myoclonic-astatic epilepsy of early childhood. Neuropediatrics 2002;33:122–132.
[Article] [PubMed]47. Laux LC, Devonshire KA, Kelly KR, Goldstein J, Nordli DR Jr. Efficacy of the ketogenic diet in myoclonic epilepsy of Doose. Epilepsia 2004;45(Suppl 7): 25148. Holtkamp M, Othman J, Buchheim K, Meierkord H. Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry 2005;76:534–539.
[Article] [PubMed] [PMC]49. Rossetti AO, Logroscino G, Bromfield EB. Refractory status epilepticus: effect of treatment aggressiveness on prognosis. Arch Neurol 2005;62:1698–1702.
[Article] [PubMed]50. Nabbout R, Mazzuca M, Hubert P, Peudennier S, Allaire C, Flurin V, et al. Efficacy of ketogenic diet in severe refractory status epilepticus initiating fever induced refractory epileptic encephalopathy in school age children (FIRES). Epilepsia 2010;51:2033–2037.
[Article] [PubMed]51. Appleton DB, DeVivo DC. An animal model for the ketogenic diet. Epilepsia 1974;15:211–227.
[Article] [PubMed]52. Bough K. Energy metabolism as part of the anticonvulsant mechanism of the ketogenic diet. Epilepsia 2008;49(Suppl 8): 91–93.
[Article] [PubMed] [PMC]53. Kapogiannis D, Mattson MP. Disrupted energy metabolism and neuronal circuit dysfunction in cognitive impairment and Alzheimer's disease. Lancet Neurol 2011;10:187–198.
[Article] [PubMed]54. Balietti M, Casoli T, Di Stefano G, Giorgetti B, Aicardi G, Fattoretti P. Ketogenic diets: an historical antiepileptic therapy with promising potentialities for the aging brain. Ageing Res Rev 2010;9:273–279.
[Article] [PubMed]55. Henderson ST, Vogel JL, Barr LJ, Garvin F, Jones JJ, Costantini LC. Study of the ketogenic agent AC-1202 in mild to moderate Alzheimer's disease: a randomized, double-blind, placebo-controlled, multicenter trial. Nutr Metab (Lond) 2009;6:31
[Article] [PubMed] [PMC]56. Kashiwaya Y, Takeshima T, Mori N, Nakashima K, Clarke K, Veech RL. D-beta-hydroxybutyrate protects neurons in models of Alzheimer's and Parkinson's disease. Proc Natl Acad Sci U S A 2000;97:5440–5444.
[Article] [PubMed] [PMC]

 About
About Browse articles
Browse articles For contributors
For contributors