All issues > Volume 55(11); 2012
Early neurodevelopment in very low birth weight infants with mild intraventricular hemorrhage or those without intraventricular hemorrhage
- Corresponding author: So-Hee Eun, MD. Department of Pediatrics, Korea University Ansan Hospital, Korea University College of Medicine, 123 Jeokgeum-ro, Danwon-gu, Ansan 425-707, Korea. Tel: +82-31-412-5096, Fax: +82-31-405-8591, sheun@korea.ac.kr
- Received July 23, 2012 Revised August 31, 2012 Accepted October 09, 2012
- Abstract
-
- Purpose
- Purpose
- This study aimed to assess early development in very low birth weight (VLBW) infants with mild intraventricular hemorrhage (IVH) or those without IVH and to identify the perinatal morbidities affecting early neurodevelopmental outcome.
- Methods
- Methods
- Bayley Scales of Infant Development-II was used for assessing neurological development in 49 infants with a birth weight <1,500 g and with low grade IVH (≤grade II) or those without IVH at a corrected age of 12 months.
- Results
- Results
- Among the 49 infants, 19 infants (38.8%) showed normal development and 14 (28.6%) showed abnormal mental and psychomotor development. Infants with abnormal mental development (n=14) were mostly male and had a longer hospitalization, a higher prevalence of patent ductus arteriosus (PDA) and bronchopulmonary dysplasia (BPD), and were under more frequent postnatal systemic steroid treatment compared with infants with normal mental development (n=35, P<0.05). Infants with abnormal psychomotor development (n=29) had a longer hospitalization and more associated PDA compared to infants with normal psychomotor development (n=20, P<0.05). Infants with abnormal mental and psychomotor development were mostly male and had a longer hospitalization and a higher prevalence of PDA and BPD compared to infants with normal mental and psychomotor development (n=19, P<0.05). Using multiple logistic regression analysis, a longer duration of hospitalization and male gender were found to be significant risk factors.
- Conclusion
- Conclusion
- Approximately 62% of VLBW infants with low grade IVH or those without IVH had impaired early development.
- Introduction
- Introduction
As survival of very preterm infants improves, the effort to improve major morbidities and quality of life in those infants has become a hot topic in neonatology. Of the major morbidities, neurologic impairment is one of the most important problems and requires early detection and intervention. Early detection of neurologic problems in preterm infants is important because early therapeutic intervention has a positive effect on final neurologic outcome1,2).Germinal matrix-intraventricular hemorrhage (IVH) is the most common variety of neonatal intracranial hemorrhage and is characteristic of the premature infant. It is well known that IVH is closely related to the mortality rate and neurological sequelae in premature infants3).Having no or mild IVH results in better outcomes than having a severe one. However, cranial ultrasonography, which is the screening procedure of choice for IVH, is limited in its ability to predict neurological sequelae.In this study, we evaluated the early developmental status of very low birth weight (VLBW) infants with no or low-grade IVH (≤grade II), which is a major patient population of high-risk preterm infants. And we also tried to identify the perinatal morbidities affecting early neurodevelopmental outcome.
- Materials and methods
- Materials and methods
- 1. Study subjects
- 1. Study subjects
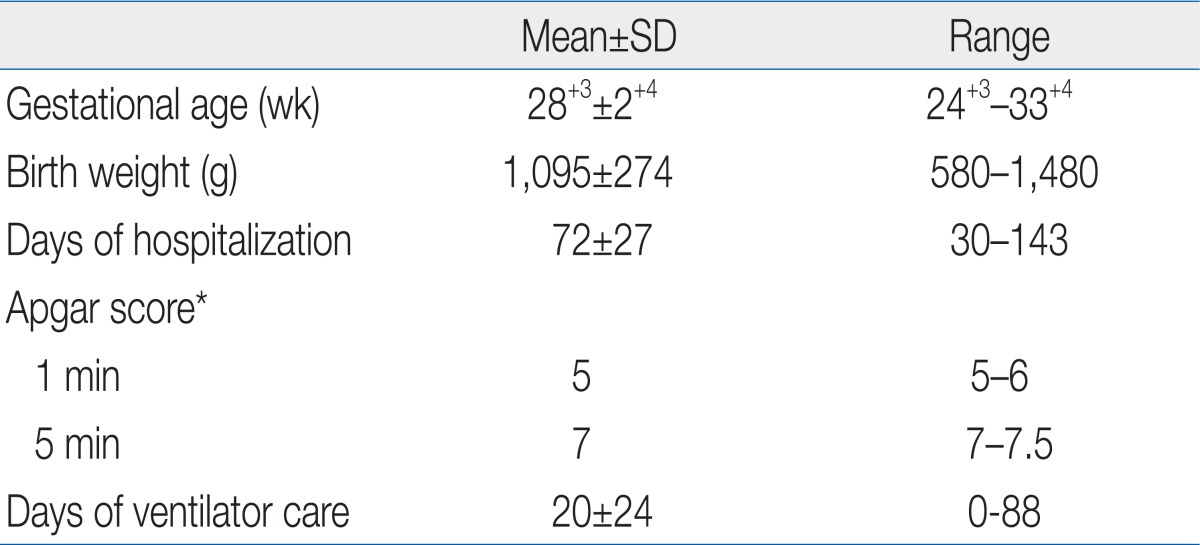
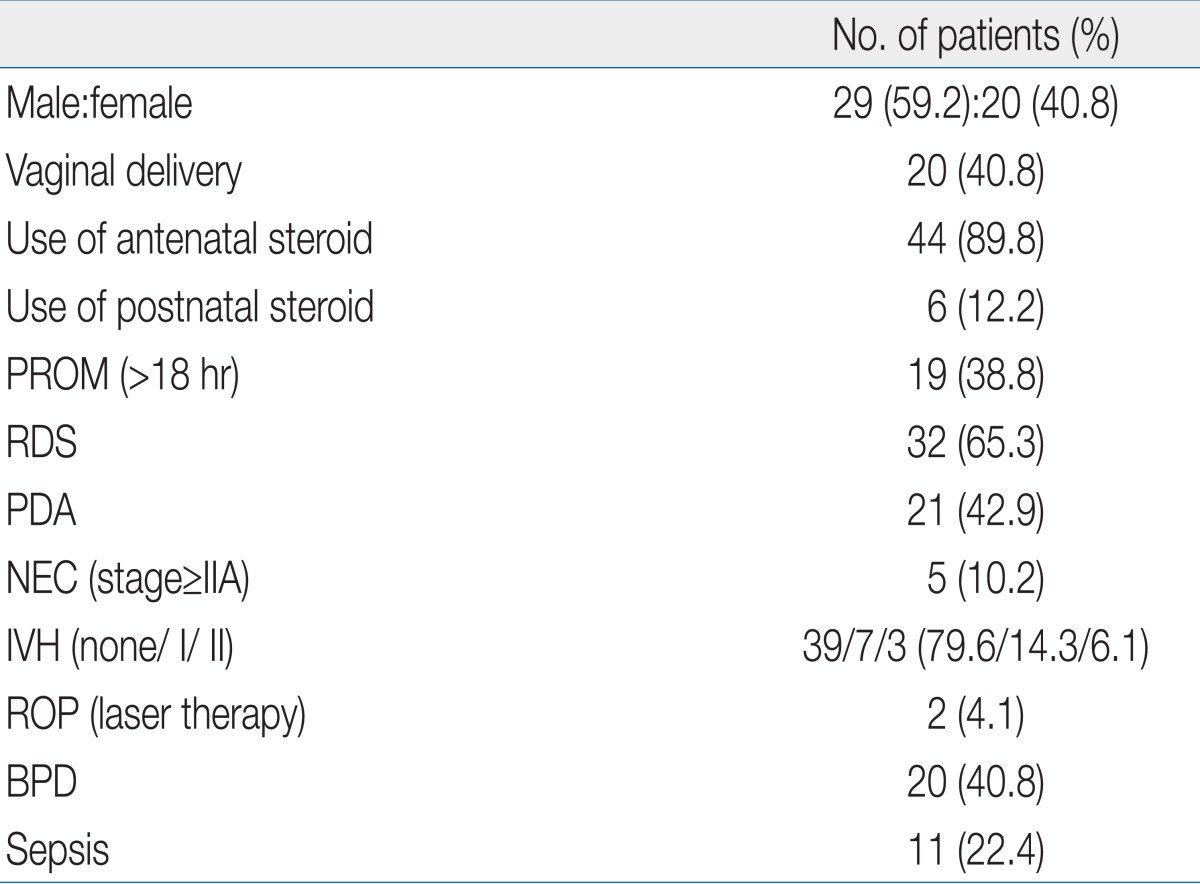
A retrospective review of medical records was performed for all infants who were treated in the neonatal intensive care units (NICU) of Korea University Medical Centers between 2006 and 2009. Fortynine VLBW infants (birth weight<1,500 g) with no or low-grade IVH (≤grade II) were enrolled in this study. Gestational age and birth weight of the 49 infants were 28+3±2+4 weeks and 1,095±274 g, respectively. Demographic data of the subjects are shown in Tables 1 and 2.- 2. Assessment of neurodevelopment
- 2. Assessment of neurodevelopment
When subjects reached a corrected age of 12 months, one psychologist administered the Bayley Scales of Infant Development-II (BSID-II). BSID-II yielded scores for mental and psychomotor development with a standardization mean of 100 and standard deviation of 15 points. The mental developmental index (MDI) and psychomotor developmental index (PDI) were used as scales of cognition and motor development, respectively. Abnormal MDI or PDI were defined as scores of less than 85. Development was considered mildly impaired if scores were 70 to 84, moderately impaired if 55 to 69, and severely impaired if less than 55. Comparisons between the two groups with normal and abnormal developmental scores were performed, and correlations between developmental outcomes and perinatal morbidities were analyzed.- 3. Definitions of perinatal morbidities
- 3. Definitions of perinatal morbidities
The protocol for IVH screening of VLBW infants in the NICU involved radiologists evaluating a cranial ultrasonogram within one week postnatally and every 2 to 4 weeks until the time of discharge from the NICU. The definition of IVH was based on the Papil grading system4).Respiratory distress syndrome was defined by the therapeutic instillation of surfactant, and patent ductus arteriosus (PDA) was defined by therapeutic injection of prostaglandin inhibitor or a ligation operation. Bronchopulmonary dysplasia (BPD) was defined as the need for supplemental oxygen support at a postmenstrual age of 36 weeks5), and necrotizing enterocolitis was defined as Bell's stage II or greater6). Retinopathy of prematurity was defined as the need for therapeutic intervention, and sepsis was defined as a positive blood culture with clinical signs of sepsis.- 4. Statistical analysis
- 4. Statistical analysis
Categorical data are presented as numbers (%), and continuous data as the mean±SD or median (25 to 75%). The χ2 or Fisher's exact test was used to compare categorical variables, and the Student's t test and the Mann-Whitney's rank sum U test were used to compare continuous variables in univariate analysis. IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA) was used for the statistical analysis, and a P value of less than 0.05 was considered statistically significant. Multiple logistic regression was performed with significant factors identified in the univariate analysis.
- Results
- Results
- 1. Neurodevelopmental outcome
- 1. Neurodevelopmental outcome
1) Mental development
1) Mental development
The mean MDI score of all 49 infants was 94±27. Thirty-five infants (71.4%) had normal MDI scores that were between 85 and 115. Fourteen infants (28.6%) had MDI scores of less than 85 and comprised the abnormal MDI group. Three (6.1%) had MDI scores of 70 to 84, suggesting mild impairment, and three (6.1%) had MDI scores of 55 to 69, suggesting moderate impairment. Eight (16.3%) had MDI scores of less than 55, suggesting severe impairment.2) Motor development
2) Motor development
The mean PDI score of all 49 infants was 81±19. Twenty infants (40.8%) had normal PDI scores that were between 85 and 115. Twenty-nine infants (59.2%) had PDI scores of less than 85 and comprised the abnormal PDI group. Fourteen (28.6%) had PDI scores of 70 to 84, suggesting mild impairment, and eight (16.3%) had PDI scores of 55 to 69, suggesting moderate impairment. Seven (14.3 %) had PDI scores of less than 55, suggesting severe impairment.
Nineteen infants (38.8%) had normal scores of above 85 on both the MDI and PDI, and 14 infants (28.6%) had less than 85 on both the MDI and PDI. Distributions of MDI and PDI scores of all infants are shown in Fig. 1.- 2. Perinatal morbidities affecting early neurodevelopmental outcome
- 2. Perinatal morbidities affecting early neurodevelopmental outcome
1) Comparison between groups with normal and abnormal mental development
1) Comparison between groups with normal and abnormal mental development
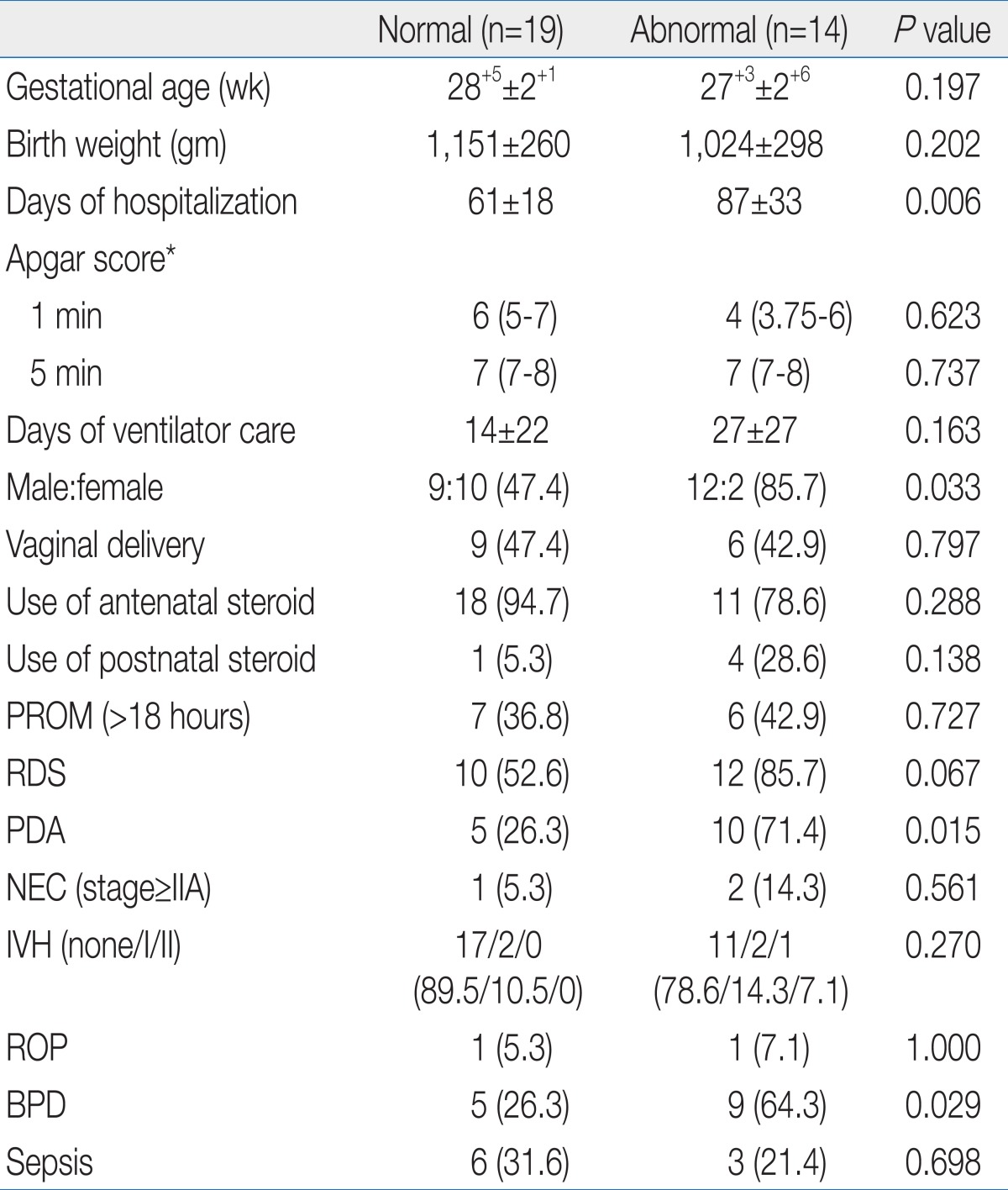
Compared to the normal MDI group (n=35), the abnormal MDI group (n=14) were more often male and had a longer duration of hospitalization, higher prevalence of PDA and BPD, and more postnatal use of systemic steroids (P<0.05) (Table 3). In the multiple logistic regression, male gender was the only statistically significant risk factor (odds ratio [OR], 17.1; 95% confidence interval (CI), 1.83 to 159.4; P=0.013) (Table 4).2) Comparison between groups with normal and abnormal motor development
2) Comparison between groups with normal and abnormal motor development
Compared to the normal PDI group (n=20), the abnormal PDI group (n=29) had a longer duration of hospitalization and higher prevalence of PDA (P<0.05) (Table 5). In the multiple logistic regression, there was no statistically significant factor associated with abnormal PDI among the perinatal morbidities that was significant in the univariate analysis (Table 4).3) Comparison between groups with normal and global impairment
3) Comparison between groups with normal and global impairment
Compared to normal infants (n=19), the infants with global mental and psychomotor impairment (n=14) were more often male and had a longer duration of hospitalization and more PDA and BPD (P<0.05) (Table 6). In the multiple logistic regression, a longer duration of hospitalization was the only statistically significant risk factor (OR, 1.08; 95% CI, 1.004 to 1.156; P=0.038) (Table 4).
- Discussion
- Discussion
The purpose of this study was to objectively assess the early development of VLBW infants with no or mild IVH, which is a major patient population of high-risk preterm infants, and to identify the perinatal morbidities affecting early neurodevelopmental outcome. We observed that 62% of VLBW infants with no or mild IVH had impaired early development, and several perinatal factors, such as longer duration of hospitalization, male gender, the presence of PDA or BPD, and postnatal use of systemic steroids, were related to impaired early development. In particular, longer duration of hospitalization and male gender were the most important prognostic factors in the early development of VLBW infants with no or mild IVH.In a previous report, 10 to 15% of surviving VLBW infants were diagnosed with neurologic problems, such as cerebral palsy and major psychomotor and cognitive deficits7). Although cranial ultrasonography is the screening procedure of choice for IVH, some reports suggest that over 50% of VLBW infants with cerebral palsy do not have intraventricular abnormalities detectable by ultrasonography8). Moreover, neurologic manifestations of cerebral palsy may not be apparent until the child is 2 to 3 years old9).Naturally, it is difficult to predict cognitive and motor functions in growing and developing infants, especially among expreterm infants with a mild degree of impairment. The later the assessment of neurodevelopment is performed, the more the findings approximate the final neurodevelopmental outcome. However, earlier recognition of developmental problems is important because early intervention for preterm infants with neurodevelopmental impairment may improve cognitive and neuromotor development10,11). Therefore, the effort to detect early neurodevelopmental problems can be very important.BSID is the gold standard for assessing motor and cognitive performance of preterm infants in many studies, despite some limitations12,13). There are many studies that have evaluated the neurodevelopment of preterm infants with a variety of objectives at different time points. Hack et al.14) reported that 67% and 39% of extremely low birth weight infants had MDI scores <85 and <70 at a corrected age of 20 months, respectively. Chuang et al.15) reported that VLBW infants with subependymal cysts had a significantly lower psychomotor development index and were more likely than normal term infants to have motor developmental delay at a corrected age of 24 months. In this study, we performed the neurodevelopmental assessment at an earlier age, a corrected age of 12 months, and specifically focused on VLBW infants with no or mild IVH, which is a patient population that includes many high-risk preterm infants.In this study, we used the BSID-II, which is an assessment tool with confirmed validity and objectivity that is recognized by most neonatologists, to evaluate the early neurodevelopment of VLBW infants with no or mild IVH16). Our study revealed that many of the infants had an abnormal neurodevelopmental status necessitating careful follow-up and early therapeutic intervention.Our results also showed that a longer duration of hospitalization, male gender, the presence of PDA or BPD, and postnatal use of systemic steroids might be associated with abnormal neurodevelopmental outcomes. It has been reported that BPD, PDA, and postnatal use of systemic steroids are associated with adverse mental and psychomotor development17-20).Male gender is also known to be an independent risk factor for adverse mental and psychomotor development21,22).In conclusion, over half of the VLBW infants with no or low grade IVH in our study had impaired early development at corrected age 12 months. Several perinatal factors, such as longer duration of hospitalization, male gender, the presence of PDA or BPD, and postnatal use of systemic steroids, were potential risk factors for impaired development. In particular, prolonged hospitalization and male gender were closely related factors. Therefore, male preterm infants who have prolonged hospitalizations require careful neurodevelopmental examination, even if the infants do not have a history of severe IVH.
- References
- 1. Spittle AJ, Orton J, Doyle LW, Boyd R. Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database Syst Rev 2007;(2): CD005495
[Article] [PubMed]2. Ohgi S, Fukuda M, Akiyama T, Gima H. Effect of an early intervention programme on low birthweight infants with cerebral injuries. J Paediatr Child Health 2004;40:689–695.
[Article] [PubMed]3. Volpe JJ. The neurology of the newborn. 2001;4th ed. Philadelphia: W.B. Saunders, :428–493.4. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978;92:529–534.
[Article] [PubMed]5. Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988;82:527–532.
[Article] [PubMed]6. Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 1986;33:179–201.
[Article] [PubMed] [PMC]7. Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR. EPICure Study Group. Neurologic and developmental disability after extremely preterm birth. N Engl J Med 2000;343:378–384.
[Article] [PubMed]8. Pinto-Martin JA, Riolo S, Cnaan A, Holzman C, Susser MW, Paneth N. Cranial ultrasound prediction of disabling and nondisabling cerebral palsy at age two in a low birth weight population. Pediatrics 1995;95:249–254.
[Article] [PubMed]9. Mirmiran M, Barnes PD, Keller K, Constantinou JC, Fleisher BE, Hintz SR, et al. Neonatal brain magnetic resonance imaging before discharge is better than serial cranial ultrasound in predicting cerebral palsy in very low birth weight preterm infants. Pediatrics 2004;114:992–998.
[Article] [PubMed]10. Koldewijn K, Wolf MJ, van Wassenaer A, Meijssen D, van Sonderen L, van Baar A, et al. The Infant Behavioral Assessment and Intervention Program for very low birth weight infants at 6 months corrected age. J Pediatr 2009;154:33–38.e2.
[Article] [PubMed]11. Als H, Lawhon G, Duffy FH, McAnulty GB, Gibes-Grossman R, Blickman JG. Individualized developmental care for the very low-birth-weight preterm infant. Medical and neurofunctional effects. JAMA 1994;272:853–858.
[Article] [PubMed]12. Vohr BR, Msall ME, Wilson D, Wright LL, McDonald S, Poole WK. Spectrum of gross motor function in extremely low birth weight children with cerebral palsy at 18 months of age. Pediatrics 2005;116:123–129.
[Article] [PubMed]13. Vincer MJ, Cake H, Graven M, Dodds L, McHugh S, Fraboni T. A population-based study to determine the performance of the Cognitive Adaptive Test/Clinical Linguistic and Auditory Milestone Scale to Predict the Mental Developmental Index at 18 Months on the Bayley Scales of Infant Development-II in very preterm infants. Pediatrics 2005;116:e864–e867.
[Article] [PubMed]14. Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Wilson-Costello D, et al. Poor predictive validity of the Bayley Scales of Infant Development for cognitive function of extremely low birth weight children at school age. Pediatrics 2005;116:333–341.
[Article] [PubMed]15. Chuang YC, Lee C, Chiu NC, Shu CH, Hung HY, Kao HA, et al. Neurodevelopment in very low birth weight premature infants with postnatal subependymal cysts. J Child Neurol 2007;22:402–405.
[Article] [PubMed]16. Bayley N. Manual for the Bayley Scales of Infant Development. 1993;2nd ed. San Antonio: Psychological Co..17. Majnemer A, Riley P, Shevell M, Birnbaum R, Greenstone H, Coates AL. Severe bronchopulmonary dysplasia increases risk for later neurological and motor sequelae in preterm survivors. Dev Med Child Neurol 2000;42:53–60.
[Article] [PubMed]18. Short EJ, Klein NK, Lewis BA, Fulton S, Eisengart S, Kercsmar C, et al. Cognitive and academic consequences of bronchopulmonary dysplasia and very low birth weight: 8-year-old outcomes. Pediatrics 2003;112:e359
[Article] [PubMed]19. Cooke RW. Perinatal and postnatal factors in very preterm infants and subsequent cognitive and motor abilities. Arch Dis Child Fetal Neonatal Ed 2005;90:F60–F63.
[Article] [PubMed] [PMC]20. Halliday HL, Ehrenkranz RA, Doyle LW. Moderately early (7-14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 2003;(1): CD001144
[PubMed]21. Platt MJ, Cans C, Johnson A, Surman G, Topp M, Torrioli MG, et al. Trends in cerebral palsy among infants of very low birthweight (<1500 g) or born prematurely (<32 weeks) in 16 European centres: a database study. Lancet 2007;369:43–50.
[Article] [PubMed]22. Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR, et al. The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed 2005;90:F134–F140.
[Article] [PubMed] [PMC]
Fig. 1
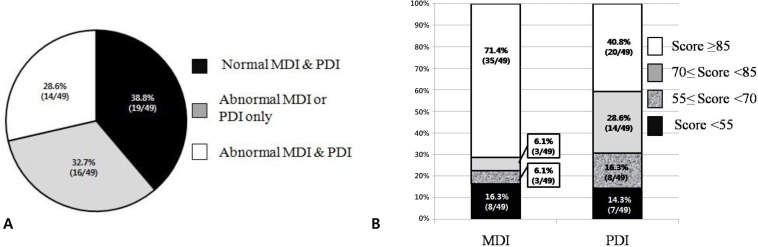
Table 3

Values are presented as mean±SD, mean (range) or number (%).
MDI, mental developmental index; PROM, premature rupture of membrane; RDS, respiratory distress syndrome; PDA, patent ductus arteriosus; NEC, necrotizing enterocolitis; IVH, intraventricular hemorrhage; ROP, retinopathy of prematurity; BPD, bronchopulmonary dysplasia.
*Apgar score is expressed with median (25-75%).
Table 4
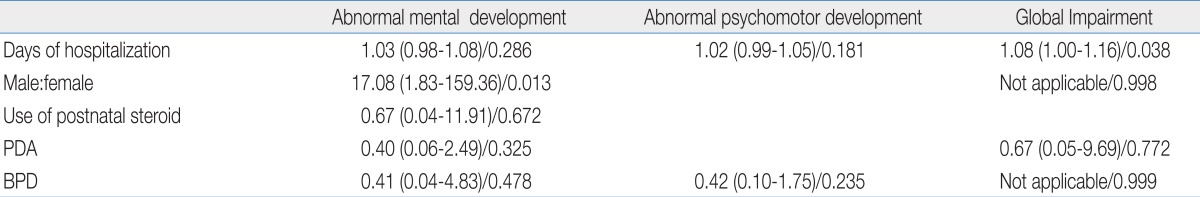
Table 5
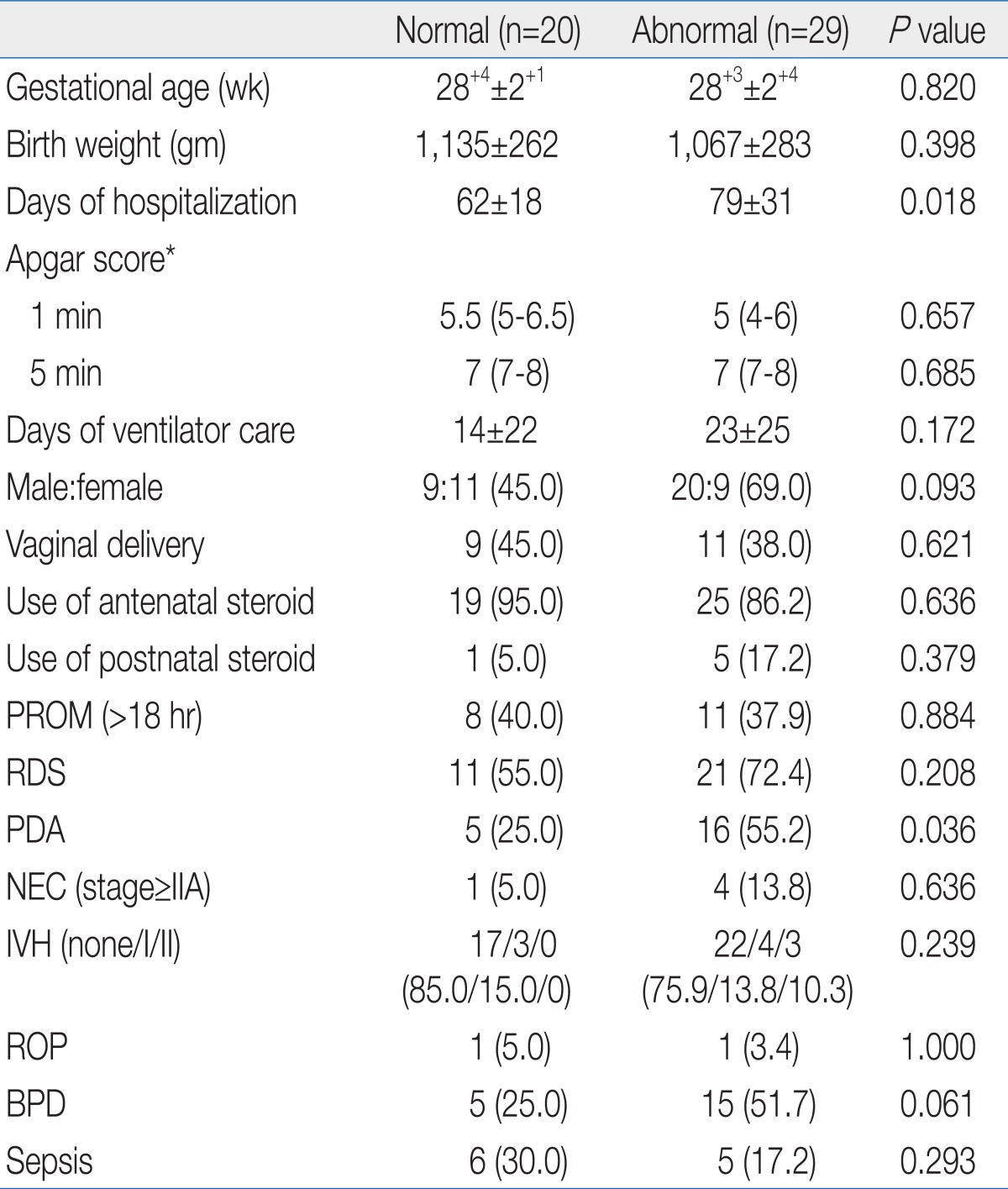
Values are presented as mean±SD, mean (range) or number (%).
PDI, psychomotor developmental index; PROM, premature rupture of membrane; RDS, respiratory distress syndrome; PDA, patent ductus arteriosus; NEC, necrotizing enterocolitis; IVH, intraventricular hemorrhage; ROP, retinopathy of prematurity; BPD, bronchopulmonary dysplasia.
*Apgar score is expressed with median (25-75%).

 About
About Browse articles
Browse articles For contributors
For contributors