All issues > Volume 55(12); 2012
Effect of early postnatal neutropenia in very low birth weight infants born to mothers with pregnancy-induced hypertension
- Corresponding author: Jae Woo Lim, MD. Department of Pediatrics, Konyang University College of Medicine, 158 Gwanjeodong-ro, Seo-gu, Daejeon 302-718, Korea. Tel: +82-42-600-9230, Fax: +82-42-600-9090, jwlim@kyuh.ac.kr
- Received August 24, 2012 Revised September 22, 2012 Accepted October 13, 2012
- Abstract
-
- Purpose
- Purpose
- In this study, we aimed to investigate the perinatal clinical conditions of very low birth weight (VLBW) infants born to mothers with pregnancy-induced hypertension (PIH) focusing on the effects of early postnatal neutropenia.
- Methods
- Methods
- We reviewed the medical records of 191 VLBW infants who were born at Konyang University Hospital, between March 2003 and May 2011. We retrospectively analyzed the clinical characteristics of the infants and their mothers and compared the incidence of perinatal diseases and mortality of the infants according to the presence or absence of maternal PIH and neutropenia on the first postnatal day.
- Results
- Results
- Infants born to mothers with PIH showed an increased incidence of neutropenia on the first postnatal day (47.4%), cesarean delivery, and intrauterine growth restriction. When the infants born to mothers with PIH showed neutropenia on the first postnatal day, their incidence of respiratory distress syndrome (RDS) was increased (P=0.031); however, the difference was not found to be significant through logistic regression analysis. In all the VLBW infants, neutropenia on the first postnatal day was correlated with the development of RDS. The incidence of the other perinatal diseases involving sepsis and mortality did not significantly differ according to the presence or absence of neutropenia in infants born to mothers with PIH.
- Conclusion
- Conclusion
- In VLBW infants born to mothers with PIH, the incidence of neutropenia on the first postnatal day was increased and it was not significantly correlated with the development of perinatal diseases involving RDS, sepsis, and mortality.
- Introduction
- Introduction
Pregnancy-induced hypertension (PIH) occurs in approximately 6 to 20% of pregnant women1). In hypertensive pregnancies, the risk of cesarean delivery, abruption of placenta, preterm delivery, and intrauterine growth restriction (IUGR) are increased, and the perinatal outcome of mothers and infants can become worse2-4). Infants born to mothers with PIH have a higher incidence of neutropenia and thrombocytopenia in the early postnatal days5,6). Although the exact underlying mechanisms are unclear, it is thought to be associated with decreased hematogenesis in the bone marrow or immunological destruction5,7).Neonatal neutropenia can be associated with infection and sepsis8,9) and can increase morbidity and mortality, especially in very low birth weight infants (VLBW)10,11). In addition, animal studies conducted by Carlton et al.12) and other studies13-15) have suggested that neutropenia during the early postnatal period is associated with an increased risk of respiratory distress and bronchopulmonary dysplasia (BPD). Infants born to mothers with PIH are often born with VLBW, and early postnatal neutropenia might be considered to negatively affect their clinical condition.In this study, we reviewed the clinical findings of VLBW infants born to mothers with PIH and investigated the effect of early postnatal neutropenia on the perinatal clinical conditions of these infants.
- Materials and methods
- Materials and methods
- 1. Subjects
- 1. Subjects
We reviewed the medical records of 197 infants with gestational ages between 24 and 32 weeks and birth weights of <1,500 g who were admitted to the neonatal intensive care unit (NICU) of the Konyang University Hospital from March 2003 to May 2011. We excluded 6 infants who had a congenital anomaly. Thus, a total of 191 infants were enrolled in the present study.- 2. Methods
- 2. Methods
We collected the following data for the mothers: maternal age, number of live births, history of antenatal care (PIH, allergy, infection, premature rupture of membrane [PROM], chorioamnionitis, incompetent cervix, or fetal distress), and drug history (especially the use of steroids and/or magnesium).We collected the following data for the infants: gestational age, birth weight, Apgar scores, sex, twin status, presence of IUGR, presence of perinatal disease (respiratory distress syndrome [RDS], BPD, sepsis, necrotizing enterocolitis [NEC], intraventricular hemorrhage [IVH], periventricular leukomalacia [PVL], or retinopathy of prematurity [ROP]), hospital days, mortality, and results of complete blood cell count (CBC) performed on the first postnatal day. Data were collected retrospectively from medical records.In this NICU, CBC is routinely performed immediately after birth and concurrently with admission. Thus, in this study, CBC on the first postnatal day was performed within 4 hours after birth in all the subjects. Maternal PIH was diagnosed when blood pressure higher than 140/90 mmHg occurred after 20 weeks of postmenstrual age16). We defined neutropenia on the first postnatal day as a peripheral absolute neutrophil count (ANC) lower than 1,500/µL according to Manroe et al.17) and thrombocytopenia as a peripheral platelet count lower than 150,000/µL18). RDS was diagnosed when infants showed clinical signs of respiratory difficulty, and when chest radiographs revealed specific manifestations of RDS such as reticulonodular pattern or air-bronchogram, and when infants required an oxygen supply higher than FiO2 0.419). According to the new diagnostic criteria of Jobe and Bancalari20), BPD was diagnosed when oxygen therapy (supplemental oxygen higher than 21%) was required for at least 28 days at 36 weeks postmenstrual age or upon discharge in infants younger than 32 weeks gestational age and between 28 and 56 days or upon discharge in infants older than 32 weeks gestational age. Sepsis was diagnosed when bacterial pathogens were detected in 1 or more blood cultures along with the appropriate clinical signs such as decreased activity, decreased feeding, fever, apnea, tachypnea, or C-reactive protein elevation21). Sepsis occurring within 7 days after birth was defined as early-onset sepsis, and that occurring later than 7 days after birth was defined as late-onset sepsis.We compared the clinical findings of the VLBW infants who were divided into 2 groups according to the presence or absence of maternal PIH. Infants born to mothers with PIH were further classified into 2 groups according to the presence or absence of infantile neutropenia on the first postnatal day, and the differences in perinatal clinical conditions between the 2 groups were investigated.- 3. Statistical analyses
- 3. Statistical analyses
Statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Comparisons between groups were performed using the paired t test, chi-square test, and Fisher's exact test, and the data were expressed as mean±standard deviation (SD) for continuous variables. Logistic regression analyses were performed to determine the factors affecting the development of neutropenia on the first postnatal day and to assess the risk of perinatal diseases affected by neutropenia considering the variables that are supposed to affect infantile neutropenia and common perinatal diseases in VLBW infants. Statistical significance was set at P<0.05.
- Results
- Results
- 1. Clinical characteristics of the subjects
- 1. Clinical characteristics of the subjects
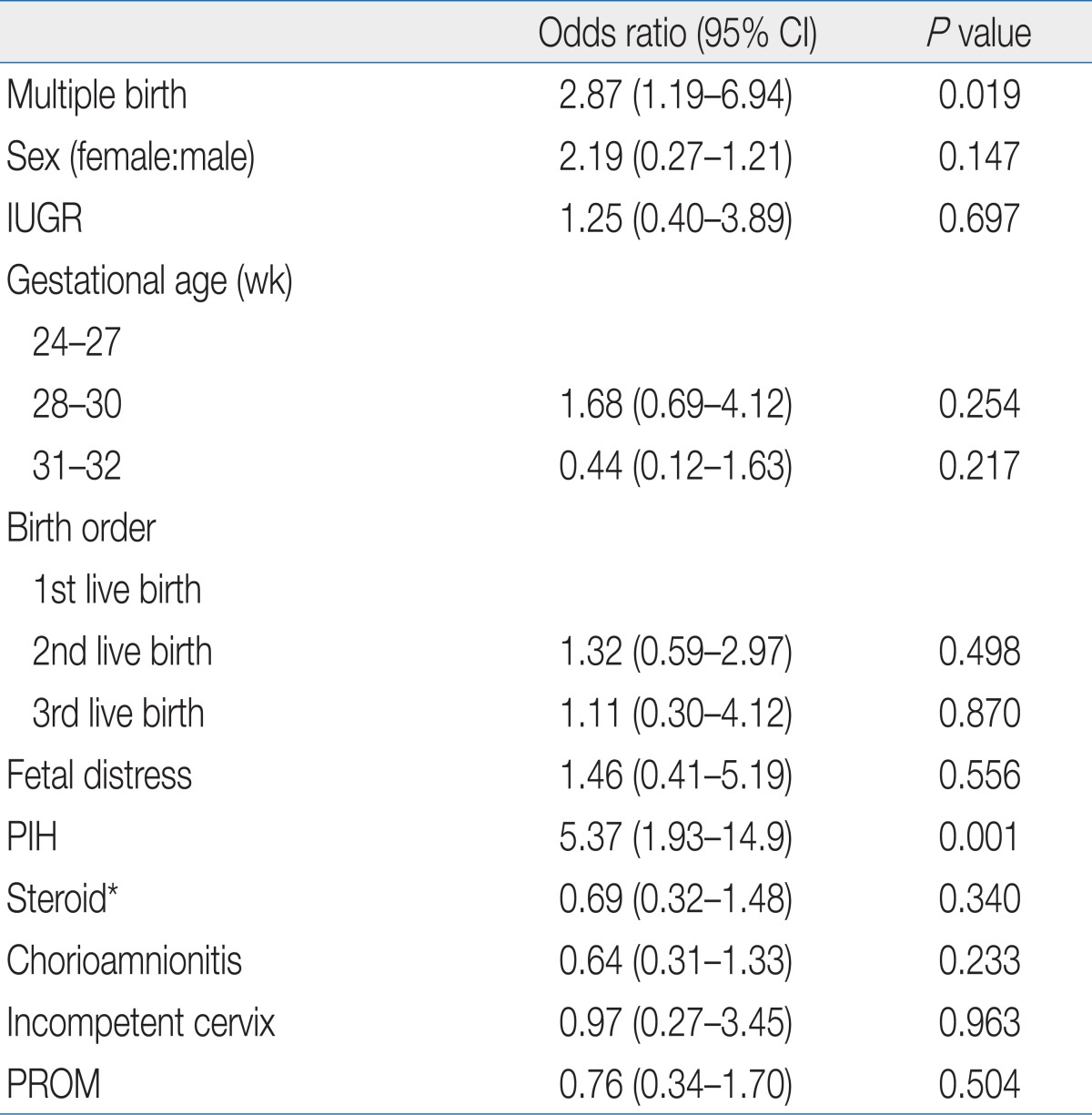
A total of 191 VLBW infants were enrolled in the study, of which 97 (50.8%) were male and 94 (49.2%) were female. The mean birth weight (mean±SD) was 1,136.7±231 g; the mean gestational age was 28.9±2.1 weeks, and the mean hospital stays was 62.3±26.8 days. There were 38 cases (19.9%) of maternal PIH and 51 cases (26.7%) of infantile neutropenia on the first postnatal day. For the perinatal diseases, there were 152 cases (79.6%) of RDS, 69 cases (37.1%) of BPD, 31 cases (16.2%) of sepsis, and 18 cases (9.6%) of NEC. Mortality was observed in 35 cases (18.3%).To review the clinical findings of the VLBW infants born to mothers with PIH, we divided the infants into 2 groups, the infants born to mothers with PIH (group A) and the infants born to mothers without PIH (group B, Table 1). No statistically significant differences in the mean birth weight and 1 min/5 min Apgar scores (P>0.05) were detected, but the mean gestational age was higher in group A (30.2±2.1 weeks) than in group B (28.5±2.0 weeks, P<0.001). The incidence rates of cesarean delivery and IUGR were higher in group A (97.4% [37 cases] and 42.1% [16 cases], respectively) than in group B (74.5% [114 cases] and 5.9% [9 cases], respectively) (P=0.002 and P<0.001, respectively). The CBC results on the first postnatal day showed that the mean ANC and platelet count were lower in group A than in group B (P=0.008 and P<0.001, respectively), and the mean hemoglobin value was higher in group A than in group B (P=0.001).In the comparison of the incidence of perinatal diseases and mortality, the incidence of neutropenia on the first postnatal day was significantly higher in group A (47.4%, 18 cases) than in group B (21.6%, 33 cases) (P=0.001) (Table 2). The incidence of thrombocytopenia on the first postnatal day was higher in group A (15.8%, 6 cases) than in group B (9.8%, 15 cases), but the difference was not statistically significant (P=0.291). The incidence of RDS was lower in group A (65.8%, 25 cases) than in group B (83.0%, 127 cases; P=0.018). There were no significant differences in the incidences of the other perinatal diseases (BPD, sepsis, NEC, IVH, PVL, and ROP), hospital days, and mortality between the 2 groups (P>0.05) (Table 2).- 2. Clinical characteristics of the infants with neutropenia on the first postnatal day who were born to mothers with PIH
- 2. Clinical characteristics of the infants with neutropenia on the first postnatal day who were born to mothers with PIH
To investigate the effects of neutropenia on the first postnatal day on the perinatal clinical conditions of the infants born to mothers with PIH, we divided the VLBW infants born to mothers with PIH into 2 groups according to the presence (group A-I) or absence (group A-II) of neutropenia on the first postnatal day and compared the clinical characteristics of the 2 groups.There were no statistically significant differences in the mean birth weight, mean gestational age, and 1 min/5 min Apgar scores between the 2 group (P>0.05) (Table 3). The CBC results obtained on the first postnatal day indicated no significant differences in the mean hemoglobin value and mean platelet count between the 2 groups (P=0.409 and P=0.771, respectively). Comparison of the incidence of perinatal diseases and mortality (Table 4) between both groups showed that the incidence of RDS was significantly higher in group A-I (83.3%, 15 cases) than in group A-II (50.0%, 10 cases; P=0.031). The incidence of BPD and sepsis was higher in group A-I (38.9% and 22.2%, respectively) than in group A-II (22.2% and 5%), but these differences did not reach statistical significance (P=0.471 and P=0.170, respectively). The other perinatal diseases (NEC, IVH, PVL, and ROP) and hospital days were not significantly different between the 2 groups (P>0.05) (Table 4). Mortality was higher in group A-I (27.8%, 5 cases) than in group A-II (10.0%, 2 cases), but the difference was not statistically significant (P=0.222).- 3. Factors affecting the development of neutropenia on the first postnatal day in the VLBW infants
- 3. Factors affecting the development of neutropenia on the first postnatal day in the VLBW infants
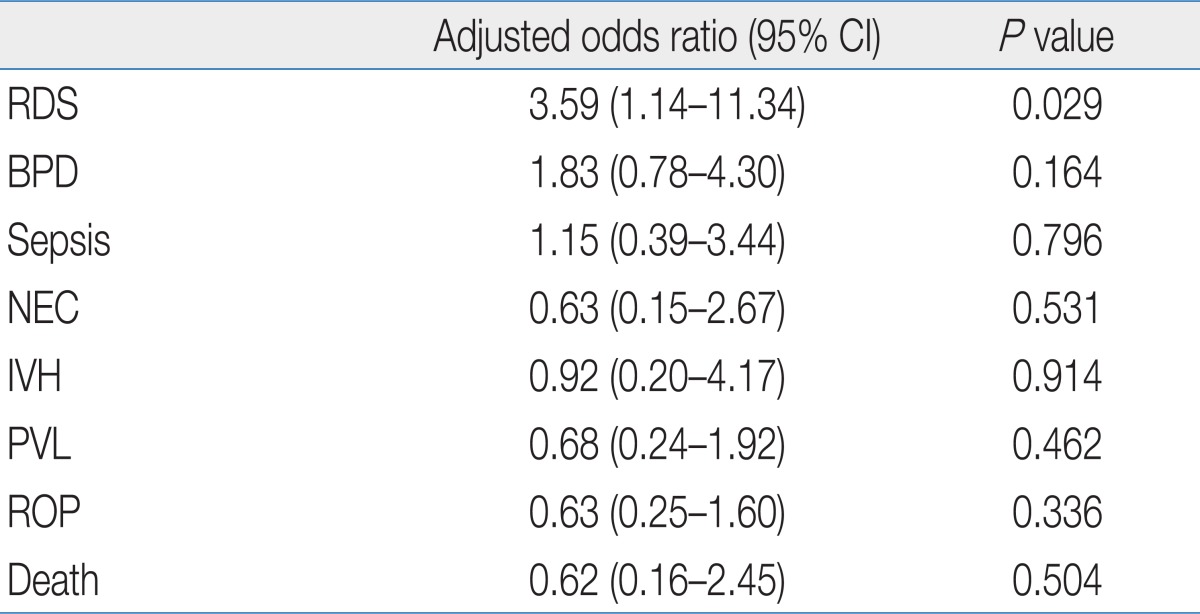
To better understanding the difference in perinatal clinical conditions according to the presence or absence of early postnatal neutropenia, we examined the factors affecting the development of early postnatal neutropenia. Logistic regression analysis was performed to assess the factors independently affecting the development of neutropenia on the first postnatal day in all the VLBW infants considering the variables that showed a correlation on the univariate analysis or those expected to affect infantile neutropenia.Multiple birth (odds ratio [OR], 2.87; 95% confidence interval [CI], 1.19 to 6.94; P=0.019) and maternal PIH (OR, 5.37; 95% CI, 1.93 to 14.9; P=0.001) showed a correlation with neutropenia on the first postnatal day (Table 5), whereas other variables involving gestational age and IUGR did not show a correlation.- 4. Perinatal diseases affected by neutropenia on the first postnatal day in the VLBW infants
- 4. Perinatal diseases affected by neutropenia on the first postnatal day in the VLBW infants
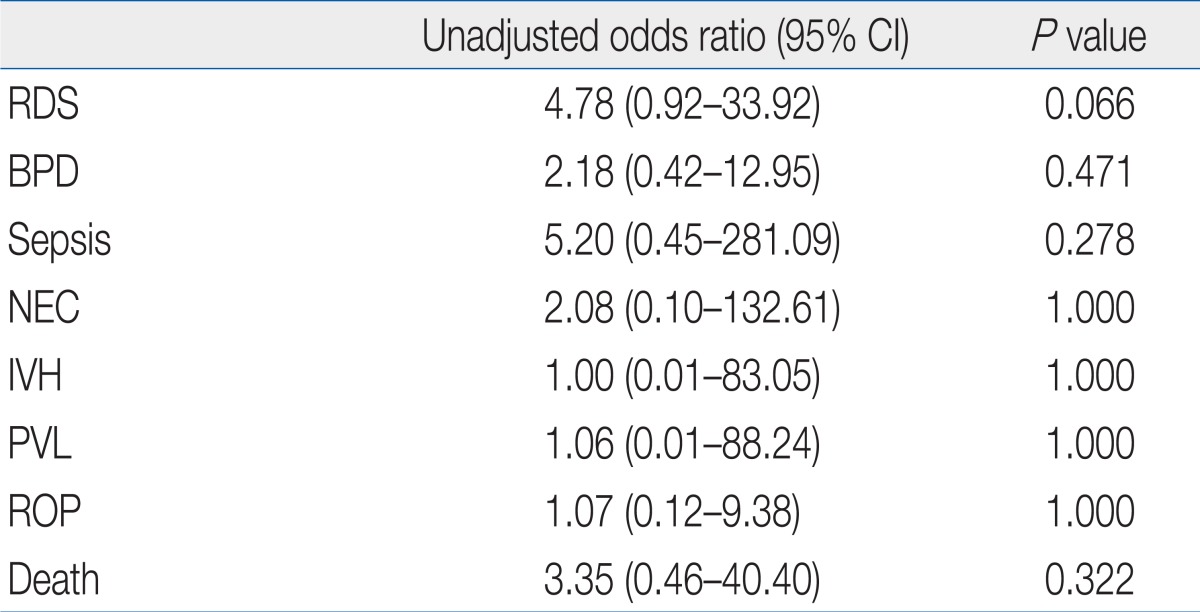
A logistic regression analysis was performed to investigate the effects of neutropenia on the first postnatal day on the perinatal clinical conditions in all the VLBW infants (Table 6). Various perinatal diseases commonly found in the NICU were selected as variables because infantile neutropenia can affect general perinatal clinical conditions in diverse and complicated manners in VLBW infants. RDS showed a correlation with neutropenia on the first postnatal day (OR, 3.59; 95% CI, 1.14 to 11.34; P=0.029), but the other perinatal diseases involving BPD and sepsis showed no significant correlation with neutropenia.- 5. Perinatal diseases affected by neutropenia on the first postnatal day in VLBW infants born to mothers with PIH
- 5. Perinatal diseases affected by neutropenia on the first postnatal day in VLBW infants born to mothers with PIH
To investigate the effects of neutropenia on the first postnatal day on the perinatal clinical conditions in 38 VLBW infants born to mothers with PIH, we performed an unadjusted univariate logistic regression analysis because of the small number of subjects (Table 7). Although the only factor that showed a correlation with neutropenia associated with maternal PIH was RDS in the Fisher's exact test (Table 4), to investigate the effects of neutropenia on the first postnatal day considering general perinatal clinical aspects, various perinatal diseases commonly observed in the NICU were selected as variables. Perinatal diseases involving RDS, which showed a correlation in the analysis performed including all the VLBW infants (Table 6), showed no significant correlation with neutropenia on the first postnatal day in the infants born to PIH mothers.
- Discussion
- Discussion
Neutropenia is a frequent problem in the NICU, and its incidence is reported to be as high as 8% among NICU patients4). Infants born to mothers with PIH have a higher incidence of neutropenia and thrombocytopenia in the early postnatal days than other infants5,6). Neutropenia occurs in approximately 50% of infants born to mothers with PIH and 80% of VLBW infants born to mothers with PIH5,6,9).The exact mechanisms underlying the occurrence of neutropenia in infants born to mothers with PIH remain elusive, but that are thought to be different from those observed in infants born to mothers without PIH. In most cases, infantile neutropenia is idiopathic. Other possible mechanisms are that infantile neutropenia is the result of decreased neutrophil production5,8), increased consumption or destruction of neutrophils associated with microbial infections and alloimmune and autoimmune neutropenia22), and increased migration of neutrophils in the microvascular endothelium8). On the other hand, a number of mechanisms have been suggested as the underlying causes of the development of neutropenia in infants born to PIH mothers, including impaired myelopoiesis, diminished numbers of myeloid progenitors5,23), enhanced expression of Fas-associated proteins7), or diminished endogenous levels of factors that stimulate neutrophil production, such as granulocyte colony-stimulating factor (G-CSF)24).There is a high proportion of VLBW infants among the infants born to mothers with PIH because of the increased risk of IUGR and preterm delivery, and perinatal diseases could be a common problem in these infants2-4). Although previous studies reported the effects of early postnatal neutropenia associated with maternal PIH on perinatal clinical conditions, most of these were studies with limited range, such as those including only hematologic profiles or development of sepsis25-28). Studies that encompass the effect of early postnatal neutropenia on the overall perinatal clinical condition of infants born to mothers with PIH are lacking.This study was initially designed based on the fact that although a correlation between early postnatal neutropenia and respiratory distress and pulmonary complications was reported in previous studies12,29), the incidence of early postnatal neutropenia was increased while the incidence of RDS was decreased in infants born to mothers with PIH5,30). This led us to question how the incidence of RDS changed according to the presence or absence of early postnatal neutropenia in infants born to mothers with PIH. In addition, we examined the differences in overall perinatal clinical conditions involving the incidence of perinatal diseases and mortality according to the presence or absence of early postnatal neutropenia in infants born to mothers with PIH. We restricted the range of subjects to VLBW infants because perinatal diseases mainly occur in preterm infants with low birth weight, and we also restricted the gestational ages of infants to a range between 24 and 32 weeks to reduce the effect of the difference of gestational age because the incidence of IUGR is increased in infants born to mothers with PIH2-4).Among the 191 VLBW infants, 19.9% (38 cases) were born to mothers with PIH. Neutropenia on the first postnatal day was observed in 26.7% (51 cases) of VLBW infants, and 47% (18 cases) of infants born to mothers with PIH. The incidence of infantile neutropenia has been reported to increase with lower gestational age and more severe maternal PIH5,25). In this study, gestational age was not correlated with the development of neutropenia on the first postnatal day, whereas multiple births and maternal PIH showed a significant correlation (Table 7). Possible explanations for this result are that the cases of neutrophilia were not excluded from the analysis, and the range of fluctuation of ANC is wide during the first few days after birth, especially in infants with lower gestational age31). A correlation between the severity of maternal PIH and the development of neutropenia could not be established because of the small number of subjects.The group of infants born to mothers with PIH showed a higher mean gestational age. The mean birth weight and 1 min/5 min Apgar scores of these infants were not significantly different as compared to those of the other infants. The incidences of cesarean delivery, IUGR, and neutropenia on the first postnatal day were increased.The incidence of RDS is known to decrease in infants born to mothers with PIH. This is due to the acceleration of fetal lung maturation by increased stress hormone levels30,32). In this study, the incidence of RDS was decreased in the infants born to PIH mothers. However, their higher gestational age might be considered when interpreting this result. Furthermore, the result was not statistically significant in the additional logistic regression analysis (OR, 0.75; 95% CI, 0.15 to 3.71; P=0.723). There were no significant differences in the incidence of the other perinatal diseases involving BPD and sepsis, hospital days, and mortality.In the comparison of the perinatal clinical conditions of the infants born to mothers with PIH according to the presence or absence of neutropenia on the first postnatal day, the group of infants with neutropenia showed no significant differences in mean birth weight, mean gestational age, and 1 min/5 min Apgar scores, whereas the incidence of RDS was increased significantly (P=0.031). However, in the logistic regression analysis performed for the group of infants born to mothers with PIH, there was no significant correlation between neutropenia on the first postnatal day and the development of perinatal diseases involving RDS (Table 7). On the other hand, in the logistic regression analysis performed for all the VLBW infants, neutropenia on the first postnatal day was significantly correlated with the development of RDS (Table 6).Previous studies reported a correlation between early postnatal neutropenia and the development of respiratory distress. In their in vivo studies, Carlton et al.12) demonstrated that neutropenia detected immediately after birth is associated with the migration of neutrophils from peripheral blood to the lung tissue and sequestration of neutrophils in the lung tissue33). They suggested that this sequestration could lead to inflammation of the pulmonary microvessels and pulmonary parenchyma, and cause pulmonary edema and respiratory distress. Other studies have also reported that early postnatal neutropenia in preterm infants is associated with pulmonary parenchymal damage and development of BPD13,29).These previous studies and the results of the present study showing that the incidence of RDS was significantly increased in infants with neutropenia on the first postnatal day who were born to mothers with PIH on the Fisher's exact test (Table 4) suggest the possibility that deterioration of lung conditions might also occur in infants born to mothers with PIH when they have neutropenia in the early postnatal days. But the logistic regression analysis showed that neutropenia on the first postnatal day and RDS were not significantly correlated in infants born to mothers with PIH. However, this result had a limitation that the number of infants born to mothers with PIH was small (38 cases). Therefore, we could not conduct a multivariate logistic regression and had to conduct a unadjusted univariate logistic regression analysis. Further clinical studies with a large number of subjects and a basic medical study to determine the underlying mechanisms are required.Previous studies investigating the correlation between neutropenia in infants born to mothers with PIH and the development of sepsis have reported variable results. Sharma et al.34) and Doron et al.25) have reported that neutropenia in infants born to mothers with PIH was significantly correlated with the development of sepsis, especially late-onset sepsis. On the contrary, Paul et al.27) and Yoon et al.28) reported no significant correlation between the two. In the present study, among the 38 infants born to mothers with PIH, 18 had neutropenia on the first postnatal day, of whom 4 (22.2%) developed sepsis, and they all represented late-onset sepsis. Compared with 1 (5%) of the infants without neutropenia, the incidence of sepsis was increased when the neutropenia occurred on the first postnatal day in the infants born to mothers with PIH, but the increase was not statistically significant.In the incidence of the other perinatal diseases (NEC, IVH, PVL, and ROP), hospital days, and mortality, no significant differences were found according to the presence or absence of neutropenia on the first postnatal day in the infants born to mothers with PIH.This study has some limitations. The small sample size included 191 VLBW infants and 38 infants born to mothers with PIH. We were unable to evaluate the effects according to the severity of maternal PIH and neutropenia. In addition, the retrospective study design was another limitation.In conclusion, in the VLBW infants born to mothers with PIH, the risks of cesarean delivery, IUGR, and early postnatal neutropenia were increased. In cases of early postnatal neutropenia occurred in the infants born to mothers with PIH, there were no significant differences in hospital days and mortality, and no significant correlation was found between early postnatal neutropenia and perinatal diseases involving RDS and sepsis. Further clinical studies with a large number of subjects are required.
- References
- 1. Dekker GA, Sibai BM. Etiology and pathogenesis of preeclampsia: current concepts. Am J Obstet Gynecol 1998;179:1359–1375.
[Article] [PubMed]2. Roberts CL, Algert CS, Morris JM, Ford JB, Henderson-Smart DJ. Hypertensive disorders in pregnancy: a population-based study. Med J Aust 2005;182:332–335.
[Article] [PubMed]3. Shah DM. Perinatal implications of maternal hypertension. Semin Pediatr Neurol 2001;8:108–119.
[Article] [PubMed]4. Gasem T, Al Jama FE, Burshaid S, Rahman J, Al Suleiman SA, Rahman MS. Maternal and fetal outcome of pregnancy complicated by HELLP syndrome. J Matern Fetal Neonatal Med 2009;22:1140–1143.
[Article] [PubMed]5. Koenig JM, Christensen RD. Incidence, neutrophil kinetics, and natural history of neonatal neutropenia associated with maternal hypertension. N Engl J Med 1989;321:557–562.
[Article] [PubMed]6. Fraser SH, Tudehope DI. Neonatal neutropenia and thrombocytopenia following maternal hypertension. J Paediatr Child Health 1996;32:31–34.
[Article] [PubMed]7. Kuntz TB, Christensen RD, Stegner J, Duff P, Koenig JM. Fas and Fas ligand expression in maternal blood and in umbilical cord blood in preeclampsia. Pediatr Res 2001;50:743–749.
[Article] [PubMed]8. Christensen RD. Neutrophil kinetics in the fetus and neonate. Am J Pediatr Hematol Oncol 1989;11:215–223.
[PubMed]9. Koenig JM, Yoder MC. Neonatal neutrophils: the good, the bad, and the ugly. Clin Perinatol 2004;31:39–51.
[Article] [PubMed]10. Funke A, Berner R, Traichel B, Schmeisser D, Leititis JU, Niemeyer CM. Frequency, natural course, and outcome of neonatal neutropenia. Pediatrics 2000;106(1 Pt 1): 45–51.
[Article] [PubMed]11. Baley JE, Stork EK, Warkentin PI, Shurin SB. Neonatal neutropenia. Clinical manifestations, cause, and outcome. Am J Dis Child 1988;142:1161–1166.
[Article] [PubMed]12. Carlton DP, Cho SC, Albertine KH, Davis PL, Miciak JR, Bland RD. Neutrophil depletion inhibits lung vascular injury and edema in preterm lambs. Pediatr Res 1994;35:1000032713. Kim HS, Park JD, Kim BI, Choi JH, Yun CK. Association of early postnatal neutropenia and development of bronchopulmonary dysplasia in preterm infants. J Korean Pediatr Soc 1998;41:1033–1060.14. Albertine KH, Carlton DP, Lont M, Davis PL, Bland RD. Pulmonary sequestration of neutrophils in preterm lambs with lung vascular injury. Pediatr Res 1994;35:1000038915. Gluck L, Kulovich MV. Lecithin-sphingomyelin ratios in amniotic fluid in normal and abnormal pregnancy. Am J Obstet Gynecol 1973;115:539–546.
[Article] [PubMed]16. Sibai BM. Hypertensive disorders of pregnancy: the United States perspective. Curr Opin Obstet Gynecol 2008;20:102–106.
[Article] [PubMed]17. Manroe BL, Weinberg AG, Rosenfeld CR, Browne R. The neonatal blood count in health and disease. I. Reference values for neutrophilic cells. J Pediatr 1979;95:89–98.
[Article] [PubMed]18. Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med 1993;329:1463–1466.
[Article] [PubMed]19. Morley CJ. In: Harvey D, Cooke UW, Levitt GA,Prevention of respiratory distress syndrome. editors. The baby under 1000 g. 1989London: Butterworth Co, :23–49.20. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001;163:1723–1729.
[Article] [PubMed]21. Young Infants Clinical Signs Study Group. Clinical signs that predict severe illness in children under age 2 months: a multicentre study. Lancet 2008;371:135–142.
[Article] [PubMed]22. Boxer LA. Immune neutropenias. Clinical and biological implications. Am J Pediatr Hematol Oncol 1981;3:89–96.
[PubMed]23. Christensen RD, Calhoun DA, Rimsza LM. A practical approach to evaluating and treating neutropenia in the neonatal intensive care unit. Clin Perinatol 2000;27:577–601.
[Article] [PubMed]24. La Gamma EF, Alpan O, Kocherlakota P. Effect of granulocyte colony-stimulating factor on preeclampsia-associated neonatal neutropenia. J Pediatr 1995;126:457–459.
[Article] [PubMed]25. Doron MW, Makhlouf RA, Katz VL, Lawson EE, Stiles AD. Increased incidence of sepsis at birth in neutropenic infants of mothers with preeclampsia. J Pediatr 1994;125:452–458.
[Article] [PubMed]27. Paul DA, Leef KH, Sciscione A, Tuttle DJ, Stefano JL. Preeclampsia does not increase the risk for culture proven sepsis in very low birth weight infants. Am J Perinatol 1999;16:365–372.
[Article] [PubMed]28. Yoon HS, Park SJ, Kim EA, Kim KS, Pi SY. Hematologic characteristics of neonates born to pregnancy-induced hypertensive mothers. J Korean Soc Neonatol 1998;5:158–166.29. Lee KJ, Yun SY, Lee R, Hean JH, Jung GY, Park JH, et al. Peripheral neutrophil count and respiratory failure in preterm infant. J Korean Pediatr Soc 2002;45:596–602.30. Chiswick ML. Prolonged rupture of membranes, pre-eclamptic toxaemia, and respiratory distress syndrome. Arch Dis Child 1976;51:674–679.
[Article] [PubMed] [PMC]31. Mouzinho A, Rosenfeld CR, Sanchez PJ, Risser R. Revised reference ranges for circulating neutrophils in very-low-birth-weight neonates. Pediatrics 1994;94:76–82.
[PubMed]32. Yoon JJ, Kohl S, Harper RG. The relationship between maternal hypertensive disease of pregnancy and the incidence of idiopathic respiratory distress syndrome. Pediatrics 1980;65:735–739.
[Article] [PubMed]33. Groneck P, Gotze-Speer B, Oppermann M, Eiffert H, Speer CP. Association of pulmonary inflammation and increased microvascular permeability during the development of bronchopulmonary dysplasia: a sequential analysis of inflammatory mediators in respiratory fluids of high-risk preterm neonates. Pediatrics 1994;93:712–718.
[Article] [PubMed]
Table 1
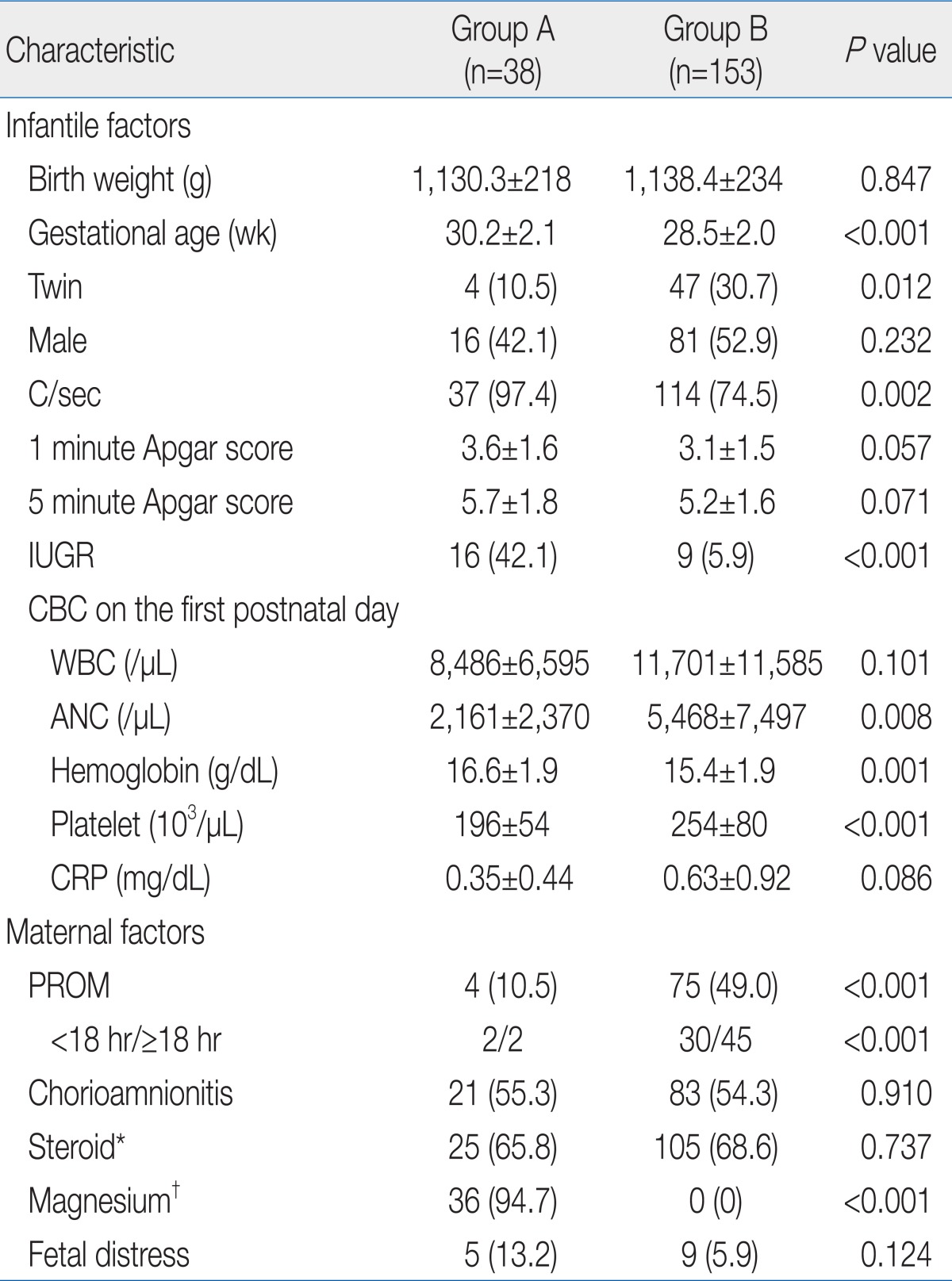
Values are presented as mean±SD or no. of patients (%).
PIH, pregnancy-induced hypertension; C/sec, cesarean section; IUGR, intrauterine growth restriction; CBC, complete blood count; WBC, white blood cell; ANC, absolute neutrophil count; CRP, C-reactive protein; PROM, premature rupture of membrane.
*Prenatal use of steroid. †Prenatal use of magnesium.
Table 2
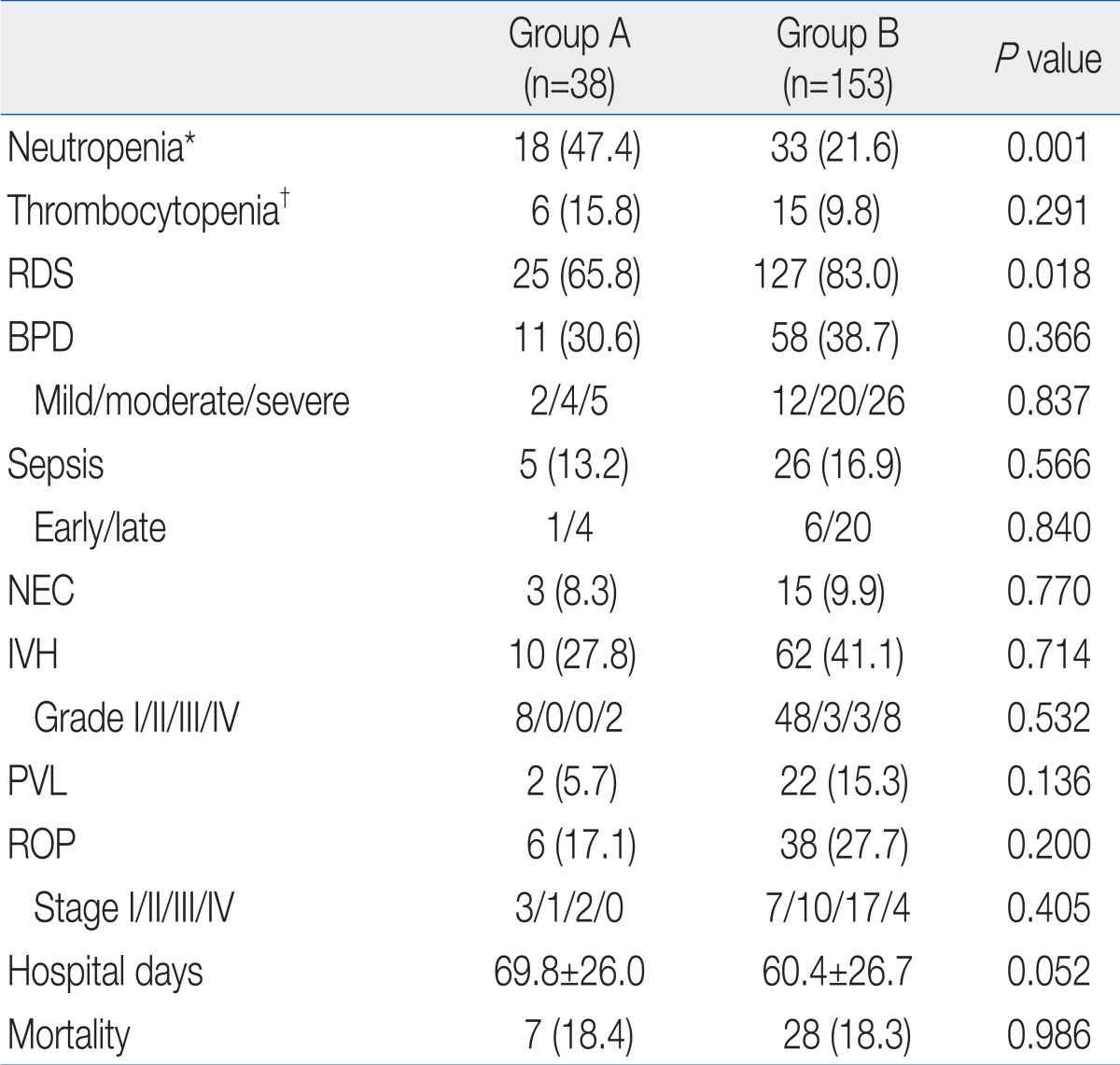
Values are presented as no. of patients (%) or mean±SD.
PIH, pregnancy-induced hypertension; RDS, respiratory distress syndrome; BPD, bronchopulmonary dysplasia; NEC, necrotizing enterocolitis; IVH, intraventricular hemorrhage; PVL, periventricular leukomalacia; ROP, retinopathy of prematurity.
*Neutropenia on the first postnatal day. †Thrombocytopenia on the first postnatal day.
Table 3
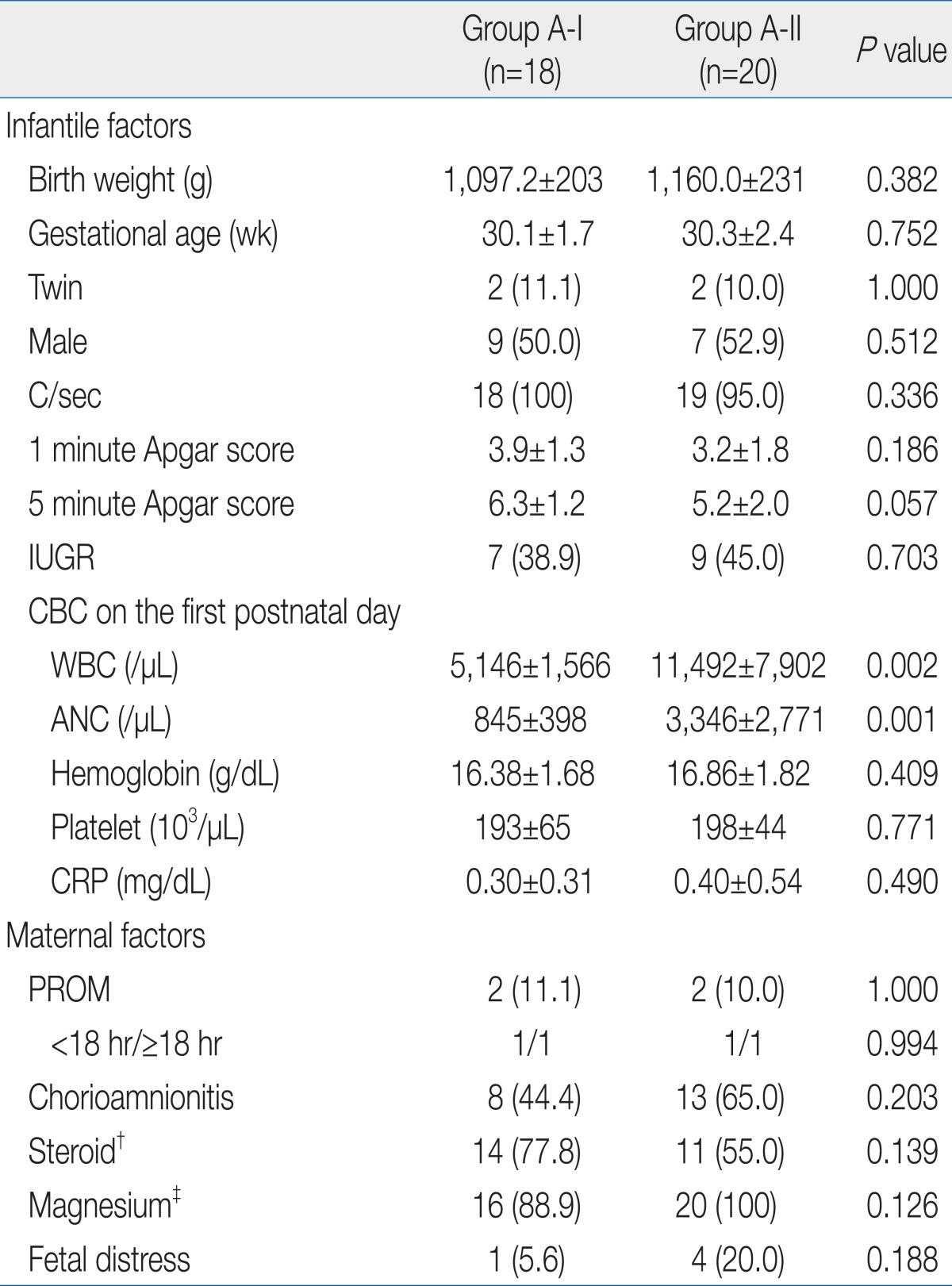
Values are presented as mean±SD or no. of patients (%).
C/sec, cesarean section; IUGR, intrauterine growth restriction; CBC, complete blood count; WBC, white blood cell; ANC, absolute neutrophil count; CRP, C-reactive protein; PROM, premature rupture of membrane.
*Neutropenia on the first postnatal day. †Prenatal use of steroid. ‡Prenatal use of magnesium.
Table 4
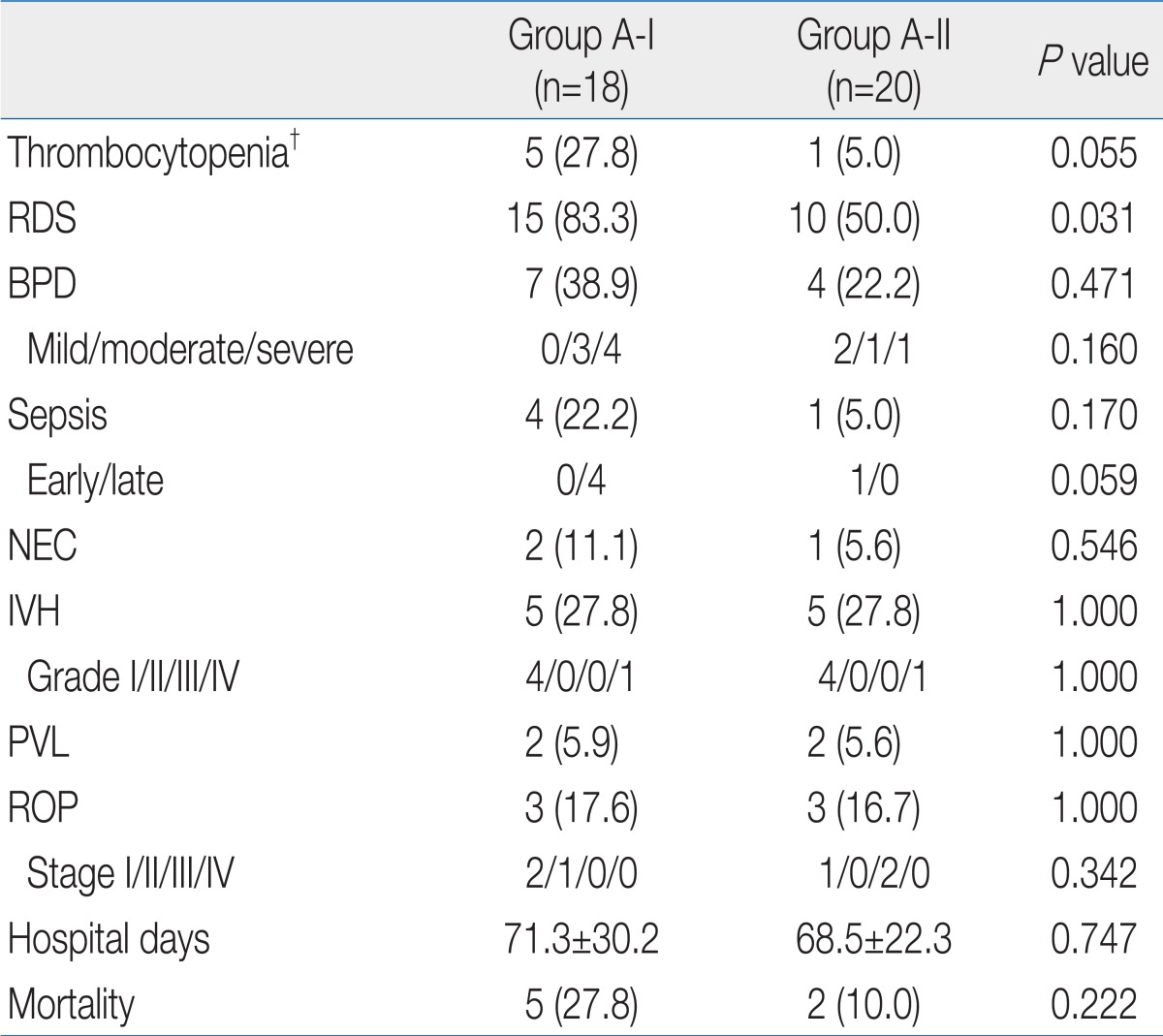
Values are presented as no. of patients (%) or mean±SD.
RDS, respiratory distress syndrome; BPD, bronchopulmonary dysplasia; NEC, necrotizing enterocolitis; IVH, Intraventricular hemorrhage; PVL, periventricular leukomalacia; ROP, retinopathy of prematurity.
*Neutropenia on the first postnatal day. †Thrombocytopenia on the first postnatal day.

 About
About Browse articles
Browse articles For contributors
For contributors