All issues > Volume 56(1); 2013
Orthostatic symptoms does not always manifest during tilt-table test in pediatric postural orthostatic tachycardia syndrome patients
- Corresponding author: Jung Sook Yeom, MD. Department of Pediatrics, Gyeongsang National University School of Medicine, 15 Jinju-daero 816beon-gil, Jinju 660-751, Korea. Tel: +82-55-750-8161, Fax: +82-55-752-9339, polo96@daum.net
- Received February 08, 2012 Revised June 28, 2012 Accepted October 23, 2012
- Abstract
-
- Purpose
- Purpose
- Chronic day-to-day symptoms of orthostatic intolerance are the most notable features of postural orthostatic tachycardia syndrome (POTS). However, we have encountered patients with such symptoms and excessive tachycardia but with no symptoms during the tilt-table test (TTT). We aimed to investigate whether POTS patients with chronic orthostatic intolerance always present orthostatic symptoms during the TTT and analyze the factors underlying symptom manifestation during this test.
- Methods
- Methods
- We retrospectively examined patients who presented with POTS at the Gyeongsang National University Hospital between 2008 and 2011. Diagnosis of POTS was based on chronic day-to-day orthostatic intolerance symptoms as well as excessive tachycardia during the TTT. The patients were divided two groups depending on the presentation of orthostatic symptoms during the TTT. Clinical data and the results of the TTT were compared between these groups.
- Results
- Results
- In 22 patients, 7 patients (31.8%) did not present orthostatic symptoms during the test. Diastolic blood pressure (BP) was significantly lower in the symptom-positive group. The head-up tilt resulted in a significant increase in diastolic BP in the symptom-negative group (P=0.04), while systolic BP had a tendency to decrease in the symptom-positive group (P=0.06).
- Conclusion
- Conclusion
- Significant patients with POTS did not present orthostatic symptoms during the TTT despite having chronic daily symptoms. This finding may be important for establishing definitive diagnostic criteria for pediatric POTS. Development of symptoms during TTT might be related to low diastolic BP and abnormal compensatory responses to orthostasis.
- Introduction
- Introduction
Postural orthostatic tachycardia syndrome (POTS) is a recently recognized orthostatic intolerance syndrome that was first officially defined by Schondorf and Low1) in 1993. It is the most common form of orthostatic intolerance in adults. Since the first published report of POTS in adolescents2), this syndrome has been increasingly recognized and characterized in symptomatic adolescents3). However, no consensus has been reached regarding the diagnostic criteria for pediatric populations, and to the best of our knowledge, only one diagnostic guideline for juvenile POTS is mentioned in Japanese clinical guidelines for juvenile orthostatic dysregulation4). The pediatric diagnostic criteria for POTS in Japan are as follows: increase in heart rate (HR) by ≥35 beats per minute (bpm) during standing or a HR of ≥115 bpm during active standing and no obvious hypotension. Unlike the diagnostic criteria for adult POTS, the pediatric criteria do not include orthostatic symptoms identified during the tilt-table test. The strict diagnostic guidelines for adult POTS state that this syndrome is diagnosed when sustained excessive tachycardia is noted during an upright tilt, accompanied by orthostatic symptoms during the test5,6). However, in clinical practice, we have encountered pediatric patients with chronic orthostatic symptoms and excessive tachycardia but no symptoms observed during the tilt-table test. Further, many healthy volunteers present the signs and symptoms of POTS during the tilt-table test but not in everyday life7). Stewart8) emphasized that chronic day-to-day orthostatic intolerance is the most notable clinical characteristic of POTS. Similarly, other researchers reported patients who developed chronic orthostatic symptoms on standing in clinical situations even though they showed no symptoms during the tilt-table test9,10). A recent study to establish diagnostic criteria for pediatric POTS also documented tilt table testing alone cannot capture the full spectrum of symptoms that patients with this syndrome frequently experience11).In this study, we diagnosed POTS on the basis of chronic day-to-day orthostatic intolerance symptoms as well as excessive tachycardia during the tilt-table test. Our aim was to investigate whether POTS patients with chronic orthostatic intolerance always presented orthostatic symptoms during the tilt-table test. Further, we analyzed factors associated with the manifestation of orthostatic symptoms during the tilt-table test.
- Materials and methods
- Materials and methods
- 1. Tilt-table test
- 1. Tilt-table test
Patients remained supine for 30 to 40 minutes while a baseline electrocardiograph and BP were recorded. They were then tilted to the head-up position at an angle of 70° held for 30 minutes. The HR and beat-to-beat BP were monitored continuously (Finapres Monitor, Ohmeda Medical, Englewood, CO, USA), and orthostatic symptoms were observed. Data of HR and BP variables were averaged (supine for 30 minutes and erect for 10 minutes).- 2. Automonic function tests
- 2. Automonic function tests
Cardiovagal, adrenergic, and postganglionic sudomotor functions were assessed as described below12), and previously published normative data were used to determine control values13).The quantitative sudomotor axon reflex test (QSART) was performed using the QSweat device (WR Electonics, Rochester, MN, USA) using the technique of Low et al.13) QSART records dynamic sweat output induced by chemically stimulating muscarinic eccrine sweat gland receptors with iontophoresis of acetylcholine and evaluates the postganglionic sympathetic sudomotor axon14).Cardiovagal function was assessed based on HR response to deep breathing and the Valsalva ratio12,13). Patients underwent controlled deep breathing six times per minute in which the longest and shortest R-R interval on electrocardiograph, inverted to a HR in bpm, was calculated as a sinus arrhythmia ratio. To test the Valsalva maneuver, the subject was placed in a recumbent position and asked to maintain a column of mercury at 40 mmHg for 15 seconds. The ratio of the maximal to the minimal HR defined the Valsalva ratio.Adrenergic function was assessed by the BP and HR responses to the Valsalva maneuver and the tilt-table test12,13).The composite autonomic severity score (CASS) was determined to grade the degree of autonomic dysfunction. The CASS is a semiquantitative score from 0 (no deficit) to 10 (maximal deficit) that combines the results of three subsets of autonomic tests and corrects for the effects of age and gender: sudomotor (range, 0 to 3), cardiovagal (range, 0 to 3), and adrenergic (range, 0 to 4)12).- 3. Statistical analysis
- 3. Statistical analysis
Descriptive statistics including the mean and standard deviation were used to describe the data distribution. A Wilcoxon signed-rank test was used to assess BP changes during the tilt table test within the same group; the Mann-Whitney U-test was used for between-group differences (the difference between the symptom-positive and symptom-negative groups). All tests were two-tailed. A P<0.05 was considered statistically significant. All statistical analyses were performed using SPSS ver. 12 (SPSS Inc., Chicago, IL, USA).
We undertook a retrospective study of patients who presented with POTS at the Gyeongsang National University Hospital, Jinju, South Korea, during a 3-year period (January 1, 2008 to March 30, 2011). The duration and frequency of the orthostatic intolerance symptoms, syncope history, and results of the tilt-table test were reviewed from the medical records of these patients.Inclusion criteria were as follows: 1) sustained HR increment of 35 bpm or greater in response to 10 minutes of tilt-table test, 2) baseline sinus rhythm with no evidence of arrhythmia, 3) symptoms of orthostatic intolerance such as light-headedness, weakness, palpitations, blurred vision, or nausea developing on standing or after tilt-table test and resolving with recumbency, and 4) these symptoms had to be present daily, almost daily, or several times a week for more than 3 months. The exclusion criteria were as follows: 1) orthostatic hypotension defined as a decline of 30 mmHg or more in systolic blood pressure (BP) or 20 mmHg or more in mean BP within 3 minutes of standing or tilt-table test, 2) episodic symptoms of orthostatic intolerance, or 3) systemic illness affecting autonomic function, such as congestive heart failure, cerebral palsy, and hypothyroidism.The patients were divided into two groups depending on whether they manifested orthostatic intolerance symptoms during the tilt-table test: the symptom-positive group and the symptom-negative group. We compared the clinical features, autonomic function tests, and results of the tilt-table tests between these groups.
- Results
- Results
- 1. Demographics
- 1. Demographics
During the study period, 65 patients underwent the tilt-table test for complaints of orthostatic intolerance, and 22 patients of them (33.8%) were diagnosed with POTS. Their ages ranged from 10 to 18 years, and most were male (72.7%).The following patients were excluded: 14 patients (21.5%) who met the HR increment criterion but had episodic symptoms, 4 (6.1%) who had orthostatic hypotension, 8 (12.3%) who had met the tachycardia criterion for POTS but whose BP dropped suddenly accompanied with syncope, and 1 who satisfied the diagnostic criteria for POTS but had dilated cardiomyopathy. Further, 16 patients (24.6%) showed no abnormalities in the tilt-table test.- 2. Comparison between the symptom-positive and symptom-negative groups
- 2. Comparison between the symptom-positive and symptom-negative groups
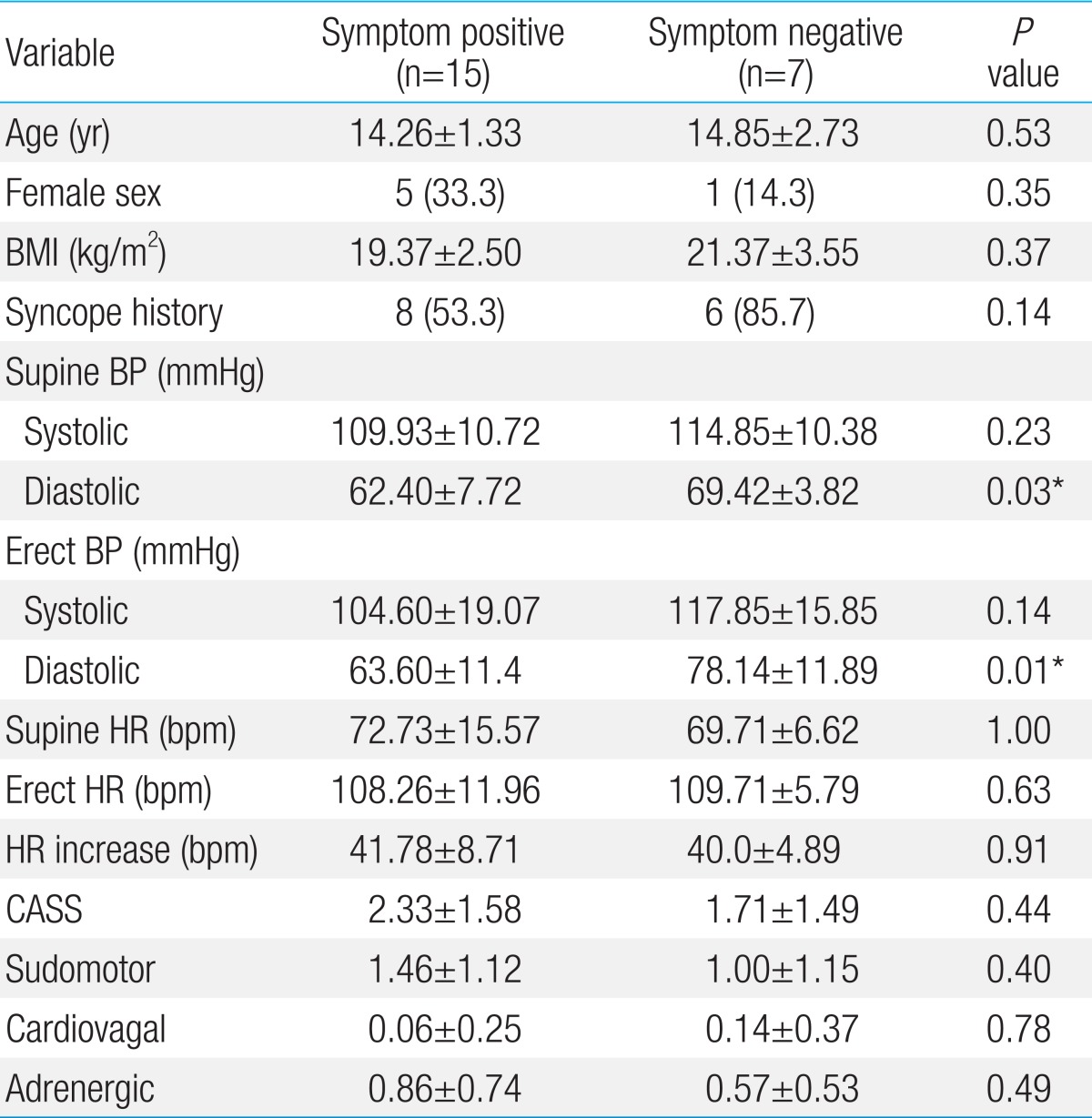
Table 1 shows the results obtained on comparison of various parameters between the symptom-positive and symptom-negative groups. Most patients (68.1%) experienced orthostatic symptoms during the tilt-table test. Age, gender, body mass index, and syncope history did not differ between the groups. No significant differences in HR and systolic BP variables, and results of autonomic function tests were observed between the groups. However, diastolic BPs (both supine and erect) were significantly lower in the symptom-positive group than those in the symptom-negative group (P=0.03 and P=0.01). The head-up tilt resulted in a significant increase in diastolic BP in the symptom-negative group (P=0.04) (Fig. 1). Systolic BP had a tendency to decrease in the symptom-positive group (P=0.06). The head-up tilt resulted in no significant change in either systolic or diastolic BP in this group (Fig. 1).
- Discussion
- Discussion
The most notable finding of our study is that a considerable number of POTS patients who were identified as actually having POTS manifested no symptoms during the tilt-table test. This finding may be important for establishing definitive diagnostic criteria for pediatric POTS, as thus far, no consensus has been reached about the diagnostic criteria for the pediatric population. In adult patients, POTS is diagnosed on the basis of a sustained HR increase of ≥30 bpm or an increase in HR to ≥120 bpm within the first 10 minutes of "orthostasis associated with symptoms of orthostatic intolerance" and without significant orthostatic hypotension15). However, POTS diagnosis may be difficult in clinical practice because interpretation of the phrase "orthostasis associated with symptoms of orthostatic intolerance" varies in the literature. Sandroni et al.5) and Ojha et al.6) insisted that for the diagnosis of POTS, orthostatic symptoms had to be manifested during the tilt-table test, while Thieben et al.9) and Peltier et al.10) included patients who developed chronic orthostatic symptoms on standing in clinical situations even if they showed no symptoms during the tilt-table test. The POTS diagnosis is more confusing in the case of pediatric patients. However, we considered inclusion criteria of Thieben et al.9) to be more reasonable and suited to the actual definition of POTS for the following reasons: Previous studies on orthostatic intolerance have reported that the sensitivity of the tilt-table test is low16). Wieling17) also reported that the initial phase of active standing caused more drastic hemodynamic changes than the tilt-table test, which clearly explains patient's symptoms of orthostatic intolerance. Moreover, Stewart8) emphasized that chronic day-to-day symptoms are characteristics of POTS and are the most notable differences between POTS and simple paint patients. Our study also demonstrated that a significant number of patients with POTS did not present orthostatic symptoms during the tilt-table test despite having chronic daily symptoms during active standing. On the basis of these findings, we infer that patients with chronic day-to-day symptoms of orthostatic intolerance should be diagnosed with POTS even if they manifest no symptoms during the tilt-table test.An important finding of our study was that diastolic BPs (both supine and erect) were significantly lower in the symptom-positive group of pediatric patients with POTS than those in the symptom-negative group. Head-up tilt resulted in an increase in both systolic and diastolic BP in the symptom-negative group; there was a significant increase in diastolic BP, in particular. In contrast, systolic BP decreased, whereas diastolic BP remained unchanged, in the symptom-positive group. Arterial BP is determined by several physical and physiological factors such as blood volume, elastic characteristics, HR, stroke volume, and peripheral resistance18). The most influential factor determining diastolic BP is peripheral resistance, and it is often asserted that decreased peripheral resistance affects diastolic more than systolic arterial pressure18,19). Although several factors should be considered, insufficient or abnormal peripheral resistance may have had an important role in lowering diastolic BP in the symptom-positive group.The symptom-negative group showed a normal compensatory response to orthostasis (increase in both systolic and diastolic BP), except for excessive tachycardia. However, systolic BP decreased and diastolic BP unchanged in the symptom-positive group, which may indicate an insufficient compensatory response to orthostasis. Decreased systolic BP during head-up tilt influences cerebral blood perfusion, which explained symptoms of orthostatic intolerance in the symptom-positive group. Ocon et al.20) suggested dynamic cerebral autoregulation is less effective in POTS patients based on a perfectly synchronous correlation between mean arterial pressure and cerebral blood f low velocity. Hemodynamic changes of symptom-positive group of our study and POTS patients in study of Ocon et al.20) are similar. They demonstrated cerebral blood f low velocity is significantly decreased in POTS patients during tilt20). Therefore, we hypothesized the decrease of systolic BP during head-up tilt in symptom-positive group of our study, seemed to be not obvious to break cerebral autoregulation, can cause a decrease of cerebral blood flow as a result of cerebral autoregulation dysfunction. Extrinsic factors also may aggravate cerebral blood flow. One such extrinsic factor may be the effect of hyperventilation, which produces hypocapnia and cerebral vasoconstriction21). However, we did not check hyperventilation during tilt-table test.Several physiological mechanisms maintain normal BP during orthostasis, including autonomic nervous system activation via baroreceptors and hormonal mechanisms such as adrenaline, norepinephrine, renin, angiotensin, and aldosterone18). No difference was observed in the autonomic function tests between the two groups. Therefore, we suggest that other compensatory mechanisms, rather than autonomic nervous system activation, were inadequate in the symptom-positive group.To the best of our knowledge, this is the first study to describe in detail the association between orthostatic symptom manifestation during the tilt-table test and the clinical and laboratory data of pediatric patients who meet the diagnostic criteria of POTS (HR increase without significant hypotension). However, this study has several limitations: First, the size of the patient population was small. Second, various factors such as volume status, peripheral blood flow, and norepinephrine levels are better bases to explain the manifestation orthostatic symptoms during the tilt-table test, but we did not evaluate these factors. Therefore, further studies should include an assessment of these factors with a large number of patients.In summary, a substantial number of POTS patients with chronic day-to-day orthostatic intolerance symptoms in this study did not present orthostatic symptoms during the tilt-table test. Diastolic BP was lower, and abnormal compensatory responses to orthostasis were found in the symptom-positive group compared with those in the symptom-negative group.
- References
- 1. Schondorf R, Low PA. Idiopathic postural orthostatic tachycardia syndrome: an attenuated form of acute pandysautonomia? Neurology 1993;43:132–137.
[Article] [PubMed]2. Stewart JM, Gewitz MH, Weldon A, Munoz J. Patterns of orthostatic intolerance: the orthostatic tachycardia syndrome and adolescent chronic fatigue. J Pediatr 1999;135(2 Pt 1): 218–225.
[Article] [PubMed]3. Johnson JN, Mack KJ, Kuntz NL, Brands CK, Porter CJ, Fischer PR. Postural orthostatic tachycardia syndrome: a clinical review. Pediatr Neurol 2010;42:77–85.
[Article] [PubMed]4. Tanaka H, Fujita Y, Takenaka Y, Kajiwara S, Masutani S, Ishizaki Y, et al. Japanese clinical guidelines for juvenile orthostatic dysregulation version 1. Pediatr Int 2009;51:169–179.
[Article] [PubMed]5. Sandroni P, Opfer-Gehrking TL, McPhee BR, Low PA. Postural tachycardia syndrome: clinical features and follow-up study. Mayo Clin Proc 1999;74:1106–1110.
[Article] [PubMed]6. Ojha A, McNeeley K, Heller E, Alshekhlee A, Chelimsky G, Chelimsky TC. Orthostatic syndromes differ in syncope frequency. Am J Med 2010;123:245–249.
[Article] [PubMed]7. de Jong-de Vos van Steenwijk CC, Wieling W, Johannes JM, Harms MP, Kuis W, Wesseling KH. Incidence and hemodynamic characteristics of near-fainting in healthy 6- to 16-year old subjects. J Am Coll Cardiol 1995;25:1615–1621.
[Article] [PubMed]8. Stewart JM. Postural tachycardia syndrome and reflex syncope: similarities and differences. J Pediatr 2009;154:481–485.
[Article] [PubMed]9. Thieben MJ, Sandroni P, Sletten DM, Benrud-Larson LM, Fealey RD, Vernino S, et al. Postural orthostatic tachycardia syndrome: the Mayo clinic experience. Mayo Clin Proc 2007;82:308–313.
[Article] [PubMed]10. Peltier AC, Garland E, Raj SR, Sato K, Black B, Song Y, et al. Distal sudomotor findings in postural tachycardia syndrome. Clin Auton Res 2010;20:93–99.
[Article] [PubMed]11. Singer W, Sletten DM, Opfer-Gehrking TL, Brands CK, Fischer PR, Low PA. Postural tachycardia in children and adolescents: what is abnormal? J Pediatr 2012;160:222–226.
[Article] [PubMed]12. Low PA. Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc 1993;68:748–752.
[Article] [PubMed]13. Low PA, Denq JC, Opfer-Gehrking TL, Dyck PJ, O'Brien PC, Slezak JM. Effect of age and gender on sudomotor and cardiovagal function and blood pressure response to tilt in normal subjects. Muscle Nerve 1997;20:1561–1568.
[Article] [PubMed]14. Low PA, Caskey PE, Tuck RR, Fealey RD, Dyck PJ. Quantitative sudomotor axon reflex test in normal and neuropathic subjects. Ann Neurol 1983;14:573–580.
[Article] [PubMed]15. Grubb BP, Kanjwal Y, Kosinski DJ. The postural tachycardia syndrome: a concise guide to diagnosis and management. J Cardiovasc Electrophysiol 2006;17:108–112.
[Article] [PubMed]16. Lai WT, Chen MR, Lin SM, Hwang HK. Application of head-up tilt table testing in children. J Formos Med Assoc 2010;109:641–646.
[Article] [PubMed]17. Wieling W. In: Bannister R,Standing, orthostatic stress and autonomic function. editor. A textbook of clinical disorders of the autonomic nervous system. 19882nd ed. Oxford: Oxford University Press, :308–320.18. Berne RM, Levy MN. In: Berne RM, Levy MN,The arterial system. editors. Cardiovascular physiology. 20018th ed. St. Louis: Mosby, :135–153.19. van den Bogaard B, Westerhof BE, Best H, Davis SC, Secher NH, van den Born BJ, et al. Arterial wave reflection decreases gradually from supine to upright. Blood Press 2011;20:370–375.
[Article] [PubMed]
Fig. 1
Blood pressure (BP) changes during the tilt-table test. (A) Systolic BP had a tendency to increase in the symptom-positive group (P=0.06). (B) The head-up tilt-table test resulted in increase in diastolic BP in the symptomnegative group with statistically significance (P=0.04), while no significant change in the symptom-positive group. SBP, systolic blood pressure; DBP, diastolic blood pressure; NS, non-significant. *Statistically significant (P<0.05).


 About
About Browse articles
Browse articles For contributors
For contributors