All issues > Volume 58(4); 2015
Ultrasound-guided internal jugular vein catheterization in critically ill pediatric patients
- Corresponding author: Sun Jun Kim, MD, PhD. Department of Pediatrics, Chonbuk National University Hospital, 20 Geonji-ro, Deokjin-gu, Jeonju 561-712, Korea. Tel: +82-63-250-1460, Fax: +82-63-250-1464, sunjun@jbnu.ac.kr
- Received June 23, 2014 Revised July 21, 2014 Accepted August 11, 2014
- Abstract
-
- Purpose
- Purpose
- Continuous intravenous access is imperative in emergency situations. Ultrasound-guided internal jugular vein (IJV) catheterization was investigated in critically ill pediatric patients to assess the feasibility of the procedure.
- Methods
- Methods
- Patients admitted to the pediatric intensive care unit between February 2011 and September 2012 were enrolled in this study. All patients received a central venous catheter from attending house staff under ultrasound guidance. Outcome measures included successful insertion of the catheter, cannulation time, number of cannulation attempts, and number and type of resulting complications.
- Results
- Results
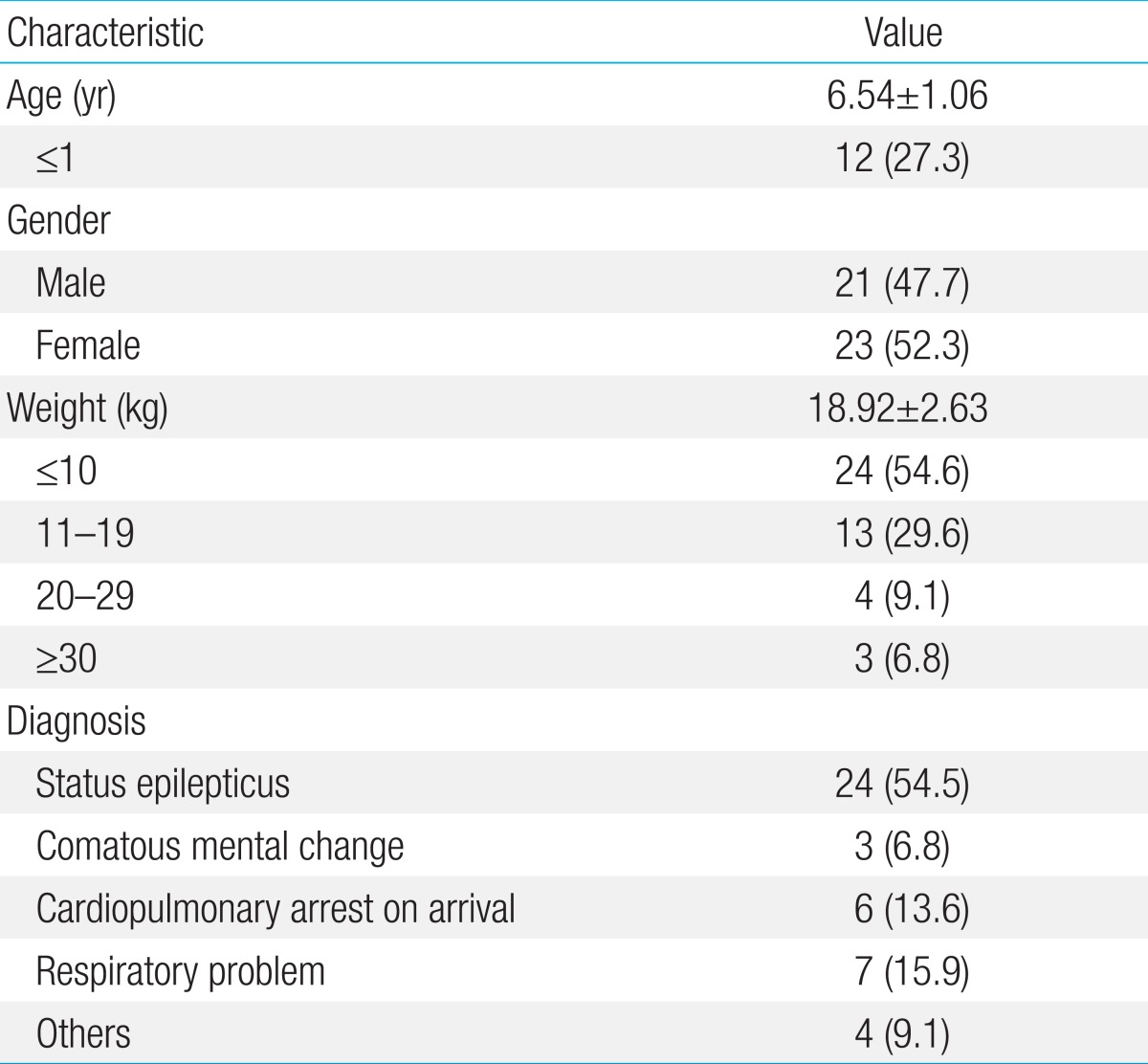
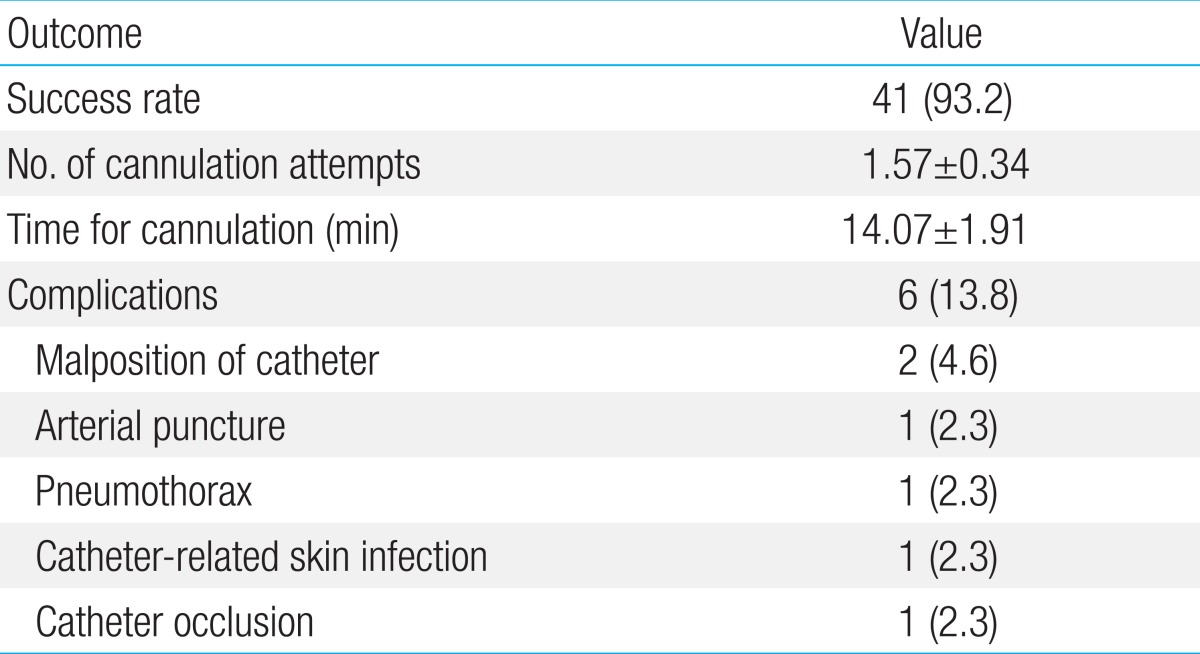
- Forty-one central venous catheters (93.2%) were successfully inserted into 44 patients (21 males and 23 females; mean age, 6.54±1.06 years). Thirty-three patients (75.0%) had neurological disorders. The right IJV was used for catheter insertion in 34 cases (82.9%). The mean number of cannulation attempts and the mean cannulation time was 1.57±0.34 and 14.07±1.91 minutes, respectively, the mean catheter dwell time was 14.73±2.5 days. Accidental catheter removal was observed in 9 patients (22.0%). Six patients (13.6%) reported complications, the most serious being catheter-related sepsis, which affected 1 patient (2.3%). Other complications included 2 reported cases of catheter malposition (4.6%), and 1 case each of arterial puncture (2.3%), pneumothorax (2.3%), and skin infection (2.3%).
- Conclusion
- Conclusion
- The results suggest that ultrasound-guided IJV catheterization can be performed easily and without any serious complications in pediatric patients, even when performed by visiting house staff. Therefore, ultrasound-guided IJV catheterization is strongly recommended for critically ill pediatric patients.
- Introduction
- Introduction
In emergency situations, intravenous routes for fluid management and drug administration are very important for the treatment of critically ill pediatric patients. Unfortunately, peripheral venous route access is often difficult to obtain for pediatric patients, especially those of whom who are critically ill or in emergency situations1). Moreover, some emergency or antiepileptic drugs can only be administered intravenously. Thus, other methods, such as the use of central venous cauterizations or intraosseous routes, are necessary to ensure effective treatment.Traditionally, central venous catheterization via the subclavian vein is the most reliable method for treating critical patients2,3). However, the potential for complications with this catheterization method is high, and its successful execution involves extreme technical difficulty. Therefore, this technique is only frequently used by highly-skilled doctors such as anesthesiologists, and not widely performed by pediatricians.Since ultrasound-guided internal jugular vein (IJV) catheterization was first described in 19774), many authors, particularly anesthesiologists, have reported its safety and advantages even for neonates5). However, pediatricians, and not anesthesiologists, are usually the first responders in children including neonate-related medical emergencies, and finding a catheterization specialist with the necessary skills may lead to a loss of time in an urgent situation. Therefore, in order to save time during these critical situations, pediatricians dealing with emergency patients should also be familiar with techniques that secure central venous access, such as ultrasound-guided central venous catheterization.The purpose of this study is to investigate the outcome in terms of success rate, number and type of resulting complications, and cannulation time of ultrasound-guided central vein catheterization through the IJV in critically ill pediatric patients.
- Materials and methods
- Materials and methods
This study was performed between February 2011 and September 2012 on patients admitted to the pediatric intensive care unit of Chonbuk National University Hospital. For the 44 critically ill pediatric patients enrolled in this study, central venous access was required for intensive care treatment, long-term intravenous treatment, or because a peripheral vein route was difficult to manage.Twenty-two patients required sedation through the use of intravenous midazolam (0.1 mg/kg) or ketamine (0.5-1.0 mg/kg). The other 22 patients were comatose and thus did not require sedation. Local anesthesia was not used for all patients. For all patients, a central catheter was inserted through the IJV via a real time ultrasound with a linear array transducer (5.0 to 8.0 MHz, Siemens, Munich, Germany) by multiple members of the pediatric attending house staff. The attending house staff members had all received annual training and ranged in experience from performing their first ultrasound-guided IJV catheterization to having previously performed up to 10 catheterizations. They underwent a common training course within the same facility, using the same ultrasound device.The IJV on each patient's right side was chosen for the primary insertion attempt. In the case that the initial attempt proved to be unsuccessful, other insertion sites were considered. Before the procedure was performed, the depth, size and position of the IJV were measured (Fig. 1). In addition, it was confirmed in advance that the vein could be compressed via the gentle pressure of a probe on the skin, and that a pulse was present in the carotid artery.Since the ultrasound-guided technique explained above requires preparation time, the house staff measured the IJV cannulation time in minutes from the time of skin puncture to the time at which the catheter was inserted into the vein. After its location was carefully selected, the puncture site was then covered, and the probe was sanitized with a sterilized sheath and conductive gel. An image of the patient's IJV was then projected onto the ultrasound screen in order to ensure that the needle was centered in the middle of the vein. After the venipuncture, blood was aspirated into the syringe. Next, the probe and syringe were removed and a round-tipped guide wire was advanced through the lumen of a 22- or 24-gauge hollow needle, which was then withdrawn. The 4.0 or 5.0-Fr double-lumen or 5.5-Fr three-lumen central venous catheter kit was chosen based on the patient's weight and age. The guide wire, covered by a blunt cannula throughout the length of the vein, was used to insert the central venous catheter (Seldinger technique). Within 1 hour of catheter insertion, a chest x-ray was routinely taken and after analyzing the results, the catheter was then fixed by skin attachment (DuoDERM Extra Thin CGF, ConvaTec, Greensboro, NC, USA).Outcome measures included the patient's age and bodyweight, the success rate of catheter insertion, cannulation time of the IJV, the number of puncture attempts, and the occurrence of any complications.
- Results
- Results
Forty-four pediatric patients (21 males and 23 females) were enrolled in this study. The mean age was 6.54±1.06 years, ranging from 1 month to 16.2 years (Table 1). Out of 44 patients, 33 patients (75.0 %) had neurological disorders such as status epilepticus (24 cases, 54.6%), a comatose mental state (3 cases, 6.8%) and cardiopulmonary arrest on arrival (6 cases, 13.6%). Seven patients (15.9%) had desaturation and respiratory problems, and four patients (9.1%) had conditions that rendered normal access to peripheral venous routes impossible.The mean body weight was 18.9±2.63 kg and ranged from 2.5 kg to 28.8 kg. Eighteen patients (40.9%) had a weight of less than 10 kg and 12 patients (27.3%) were younger than one year of age. Thirty-nine out of 44 patients (88.6%) were admitted to the pediatric intensive care unit, and 31 patients (70.5%) were on a ventilator. The success rate of IJV catheter insertion was 93.2% (41 cases, Table 2). In three cases which was unsuccessful at both right and left subclavian attempt, the femoral vein in angiography was chosen. Out of the 41 successful IJV insertion attempts, catheters were inserted on the right side of 34 patients (82.9%). For the seven cases in which the initial IJV insertion attempt was unsuccessful, the patient's left side was then chosen for catheter insertion (17.1%).The mean number of attempts necessary to successfully perform IJV catheterization was 1.57±0.34 and ranged from one to four attempts (Table 2). The mean IJV cannulation time was 14.07±1.91 minutes and ranged in span from 1.5 to 37.0 minutes.The average duration use of the central venous catheter was 14.73±2.5 days, with the total range spanning between 1 and 62 days. Accidental catheter removals were noted in nine patients (22.0%). Eight of these nine patients reported this unplanned removal to be the result of their own actions, either taking hold of the catheter in their hands or making voluntary movements to dislodge the catheter. The one remaining case of accidental catheter removal was attributed to inappropriate handling by the staff.All complications related to catheterization were investigated (Table 2). These complications included arterial puncture in one patient (2.3%) and the malposition of the catheter in two cases (4.6%). These complications did not give rise to any major problems. Additionally, one patient developed pneumothorax (2.3%), which required placement of a chest tube for 3 days. One patient (2.3%) each developed catheter-related skin infection and catheter occlusion respectively. The isolation of organisms from the catheter or blood was not reported in either case, and both patients exhibited clinical improvement after the catheter was removed. Insertion complications from the central venous catheter did not result in morbidity or mortality.
- Discussion
- Discussion
Central venous catheterization is used in cases in which a lack of access renders it impossible to administer medication via the peripheral veins of infants and children. Central venous catheterization offers safer, more rapid, and more effective vascular access in emergency and critical situations. Many previous studies have shown ultrasound-guided catheterization to be superior to the landmark technique of catheterization1,6,7,8); the results of this study are consistent with such findings. For example, ultrasound-guided catheterization of the IJV was successful in all infants (100%) and in 40 of 52 (77%) or 24 of 30 infants (80%) in the landmarks group in the previous studies6,8). In particular, Verghese et al.1) have demonstrated a significantly lower catheterization time and the reduced incidence of carotid artery punctures in infants and children when using the ultrasound technique as compared with the landmark technique. However, some studies show there is insufficient evidence to support the use of ultrasound-guided catheterization9). Furthermore, meta-analysis in children and infants has shown that ultrasound-guided catheterization has had no effect on the failure rate or incidence of complications as compared with the anatomical landmark technique10).Central venous catheterization is more difficult in pediatric patients than in adult patients due to the smaller dimensions of the IJV in infants and children, particularly the size of its diameter11). As a result, more insertion attempts are often necessary before successful catheterization can be performed in pediatric patients, and as the number of insertion attempts increases, so too does the risk of complications such as carotid artery puncture.Although the vascular anatomy of infants has been assessed in only a few studies, it is clear that cervical vessel anatomy in children is more variable than in adults12,13). Thus, the major advantage of the ultrasound-guided technique lies in its ability to provide a visual of the structures at the puncture site before catheterization is attempted. Ultrasound also allows for the confirmation of anatomical variations related to the IJV-carotid artery relationship. The IJV is normally located laterally to the carotid artery. The few studies that have been published on the vascular anatomy of infants and children have shown that the position of the IJV is variable and can be located in an anterior position, anteriolateral position, or lateral position to the carotid artery12,13,14,15,16). We investigated the IJV is found to be anterior to the carotid artery in 28 of cases, anterolateral in three patient and lateral in ten of the cases.A central venous catheter is usually inserted into the femoral, internal jugular, or subclavian vein. There are both advantages and disadvantages at each puncture site. Therefore, choosing a puncture site depends on the intended purpose of the central venous catheter. Since 2002, the use of ultrasound guidance for central vein catheterization into the IJV has been recommended for children by the United Kingdom National Institute for Clinical Excellence5). This study focused on IJV catheterization for several reasons. In the IJV approach, the carotid artery pulse can be easily observed by ultrasound, thus preventing arterial puncture. In addition, the IJV is located close to the skin and is therefore easy to compress by ultrasound17).In some studies, techniques using the subclavian vein also yielded positive results2,3). A subclavian vein puncture has some benefits over an IJV puncture. First of all, the subclavian vein is fixed to the clavicle. Therefore, the collapse of the vascular anterior wall under the pressure of a needle can be avoided. Secondly, in infants less than 1 year of age, the subclavian vein is in a nearly extrathoracic position before reaching the innominate vein. Lastly, the subclavian vein is often the preferred site for long-term central venous catheter placement in children3). However, since the right subclavian vein enters the central venous system at an acute angle, sometimes the catheter is inserted into the opposite side of the innominate vein or IJV.Some studies reported both the central venous catheter access time and the number of skin puncture attempts6,7,8,9,14). In those studies, the mean time of cannulation of the IJV with ultrasound was reported as ranging from 2 to 4.5 minutes, which is significantly less time than with the landmark technique. However, meta-analysis found ultrasonographic guidance to have no influence over the access time as compared to with traditional techniques10). Since the ultrasound-guided technique requires some preparation time for anatomical screening and equipment preparation as discussed above, ultrasound-guided central venous catheterization can take more time in practice. However, taking into consideration that the mean time of cannulation was measured as 14.07±1.91 minutes in this study, it is clear that ultrasound-guided central venous catheterization is rapid and reliable enough to secure venous access in emergency situations. Additionally, the ultrasound-guided technique in this study significantly reduced the number of cannulation attempts. In this sense, Verghese et al.6) have explained the mean time of cannulation of the IJV was definitely less with the ultrasound-guided technique (4.2±2.8 minutes) than with the landmarks technique (14.0±15.1 minutes) (P<0.0004). Also, the mean number cannulation of attempts with the ultrasound-guided technique (1.3±0.6) was also significantly less than with the landmarks method (3.3±2.8) (P<0.0001)6). The mean number of skin puncture attempts was 1.3 to 1.57 times higher in previous studies that used more traditional techniques, but meta-analysis reported that ultrasonographic guidance decreased the number of skin puncture attempts10). That said, such results were directly related to the practitioner's experience, hand skill, and sample size, all potential confounding factors.Central venous catheterization is usually related to the practitioner's experience and hand skill. Interestingly, in the landmark procedures, between the preeducation and posteducation periods there was no difference between the central venous catheterizations performed by fellows and those performed by attending house staff18). In many previous studies, pediatric anesthesia fellows or experts accessed the central venous catheter but this study was conducted exclusively by attending house staff with variable experience. This study, in demonstrating no significant difference in terms of success rate, access time, or incidence of complications, reveals that ultrasound-guided central venous catheterization is a suitable technique for any attending house staff in the medical field to perform. Adequate training and more experience can increase both the success rate and hand skill of such staff.Although catheter permanence (mean duration, 14.73±2.5 days) in this study was longer than in other previous studies19), accidental catheter removal was frequently noted (22.0%). These accidental removals were mainly caused by the patient's movement, but in one case it was attributed to a mistake made by the staff. Skin attachments were only used as a last resort in order to fix the catheter without having to give the patient sutures. In the future, alternative ways to fix the catheter should be investigated.The most common complication of central venous catheterization is an arterial puncture or hematoma. In this study, the incidence of carotid artery puncture was 2.3%, a more successful result (0%-11.9%) in comparison with previous studies6,7,8,9). And no arterial or venous hematoma occurred in our study. Though few previous studies have shown that the ultrasound-guided technique has any effect on the rate of arterial puncture, the incidence of carotid artery puncture was decreased in this study because ultrasound guidance allowed for the visualization and distinction of the patients' arteries and veins. There was only one patient developed pneumothorax in the entire study. The result of the incidence of pneumothorax was similar to other studies6,8,19).The long-term complications of central venous catheters in children are thrombotic and infectious complications20). This study involved one case of each developed catheter-related skin infection and catheter occlusion. The patient with catheter-related skin infection had erythema of skin at the insertion site. but any localizing signs or symptoms including fever were not reported. No organism from the catheter or blood was reported, and the patients exhibited clinical improvement after the catheter was removed. In a pediatric intensive care unit setting, the risk of bloodstream infections related to central venous catheters increases significantly after 7 days21). The American Pediatric Surgical Association recommends strategies for the prevention of central venous catheter infections22). The first of these is chlorhexidine skin preparation and chlorhexidine-impregnated dressing. The second suggestion is the use of heparin and an antibiotic-impregnated central venous catheter. Finally, ethanol and vancomycin lock therapy is recommended.Until now, ultrasound-guided IJV catheterization has been widely performed by anesthesiologists, but not frequently used by pediatricians. This study shows that ultrasound-guided IJV catheterization is not only an efficient and easy technique to use for infant and children patients, but also highly successful and very safe to perform not only by pediatric specialists but by attending house staff as well.
- Conflicts of interest
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
- References
- 1. Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE. Internal jugular vein cannulation in infants: palpation vs imaging. Anesthesiology 1996;85:10782. Pirotte T, Veyckemans F. Ultrasound-guided subclavian vein cannulation in infants and children: a novel approach. Br J Anaesth 2007;98:509–514.
[Article] [PubMed]3. Citak A, Karabocuoglu M, Ucsel R, Uzel N. Central venous catheters in pediatric patients--subclavian venous approach as the first choice. Pediatr Int 2002;44:83–86.
[Article] [PubMed]4. Ullman JI, Stoelting RK. Internal jugular vein location with the ultrasound Doppler blood flow detector. Anesth Analg 1978;57:118
[Article] [PubMed]5. National Institute for Clinical Excellence. NICE technology appraisal guidance No. 49: guidance on the use of ultrasound locating devices for placing central venous catheters. London: NICE, 2002.6. Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE. Ultrasound-guided internal jugular venous cannulation in infants: a prospective comparison with the traditional palpation method. Anesthesiology 1999;91:71–77.
[Article] [PubMed]7. Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE. Comparison of three techniques for internal jugular vein cannulation in infants. Paediatr Anaesth 2000;10:505–511.
[Article] [PubMed]8. Chuan WX, Wei W, Yu L. A randomized-controlled study of ultrasound prelocation vs anatomical landmark-guided cannulation of the internal jugular vein in infants and children. Paediatr Anaesth 2005;15:733–738.
[Article] [PubMed]9. Grebenik CR, Boyce A, Sinclair ME, Evans RD, Mason DG, Martin B. NICE guidelines for central venous catheterization in children. Is the evidence base sufficient? Br J Anaesth 2004;92:827–830.
[Article] [PubMed]10. Sigaut S, Skhiri A, Stany I, Golmar J, Nivoche Y, Constant I, et al. Ultrasound guided internal jugular vein access in children and infant: a meta-analysis of published studies. Paediatr Anaesth 2009;19:1199–1206.
[Article] [PubMed]11. Sayin MM, Mercan A, Koner O, Ture H, Celebi S, Sozubir S, et al. Internal jugular vein diameter in pediatric patients: are the J-shaped guidewire diameters bigger than internal jugular vein? An evaluation with ultrasound. Paediatr Anaesth 2008;18:745–751.
[Article] [PubMed]12. Cobb LM, Vinocur CD, Wagner CW, Weintraub WH. The central venous anatomy in infants. Surg Gynecol Obstet 1987;165:230–234.
[PubMed]13. Steinberg C, Weinstock DJ, Gold JP, Notterman DA. Measurements of central blood vessels in infants and children: normal values. Cathet Cardiovasc Diagn 1992;27:197–201.
[Article] [PubMed]14. Lamperti M, Caldiroli D, Cortellazzi P, Vailati D, Pedicelli A, Tosi F, et al. Safety and efficacy of ultrasound assistance during internal jugular vein cannulation in neurosurgical infants. Intensive Care Med 2008;34:2100–2105.
[Article] [PubMed]15. Alderson PJ, Burrows FA, Stemp LI, Holtby HM. Use of ultrasound to evaluate internal jugular vein anatomy and to facilitate central venous cannulation in paediatric patients. Br J Anaesth 1993;70:145–148.
[Article] [PubMed]16. Mallinson C, Bennett J, Hodgson P, Petros AJ. Position of the internal jugular vein in children. A study of the anatomy using ultrasonography. Paediatr Anaesth 1999;9:111–114.
[Article] [PubMed]17. Kim KO, Jo JY, Oh AY, Kim HS, Kim CS. Optimal depth of insertion of CVP catheter using the right third intercostal space in children. Korean J Ped Anesth 2002;6:86–90.18. Sekiguchi H, Tokita JE, Minami T, Eisen LA, Mayo PH, Narasimhan M. A prerotational, simulation-based workshop improves the safety of central venous catheter insertion: results of a successful internal medicine house staff training program. Chest 2011;140:652–658.
[Article] [PubMed]19. Asheim P, Mostad U, Aadahl P. Ultrasound-guided central venous cannulation in infants and children. Acta Anaesthesiol Scand 2002;46:390–392.
[Article] [PubMed]20. Sol JJ, van Woensel JB, van Ommen CH, Bos AP. Long-term complications of central venous catheters in children. Paediatr Child Health 2007;17:89–93.
[Article]21. Casado-Flores J, Barja J, Martino R, Serrano A, Valdivielso A. Complications of central venous catheterization in critically ill children. Pediatr Crit Care Med 2001;2:57–62.
[Article] [PubMed]22. Huang EY, Chen C, Abdullah F, Aspelund G, Barnhart DC, Calkins CM, et al. Strategies for the prevention of central venous catheter infections: an American Pediatric Surgical Association Outcomes and Clinical Trials Committee systematic review. J Pediatr Surg 2011;46:2000–2011.
[Article] [PubMed]

 About
About Browse articles
Browse articles For contributors
For contributors