|
Question: Hospitalization in neonatal intensive care unit (NICU) is associated with life-threatening hazards. What factors associated with neonatal length of stay (LOS) in the NICU?
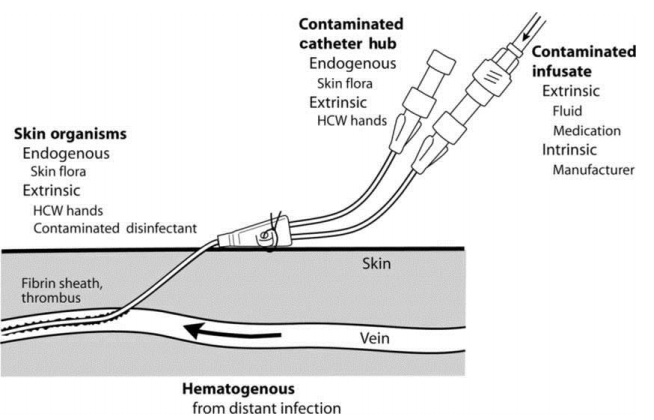
Finding: Breastfeeding, phototherapy, acute renal failure (ARF), mechanical ventilation, and central venous catheter (CVC) access were identified as factors associated with NICU length of stay.
Meaning: Protective effects of breastfeeding and CVC access, whereas increase effects of phototherapy, ARF, and mechanical ventilation in LOS can be supporting evidence to establish effective interventions to reduce length of NICU stay. |