Infection
- Page Path
-
- HOME
- TOPICS
- Infection
- Topics
-
- Adolescence Medicine (4)
- Allergy (64)
- Cardiology (81)
- Critical Care Medicine (15)
- Developmental and Behavioral Medicine (24)
- Emergency Medicine (5)
- Endocrinology (65)
- Gastroenterology (76)
- General Pediatrics (58)
- Genetics and Metabolism (26)
- Hematology (20)
- Immunology (16)
- Infection (82)
- Neonatology (Perinatology) (127)
- Nephrology (Genitourinary) (54)
- Neurology (96)
- Nutrition (33)
- Oncology (19)
- Neurobehavior (12)
- Pulmonology (35)
- Rheumatology (4)
- Other (44)
- Guideline
- Infection
- Recommendation for use of 15- and 20-valent pneumococcal conjugate vaccines in Korean infants and children
- Ki Wook Yun, Dong Hyun Kim, Jong Gyun Ahn, Byung-Wook Eun, Jin Lee, Jina Lee, Taek-Jin Lee, Hyunju Lee, Dae Sun Jo, Eun Young Cho, Hye-Kyung Cho, Soo-Han Choi, Young June Choe, Ui Yoon Choi, Yun-Kyung Kim; The Committee on Infectious Diseases of the Korean Pediatric Society
- Clin Exp Pediatr. 2026;69(1):76-83. Published online December 30, 2025
-
Compared to PCV13, PCV15 includes 2 (22F and 33F), and PCV20 includes 7 (8, 10A, 11A, 12F, 15B, 22F, and 33F) additional serotypes. The vaccination schedule remains the same: primary doses at 2, 4, and 6 months, and a booster at 12–15 months. If PCV13 was administered in the primary series, PCV15 and PCV20 may be used to complete it or as a booster.
- Original Article
- Infection
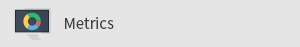
- Clinical outcomes and healthcare utilization of hospitalized children with influenza versus COVID-19
- David Chun-Ern Ng, Chuin-Hen Liew, Kah Kee Tan, Joanne Pereira, Muhammad Ihsan Roslan, Xiang Lin Cheng, Hui Yi Lim, Farah Nuruliayana A. Nazri, Asuwani Maran, Wan Fei Wong, Yasothai Chandran, Syaniza Shaharudin, Pon Ling Lau, Naveen Nair Gangadaran, Marlindawati Mohd Ali
- Clin Exp Pediatr. 2025;68(12):1007-1014. Published online October 2, 2025
-
Question: How do clinical presentations, healthcare resource utilization, and outcomes differ between children hospitalized with influenza versus coronavirus disease 2019 (COVID-19)?
Finding: Patients with influenza were older, were more symptomatic, and required greater healthcare resources, including intravenous fluids, empirical antibiotics, respiratory support, and pediatric intensive care unit admission.
Meaning: Influenza involves greater severity and a higher healthcare burden than COVID-19, highlighting the need for preventive strategies such as vaccination and hospital resource planning during seasonal outbreaks.
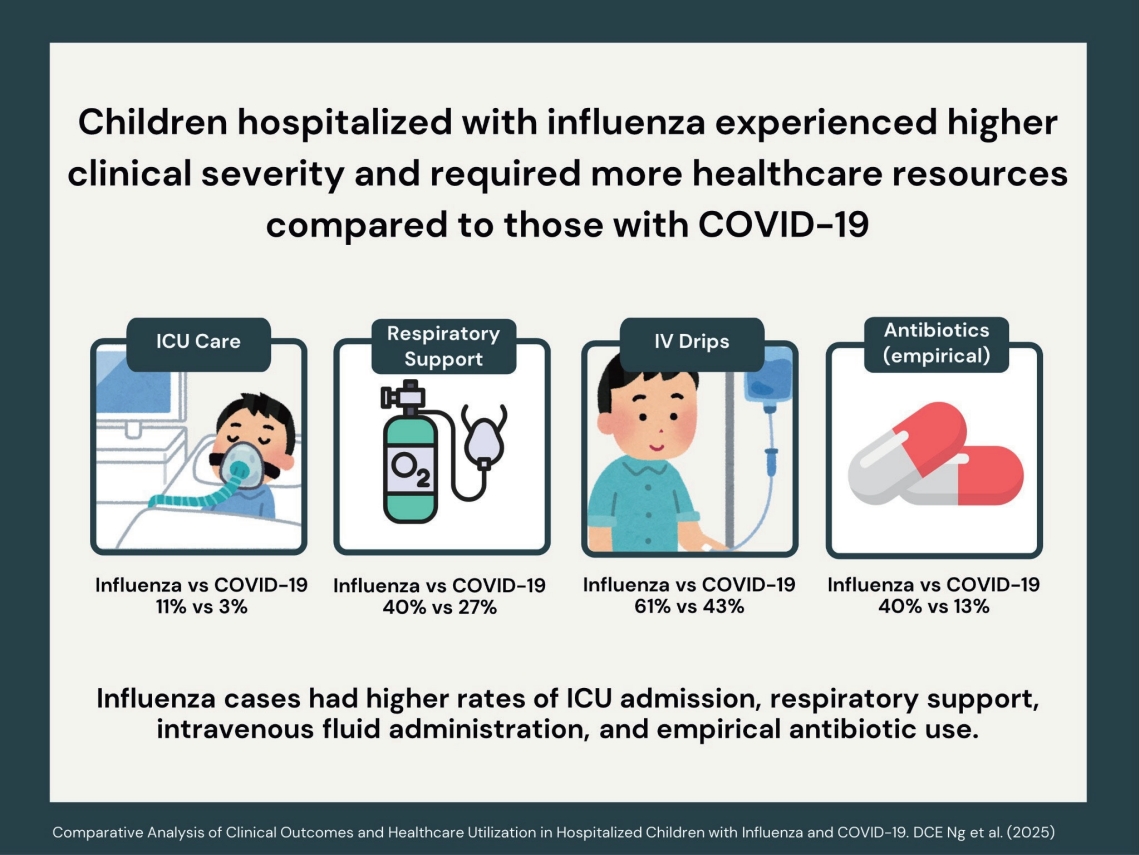
- Association between vitamin D polymorphisms and binding protein and COVID-19 risk and severity in children
- Victoria Giatraki, Helen Dimitriou, Georgia Martimianaki, Christos Tsatsanis, Emmanouil Galanakis, Chrysoula Perdikogianni
- Clin Exp Pediatr. 2025;68(12):998-1006. Published online October 22, 2025
-
Question: Addressing crucial genetic variants within the vitamin D pathway and coronavirus disease 2019 (COVID-19) susceptibility, the vitamin D receptor, vitamin D binding protein, and CYP27B1-1260 polmorphisms might be associated with COVID-19 occurrence and severity in children.
Finding: The FokI FF genotype might be an independent risk factor for COVID-19 severity in childhood.
Meaning: This research may further elucidate genetic susceptibility to multisystem viral infections and establish genetic markers for severe clinical outcomes.
- Editorial
- Infection
- Beyond COVID-19: meeting the challenge of evolving pediatric invasive group A streptococcal disease
- Han Wool Kim
- Clin Exp Pediatr. 2025;68(12):971-973. Published online November 26, 2025
-
Pediatric for invasive group A Streptococcus has resurged globally with increasing severity and toxin-mediated presentations. Beta-lactams remain the first-line treatment, but linezolid has emerged as a safe alternative in cases refractory to β-lactams. Early intravenous immunoglobulin use may improve outcomes in severe streptococcal toxic shock syndrome cases, while C-reactive protein and procalcitonin aid early risk stratification. Integrating global surveillance and individualized therapy is crucial in the postpandemic era.
- Original Article
- Infection
- Evolving treatment strategies for invasive Streptococcus pyogenes in children in the postpandemic era
- Laura Buricchi, Giuseppe Indolfi, Marco Renni, Elisabetta Venturini, Luisa Galli, Elena Chiappini
- Clin Exp Pediatr. 2025;68(11):921-931. Published online August 11, 2025
-

Question: What are the roles of linezolid, intravenous immunoglobulin (IVIG), and corticosteroids in pediatric invasive group A streptococcal infection (iGAS)? Can any improve outcomes beyond beta-lactams and clindamycin?
Finding: Two of 46 patients with iGAS died. Nearly all received beta-lactams plus clindamycin. Linezolid was effective in refractory cases. IVIG and corticosteroids had variable efficacies.
Meaning: Linezolid may be valuable in refractory cases. IVIG may be considered in severe presentations. The role of corticosteroids remains less clearly defined.
- Serum copper and ceruloplasmin levels as biomarkers reflecting liver fibrosis in children with autoimmune hepatitis
- Salma Abdel Megeed Nagi, Mai Ibrahim Elashmawy, Amany E. Elashkar, Mohamed Zaeim Hafez, Ashraf A.E. Emara, Osama Mohammad Abdelhay, Albayoumi A.B. Fouda, Mohamed AbdelAziz Doma, Ahmad Mohamed Awad, Ahmed Mohammed Saba, Hesham Abdelrahman Ahmed, Ahmed Mohamed Gad Allah, Fatma Mahmoud Abdelraheem, Mohamed A. Gad, Mohamad A. Soliman, Tamer I. Abdalrhman, Khaled Hassaan Awad, Ismael A.K.M. El-lebedy, Mostafa M. Abdelnaser, Mohammed Z. Abdel Kareem, Marwa Fekry Hassan, Shymaa Sobhy Menshawy Khalifa
- Clin Exp Pediatr. 2025;68(11):909-920. Published online August 6, 2025
-

· A total of 159 children with autoimmune hepatitis (AIH; 60.3% female, 13.2% type 2 AIH) were identified. According to a global study, the estimated annual incidence of AIH in Egypt is 1.28 cases per 100,000 inhabitant-years.
· No studies to date have examined the serum levels of copper or ceruloplasmin in children with AIH. Therefore, here we investigated whether serum copper and ceruloplasmin levels are useful for identifying liver fibrosis in children with AIH.
· Serum copper and ceruloplasmin levels may provide important information for the identification of advanced liver fibrosis in children with AIH.
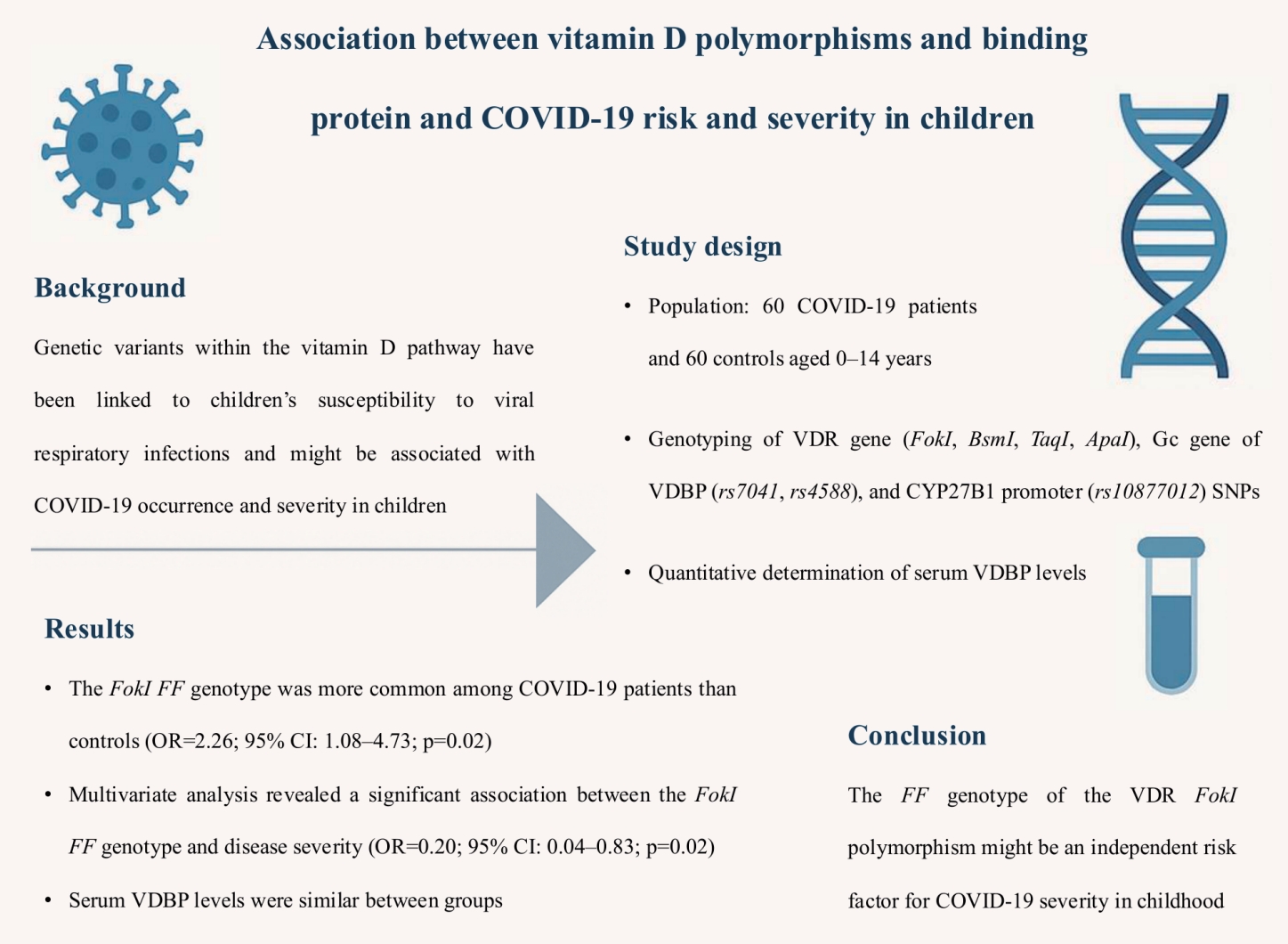
- Role of miRNA-146a and miRNA-125b in Helicobacter pylori
- Nashwa Farouk Mohamed, Ola G.A. Behairy, Manal S. EL-Defrawy, Mona Mahmoud Elsayed, Naglaa F. Alhusseini
- Clin Exp Pediatr. 2025;68(10):781-789. Published online April 1, 2025
-
Question: Why is the early detection of Helicobacter pylori-associated gastritis in children important?
Finding: The early detection of H. pylori-related gastritis is crucial for its effective management, especially in pediatric patients with dyspepsia.
Meaning: The use of miRNA signatures could detect early gastritis, enabling timely H. pylori eradication treatment to mitigate growth delays and cancer risk.
- Review Article
- Infection
- Recommendation for use of a long-acting monoclonal antibody to prevent respiratory syncytial virus infection in infants and young children
- Soo-Han Choi, Dong Hyun Kim, Jong Gyun Ahn, Ki Wook Yun, Byung-Wook Eun, Jin Lee, Jina Lee, Taek-Jin Lee, Hyunju Lee, Dae Sun Jo, Eun Young Cho, Hye-Kyung Cho, Young June Choe, Ui Yoon Choi, Yun-Kyung Kim; The Committee on Infectious Diseases of the Korean Pediatric Society
- Clin Exp Pediatr. 2025;68(10):742-750. Published online September 3, 2025
-
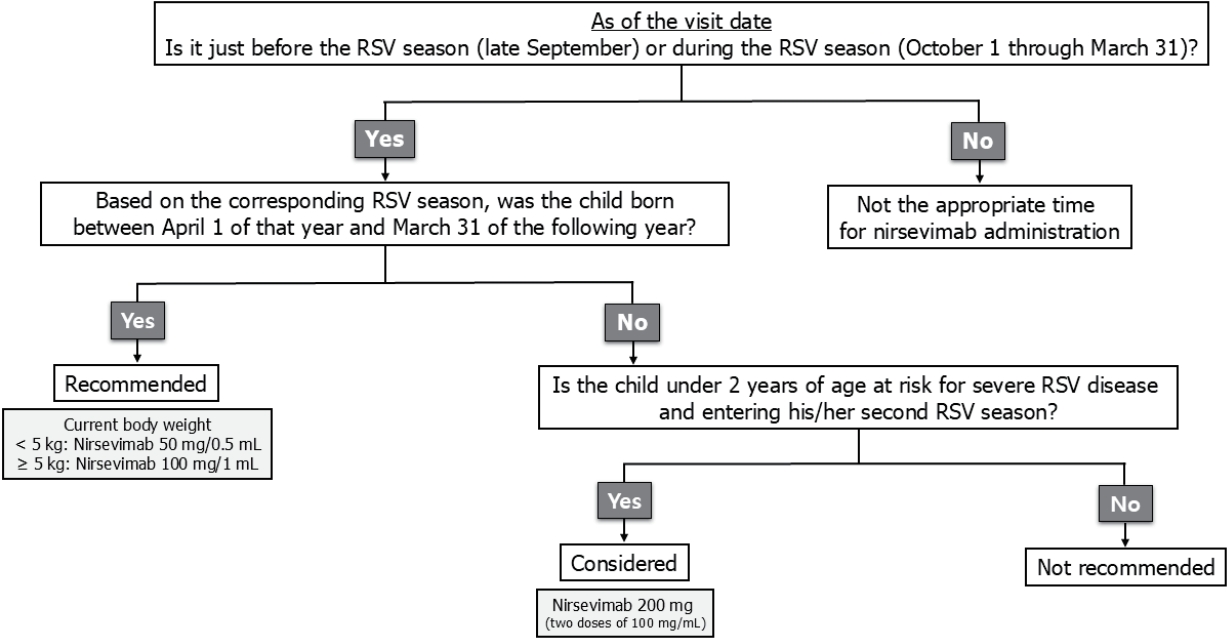
To prevent respiratory syncytial virus (RSV)-associated lower respiratory tract infections, a single dose of nirsevimab, a long-acting monoclonal antibody, is recommended for all neonates born during the RSV season (October to March) and all infants younger than 6 months old at the start of the RSV season. Nirsevimab should be administered shortly after birth to neonates and just before or early in the season to infants entering their first RSV season.
- Correspondence
- Infection
- A commentary on "COVID-19 vaccine hesitancy among parents of children with systemic lupus erythematosus"
- Hinpetch Daungsupawong, Viroj Wiwanitkit
- Clin Exp Pediatr. 2025;68(8):624-625. Published online April 16, 2025
-
- Original Article
- Infection
- Enteric pathogens implicated in acute infectious diarrhea among young children in resource-limited region with rapidly growing population: a hospital-based cross-sectional study
- Aseel Mahmood Ibrahim Al-Mashahedah, Randa Mohammed Dhahi
- Clin Exp Pediatr. 2025;68(5):379-387. Published online December 23, 2024
-

Question: What are the most common enteric pathogens in acute diarrhea among children younger than 5 years of age, and which age group is most susceptible?
Finding: Bacteria were the most common causative microorganisms of diarrhea, followed by viruses, parasites, and fungi. The 1–2-year age group was the most commonly affected.
Meaning: There is a need to formulate preventive strategies targeting children exposed to enteric pathogens to limit diarrhea.
- Clinical characteristics and associated factors of pediatric acute necrotizing encephalopathy: a retrospective study
- Huiling Zhang, Yilong Wang, Qianyun Ding, Xuekun Li, Sheng Ye
- Clin Exp Pediatr. 2025;68(2):153-162. Published online November 11, 2024
-
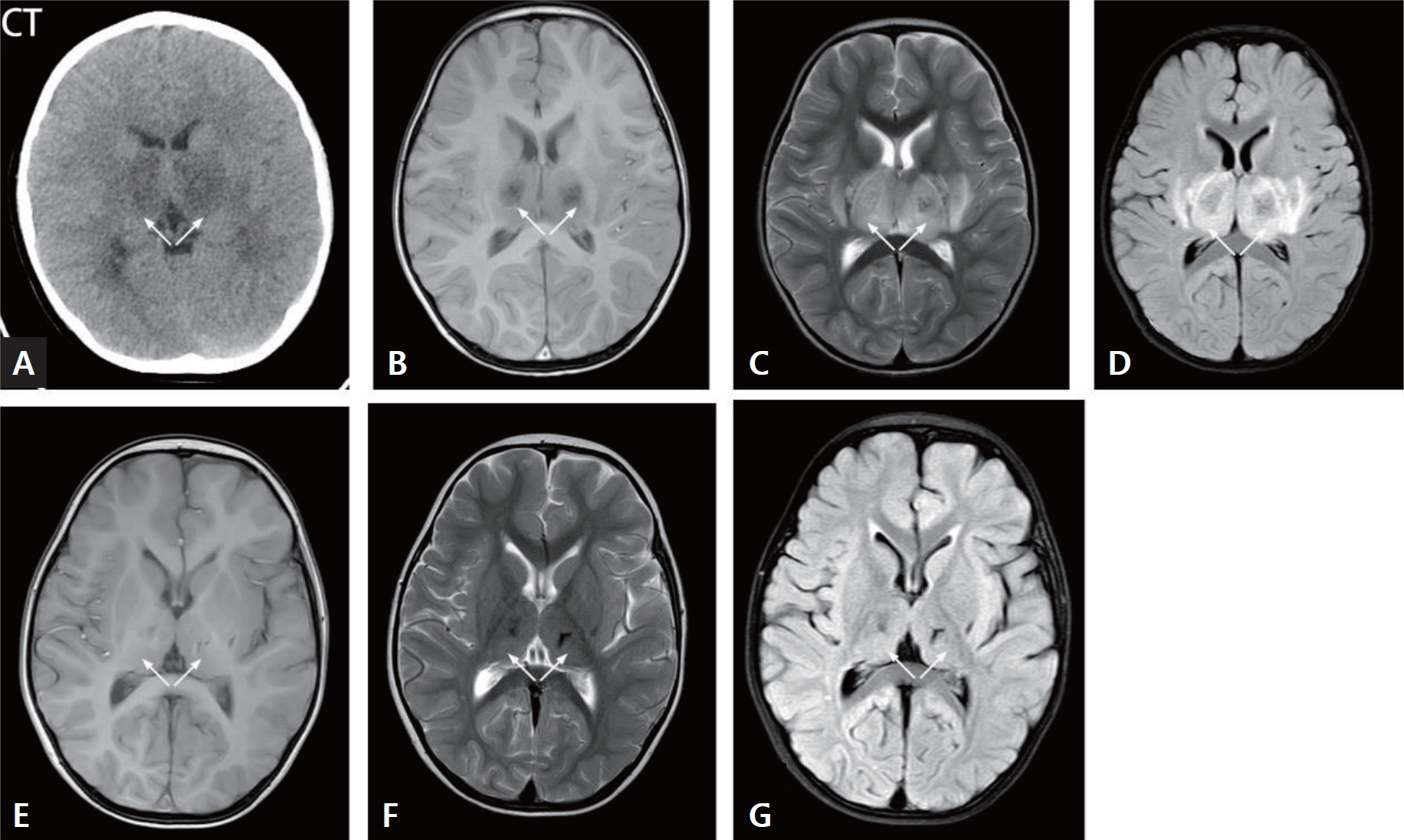
· The mortality rate of acute necrotizing encephalopathy was high.
· Laboratory tests revealed that the fatal group had higher creatinine, lactate, activated partial thromboplastin time, thrombin time, interleukin (IL)-6, IL-10, creatine kinase, and D-dimer than survivors.
· The fatal group displayed lower Glasgow Coma Scale scores and arterial pH.
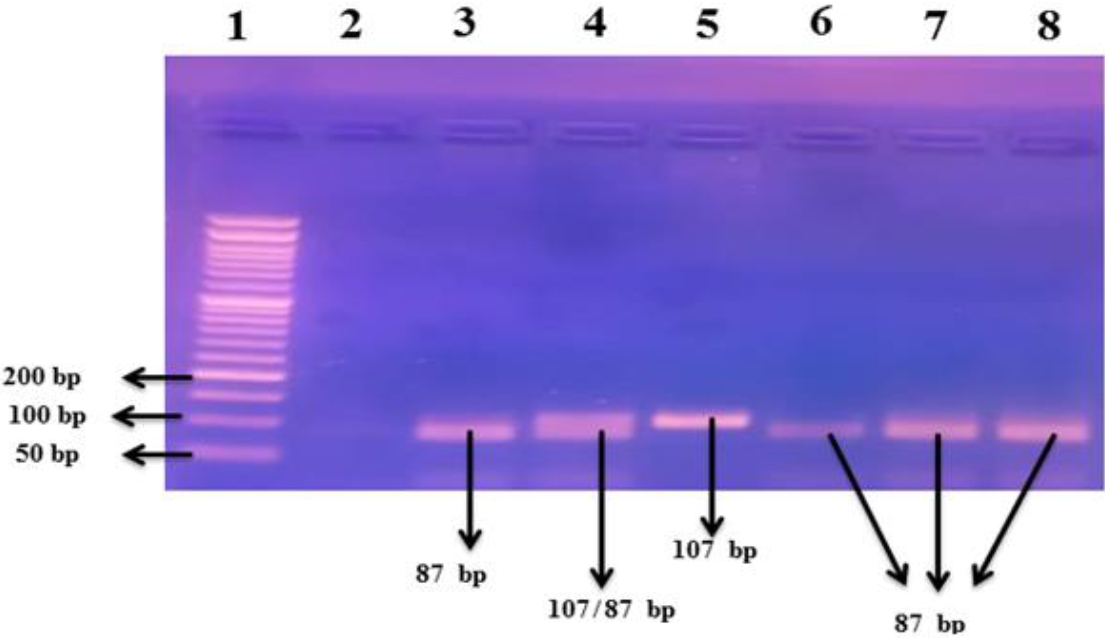
- Carbapenem resistance in gram-negative pathogens in an Iranian hospital: high prevalence of OXA-type carbapenemase genes
- Setareh Mamishi, Reihaneh Hosseinpour Sadeghi, Sadaf Sajedi Moghaddam, Babak Pourakbari, Shiva Poormohammadi, Maryam Sotoudeh Anvari, Shima Mahmoudi
- Clin Exp Pediatr. 2025;68(1):65-72. Published online October 31, 2024
-

Question: What is the prevalence of carbapenem resistance in gram-negative bacteria and associated carbapenemase genes?
Findings: This study identified a notable prevalence of carbapenem-resistant gram-negative isolates, with Escherichia coli being the predominant contributor, follow ed by Klebsiella pneumoniae, Acinetobacter baumannii, while bla OXA48 was the most prevalent carbapenemase gene.
Meaning: These findings highlight the urgent need for proactive measures including the rapid detection of carbapenemase- producing isolates and effective infection control.
- Clinical, biochemical, and genetic study of TACE/TNF-α/ACE signaling pathway in pediatric COVID-19 infection
- Ahmed El-Abd Ahmed, Sawsan M.A. Abuhamdah, Mohammed H. Hassan, Nagwan I. Rashwan, Eman A. Abd-Elmawgood, Haggagy Mansour, Hoda S. Sherkawy, Shymaa G. Rizk
- Clin Exp Pediatr. 2024;67(12):704-717. Published online November 27, 2024
-
Question: Is the tumor necrosis factor (TNF) signaling pathway (TNF-α-converting enzyme [TACE]/TNF-α/angiotensin converting enzyme [ACE]) involved in pediatric coronavirus disease 2019 (COVID-19) infection?
Finding: Significantly increased circulating TACE/TNF-α and decreased ACE2 levels were noted. TNF-α-308G/A plays a significant role in susceptibility to COVID-19 infection among children. The ACE (I/D) (rs4646994) and ACE2 (rs2285666) single nucleotide polymorphisms lack significant associations with pediatric COVID-19 infection.
Meaning: The TNF signaling pathway participates in pediatric COVID-19 infection.
- Editorial
- Infection
- Preventing bloodstream infections in children after liver transplantation
- Young June Choe
- Clin Exp Pediatr. 2024;67(11):599-600. Published online April 18, 2024
-
Liver transplantation (LT) is crucial for children with end-stage liver diseases, yet bloodstream infections (BSI) pose significant risks, despite medical advancements. Immunosuppressants, essential for preventing organ rejection, heighten infection susceptibility. Understanding BSI organisms is vital due to antimicrobial resistance. Pediatric LT recipients have unique risk factors, demanding tailored preventive measures. This systematic review on bacterial BSI emphasizes the urgency of effective prevention strategies, considering the high incidence and distinct organism profile. Further research is vital for optimizing antibiotic management and improving outcomes for this vulnerable population.
- Review Article
- Infection
- Incidence, causative organisms, and risk factors of bloodstream infections in pediatric liver transplant patients: a systematic review
- Mohamad Shieb, Rand Hasanain, Zara Arshad, Faisal A. Nawaz, Rahul Kashyap, Eric J. Stern
- Clin Exp Pediatr. 2024;67(9):427-434. Published online April 5, 2024
-

The overall incidence of bloodstream infections was 23.5%. Gram-negative organisms occur at a much higher rate in pediatric liver transplant recipients then that the general pediatric population. However, when comparing pediatric and adult liver transplant recipients Gram-positive organisms occur with a much higher rate in the pediatric population highlighting the importance of early and broad spectrum antimicrobial coverage when bloodstream infections are suspected.
- Original Article
- Infection
- Construction and validation of predictive models for intravenous immunoglobulin–resistant Kawasaki disease using an interpretable machine learning approach
- Linfan Deng, Jian Zhao, Ting Wang, Bin Liu, Jun Jiang, Peng Jia, Dong Liu, Gang Li
- Clin Exp Pediatr. 2024;67(8):405-414. Published online July 23, 2024
-

Question: Is there a reliable model to predict intravenous immunoglobulin (IVIG)-resistant Kawasaki disease (KD)?
Finding: We constructed 5 machine learning models to predict IVIG-resistant KD. Extreme gradient boosting (XGBoost) model was superior to logistic, support vector machine, light gradient boosting machine and multiple layers perception models. The SHAP (SHapley Additive exPlanations) value interpreted the contribution of each feature in XGBoost model.
Meaning: XGBoost model showed the excellent performance to predict IVIG-resistant KD with explainable and visualizable machine learning algorithm.
- Review Article
- Infection
- Community-acquired pneumonia in children: updated perspectives on its etiology, diagnosis, and treatment
- Ki Wook Yun
- Clin Exp Pediatr. 2024;67(2):80-89. Published online June 14, 2023
-
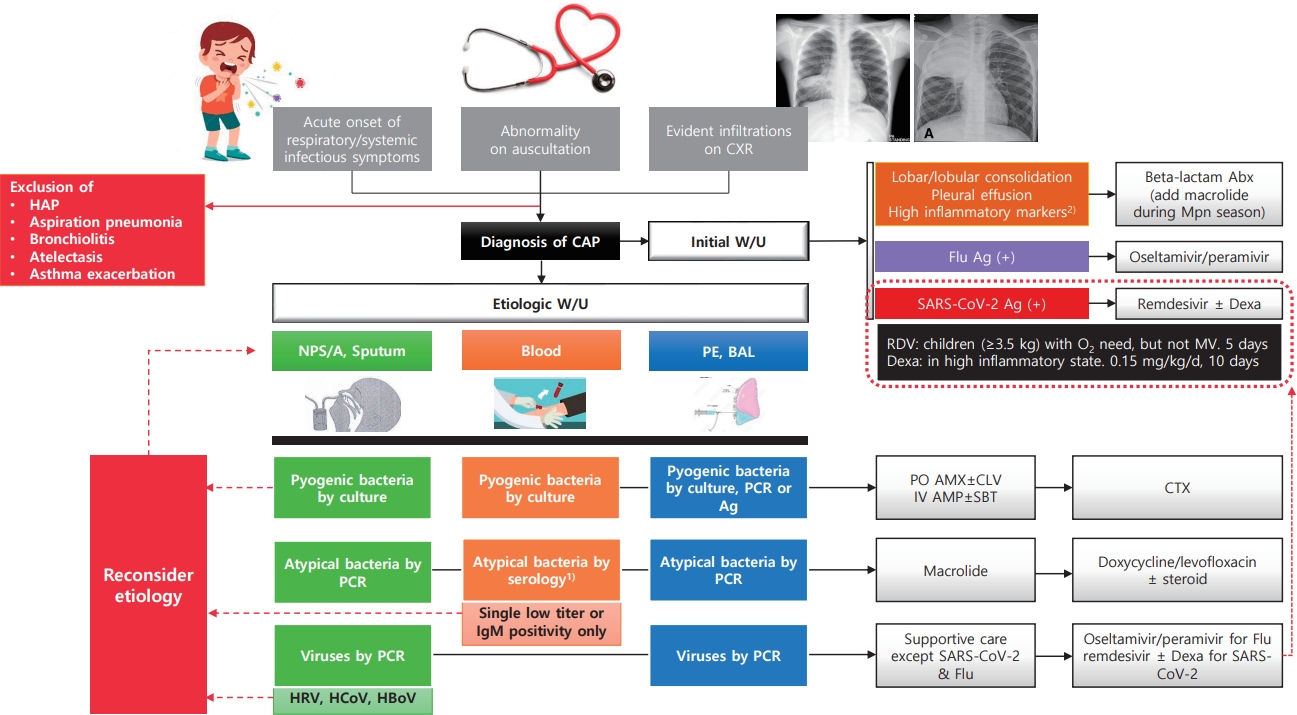
· Most commonly confirmed causes of community-acquired pneumonia (CAP) in children are Mycoplasma pneumoniae (8%–40%) and respiratory syncytial virus (15%–20%).
· Pyogenic bacteria, most commonly Streptococcus pneumoniae (40%–50%) and Streptococcus pyogenes (10%–25%), are detected in 2%–5% of children hospitalized with CAP.
· CAP should be diagnosed conservatively according to clinical and radiological criteria.
· The etiology should be identified via appropriate test result interpretation.
- COVID-19 among infants: key clinical features and remaining controversies
- Nevio Cimolai
- Clin Exp Pediatr. 2024;67(1):1-16. Published online November 27, 2023
-
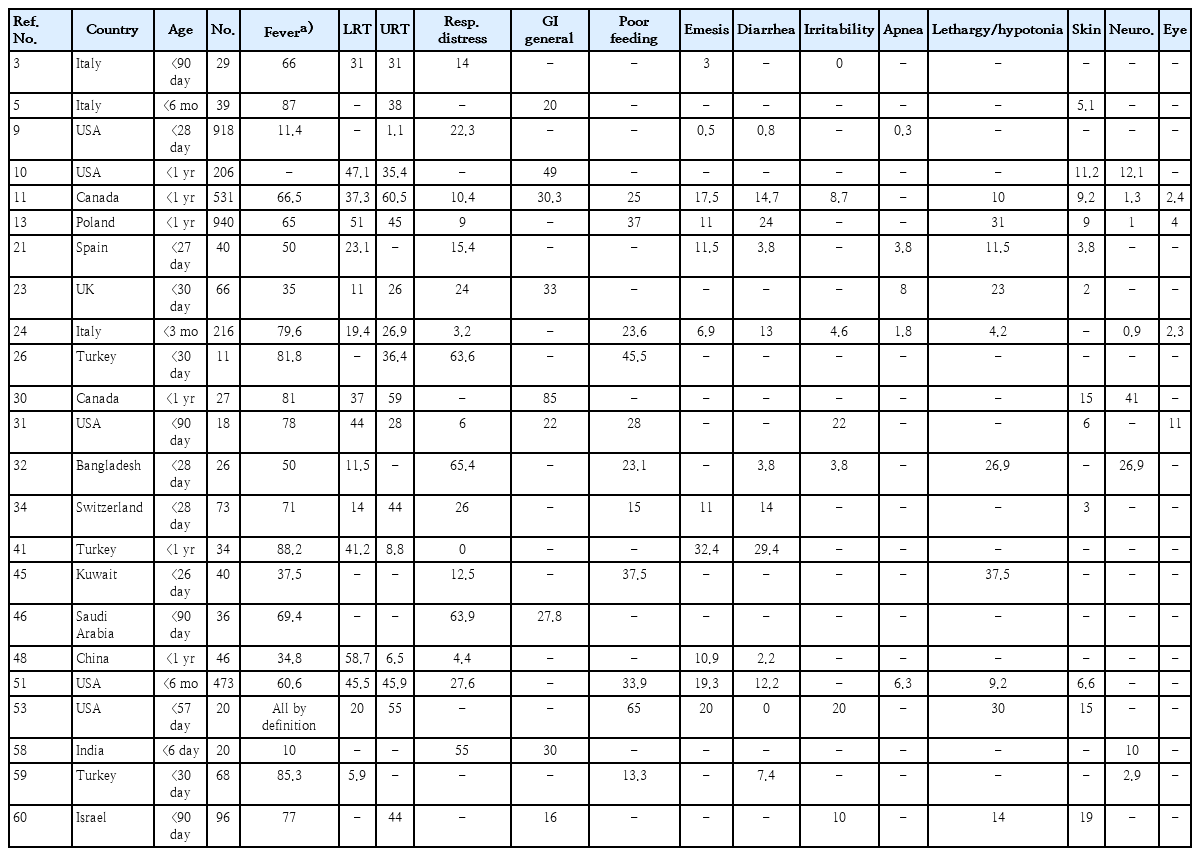
· Clinical studies of coronavirus disease 2019 (COVID-19) in infants should be supported by rigorous laboratory diagnostic criteria.
· Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spreads to infants similarly to other viral respiratory infections.
· Among infants ≤1 year of age beyond the immediate postpartum period, COVID-19 is relatively mild, but even the low risk of severe disease requires prevention.
· Comorbidities increase infection vulnerability and complications in infants.
· Clinical and laboratory data do not sufficiently distinguish COVID-19 from other respiratory viral infections.
· Coinfection with SARS-CoV-2 is uncommon among infants.
· Unique infection sequelae, including multi-inflammatory syndrome in children and neonates and long COVID require further study and refinement of diagnostic criteria.
· Infection control standards applied to mother-infant dyads should be tempered by standard preventive strategies, maternal input, accommodation potential, and overall safety.
· Maternal vaccination prevents disease in early infancy.
- Editorial
- Infection
- COVID-19 infection and vaccination among children
- Amnuay Kleebayoon, Viroj Wiwanitkit
- Clin Exp Pediatr. 2023;66(12):531-532. Published online August 30, 2023
-
· Coronavirus disease 2019 (OVID-19) infection and immunization have been linked with kidney problems; however, causality has not been proven.
· Concern about confounders is usually needed.
· Correspondence about a published article on the COVID-19 vaccine
- Review Article
- Infection
- Safety monitoring of COVID-19 vaccines: February 26, 2021, To June 4, 2022, Republic of Korea
- Yeon-Kyeng Lee, Yunhyung Kwon, Yesul Heo, Eun Kyoung Kim, Seung Yun Kim, Hoon Cho, Seontae Kim, Mijeong Ko, Dosang Lim, Soon-Young Seo, Enhi Cho
- Clin Exp Pediatr. 2023;66(10):415-423. Published online June 13, 2023
-
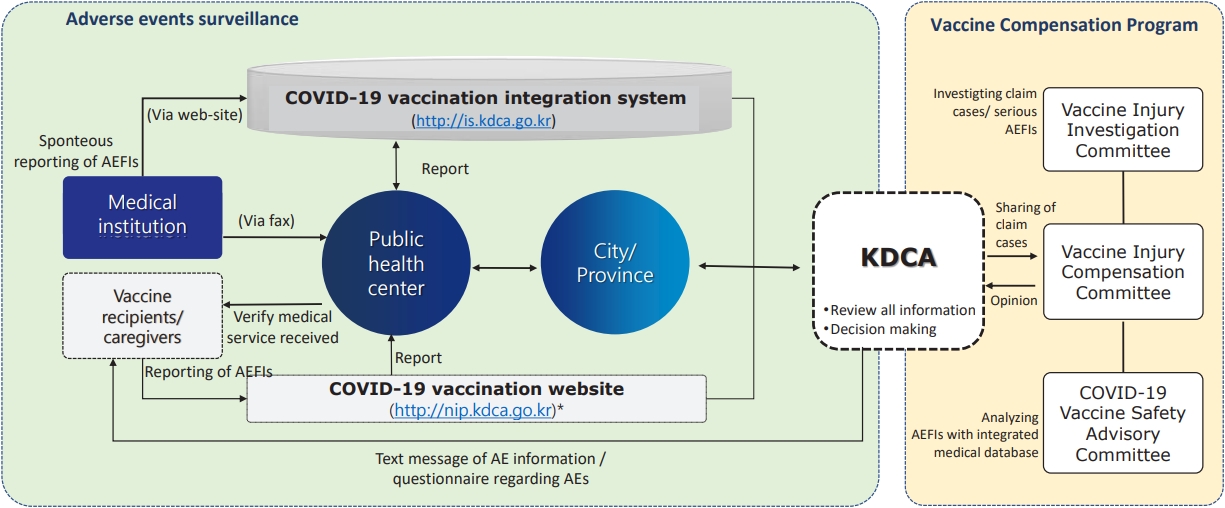
· Enhanced safety monitoring system of coronavirus disease 2019 (COVID-19) vaccines were implemented to detect signals rapidly as part of the national COVID-19 vaccination program.
· As of June 4, 2023, reported adverse events after COVID-19 vaccination was 0.38% among 125,107,883 doses of COVID- 19 vaccines administered.
· Most reported adverse reactions after COVID-19 vaccinations have shown nonserious and mild intensity.
- Letter to the Editor
- Infection
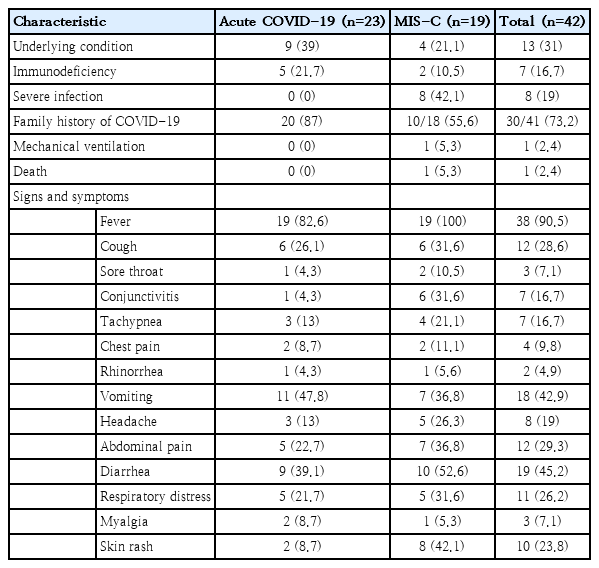
- SARS-CoV-2 fecal shedding pattern in pediatric patients with acute COVID-19 or COVID-19-associated multisystem inflammatory syndrome
- Setareh Mamishi, Fatemeh Jalali, Sepideh Benvari, Babak Pourakbari, Mohammad Reza Abdolsalehi, Reihaneh Hosseinpour Sadeghi, Mohammad Shahbabaie, Amene Navaeian, Shima Mahmoudi
- Clin Exp Pediatr. 2023;66(8):366-368. Published online June 14, 2023
-
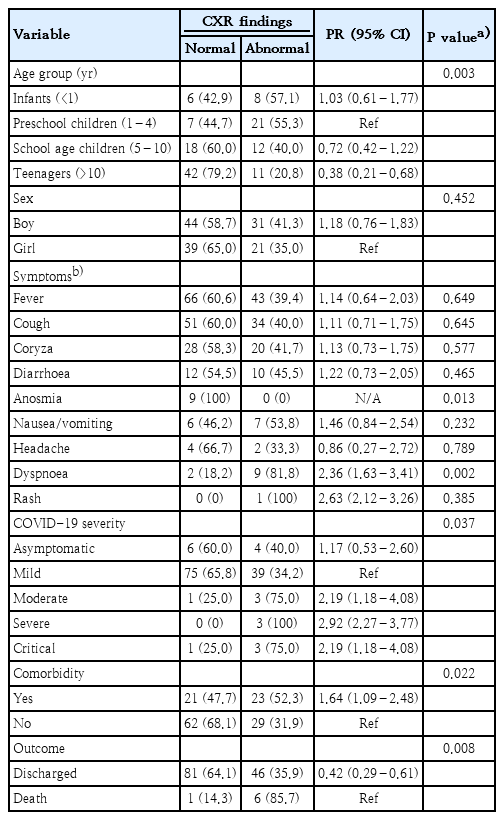
- Chest x-ray findings in children with COVID-19: lesson learned from referral hospitals in Medan, North Sumatera, Indonesia
- Andrew Limavady, Eka Airlangga, Ririe Fachrina Malisie, Ayodhia Pitaloka Pasaribu
- Clin Exp Pediatr. 2023;66(7):317-319. Published online May 16, 2023
-
- Original Article
- Infection
- Seroprevalence of maternal peripartum human T-cell lymphotropic virus type-1 infection: a systematic review and meta-analysis of the Nigerian literature
- Abdulrasheed Usman, Muhammad Hamis Musa, Bukhari Isah Shuaib, Olayemi Balogun, Mukhtar Adeiza
- Clin Exp Pediatr. 2023;66(7):307-316. Published online December 22, 2022
-
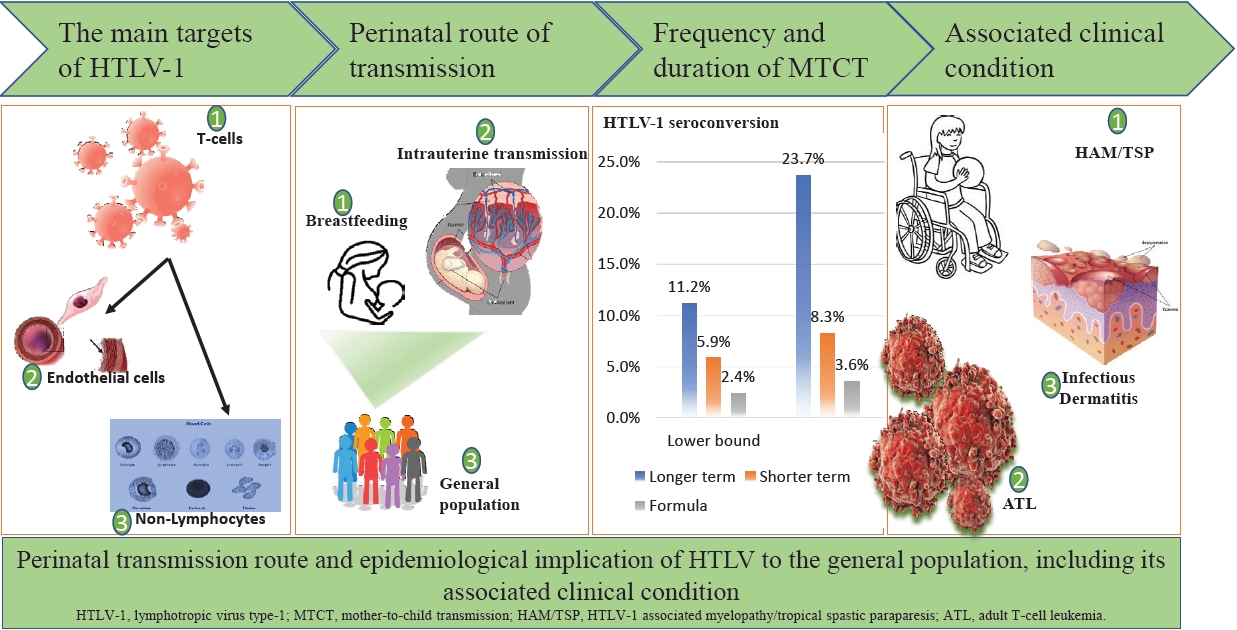
The peripartum period is an important transmission time for human T-cell lymphotropic virus-1 (HTLV-1) infection, mainly via breastfeeding and partly through the placental tissues of carrier mothers. Although most HTLV-1–infected individuals are asymptomatic, fetal and childhood infections often result in several diseases with disappointing treatment outcomes. An estimated HTLV-1 burden in Nigeria among perinatal women must be determined to enable rational planning of a comprehensive health care intervention.
- Editorial
- Infection
- Impact and role of vitamins as immunonutrition in children during COVID-19 pandemic
- Yoo Min Lee
- Clin Exp Pediatr. 2023;66(5):212-214. Published online April 18, 2023
-

· Vitamins have effector mechanisms in the innate and adaptive immune systems and potential roles in preventing and reducing the severity of coronavirus disease 2019 (COVID-19).
· Vitamins may be immunonutrients in the treatment of COVID-19 infections and prevention of patient deterioration due to critical illness, thus demonstrating the significance of a nutritious, well-balanced diet.
- Review Article
- Infection
- COVID-19 in immunocompromised children and adolescents
- Byung Ok Kwak, Byung Wook Eun
- Clin Exp Pediatr. 2023;66(5):182-189. Published online April 18, 2023
-

Most immunocompromised children and adolescents are not at increased risk of developing severe coronavirus disease 2019 (COVID-19). COVID-19 outcomes for low- or medium-risk immunocompromised children are favorable, while more serious illness reportedly occurs in high-risk immunocompromised children by underlying disease, its treatments, and other factors. Therefore, the early detection and timely management of severe COVID-19 and treatment of underlying disease are important. Hospitalization and COVID-19 vaccination should be carefully considered.
- Original Article
- Infection
- Predicting COVID-19 transmission in a student population in Seoul, South Korea, 2020–2021
- Young Hwa Lee, Han Ho Kim, Young June Choe
- Clin Exp Pediatr. 2023;66(4):173-178. Published online December 22, 2022
-
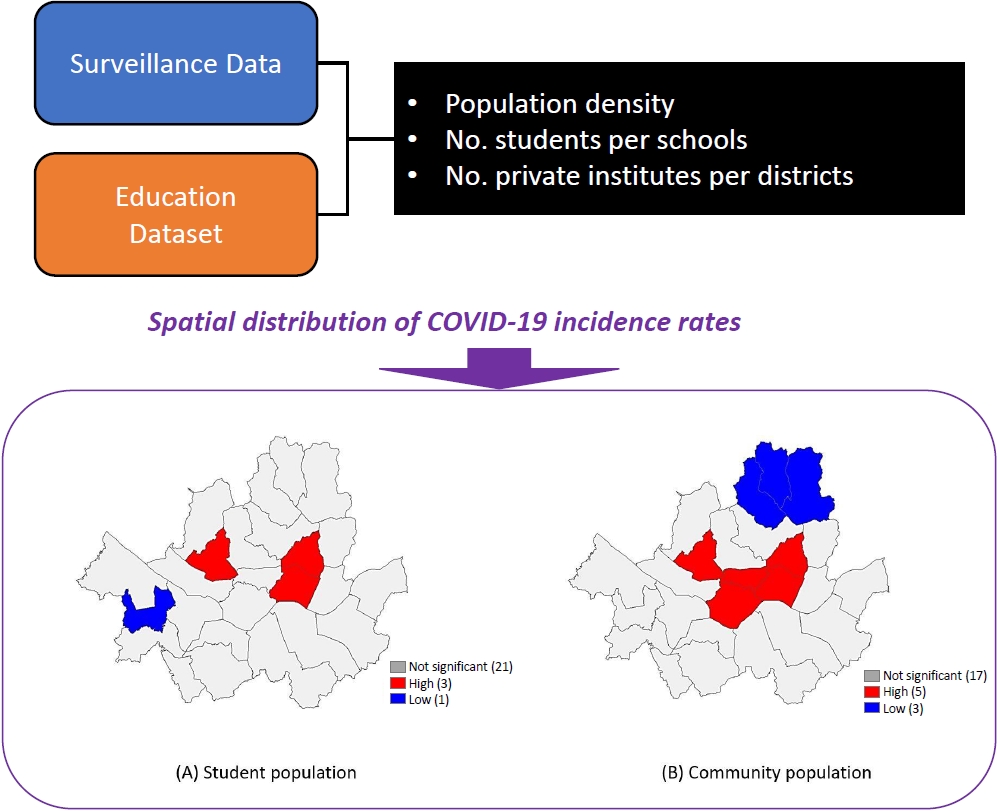
Question: What is the spatial distribution and determinants of coronavirus disease 2019 (COVID-19) infection among students in Korea?
Finding: The community population was closely associated with the risk of COVID-19, and the number of students per school class were inversely associated with COVID-19 rates in students.
Meaning: Our finding suggests that controlling the community-level burden of COVID-19 can help prevent sudden acute respiratory syndrome coronavirus 2 infection in school-aged children.
- Clinical characteristics of pediatric patients infected with SARS-CoV-2 versus common human coronaviruses: a national multicenter study
- In Suk Sol, Eun Lee, Hyeon-Jong Yang, Yong Ju Lee, Hye Yung Yum, Mi-Hee Lee, Mi Ae Chu, Hui Jeong Moon, Hyo-Bin Kim, Ju Hee Seo, Jung Yeon Shim, Ji Young Ahn, Yoon Young Jang, Hai Lee Chung, Eun Hee Chung, Kyunghoon Kim, Bong-Seong Kim, Cheol Hong Kim, Yang Park, Meeyong Shin, Kyung Suk Lee, Man Yong Han, Soo-Jong Hong, Eun Kyeong Kang, Chang Keun Kim; on behalf of The Pneumonia & Respiratory Disease Study Group of Korean Academy of Pediatric Allergy and Respiratory Disease
- Clin Exp Pediatr. 2023;66(3):134-141. Published online December 22, 2022
-

Question: The clinical differences between severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and human coronaviruses (HCoV) in children remain unknown.
Finding: This study compared the clinical findings of children infected with SARS-CoV-2 versus HCoV. Its findings suggest that children and adolescents with SARS-CoV-2 have a milder clinical course than those with HCoV.
Meaning: The clinical course of children and adolescents with SARS-CoV-2 should be closely monitored during the coronavirus disease 2019 pandemic.
- Review Article
- Infection
- Pathogenetic and etiologic considerations of febrile seizures
- Ji Yoon Han, Seung Beom Han
- Clin Exp Pediatr. 2023;66(2):46-53. Published online January 13, 2023
-

· Inflammatory responses accompanying fever increase neuronal excitability in the central nervous system, which in turn provokes seizures.
· Fever in children with febrile seizures is usually caused by common respiratory viruses, the distributions of which match those of seasonal community-acquired respiratory tract infections.
· Several genetic variations in ion channels seem associated with neuronal hyperexcitability in children with febrile seizures.
- Global varicella vaccination programs
- Young Hwa Lee, Young June Choe, Jia Lee, Eunseong Kim, Jae Young Lee, Kwan Hong, Yoonsun Yoon, Yun-Kyung Kim
- Clin Exp Pediatr. 2022;65(12):555-562. Published online November 2, 2022
-

It is important to evaluate its effectiveness at the national level and to determine the varicella vaccine schedule based on the evidence generated through the studies.
- Perspective
- Infection
- Statement on healthcare system preparedness in response to COVID-19 Omicron subvariants BA.4 and BA.5 surge in Korea from the Korean Pediatric Society and Korean Society of Pediatric Infectious Diseases
- Eun Young Cho, Dong Hyun Kim, Soo-Han Choi, Ki Wook Yun, Jong Gyun Ahn, Hye-Kyung Cho, Hyunju Lee, Jina Lee, Taek-Jin Lee, Byung-Wook Eun, Jin Lee, Dae Sun Jo, Yun-Kyung Kim, Yae-Jean Kim; Committee on Infectious Diseases of the Korean Pediatric Society
- Clin Exp Pediatr. 2022;65(11):510-511. Published online September 23, 2022
-
In order to respond to the recent surge in coronavirus disease 2019 (COVID-19) cases and the continuously changing epidemiology of COVID-19, a sustainable and flexible pediatric healthcare system must be prepared considering the specificity of pediatric care. We demand a more proactive response from the health authorities to check the current state of pediatric COVID-19 patient care and to ensure that pediatric patients receive appropriate and timely management.
-

-
-
6.02024CiteScore98th percentilePowered by
-
Impact Factor3.6
-
- TOPICS
- ARTICLE CATEGORY
- Editorial Office
-
Korean Pediatric Society
#1606 Seocho World Officetel, 19 Seoun-ro, Seocho-ku, Seoul 06732, Korea
Tel: +82-2-3473-7306 Fax: +82-2-3473-7307 E-mail: office@e-cep.org
Clinical and Experimental Pediatrics is an open access journal. All articles are distributed under the terms of the Creative Commons Attribution NonCommercial License (http://creativecommons.org/licenses/by-nc/4.0/)
Copyright © 2026 by Korean Pediatric Society.