1. Halstead SB, Hills SL, Dubischar K. Japanese encephalitis vaccines. In: Plotkin SA, Orentein WA, Offit PA, Edwards KM, editors. Plotkin’s vaccines. 7th ed. Philadelphia (PA): Elsevier, 2018:511–48.
2. Solomon T. Control of Japanese encephalitis-within our grasp? N Engl J Med 2006;355:869–71.


5. Sabin AB, Schlesinger RW. Japanese B encephalitis in American soldiers in Korea. Am J Hyg 1947;46:356–75.

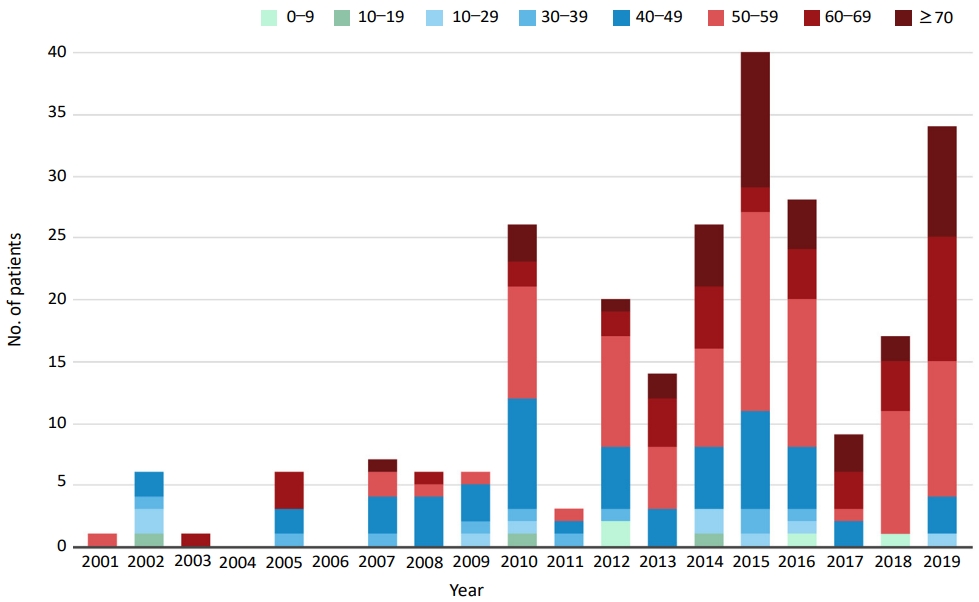
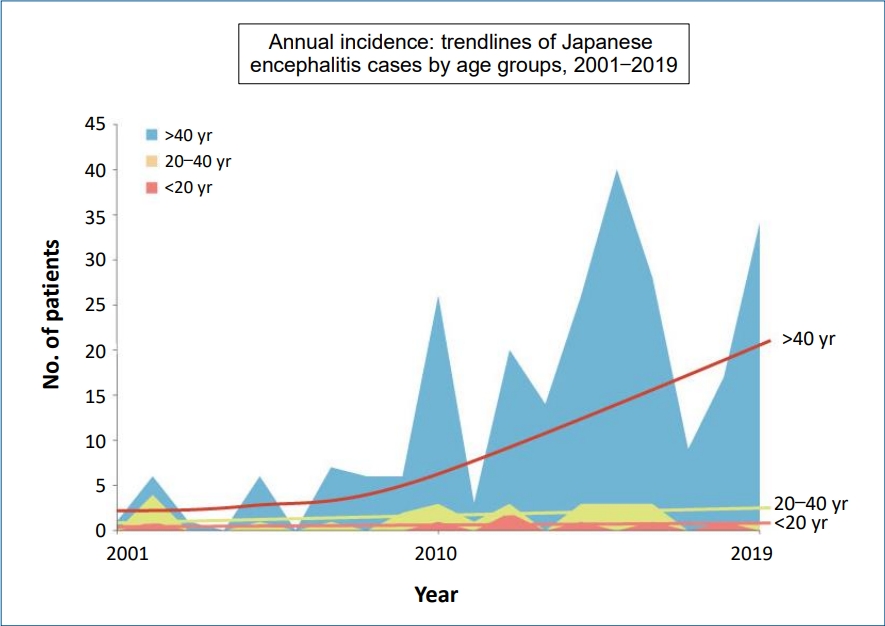
7. Lee DW, Choe YJ, Kim JH, Song MK, Cho H, Bae GR, et al. Epidemiology of Japanese encephalitis in South Korea, 2007–2010. Int J Infect Dis 2012;16:448–52.

9. Simon-Loriere E, Faye O, Prot M, Casademont I, Fall G, Fernandez-Garcia MD, et al. Autochthonous Japanese encephalitis with yellow fever coinfection in Africa. N Engl J Med 2017;376:1483–5.


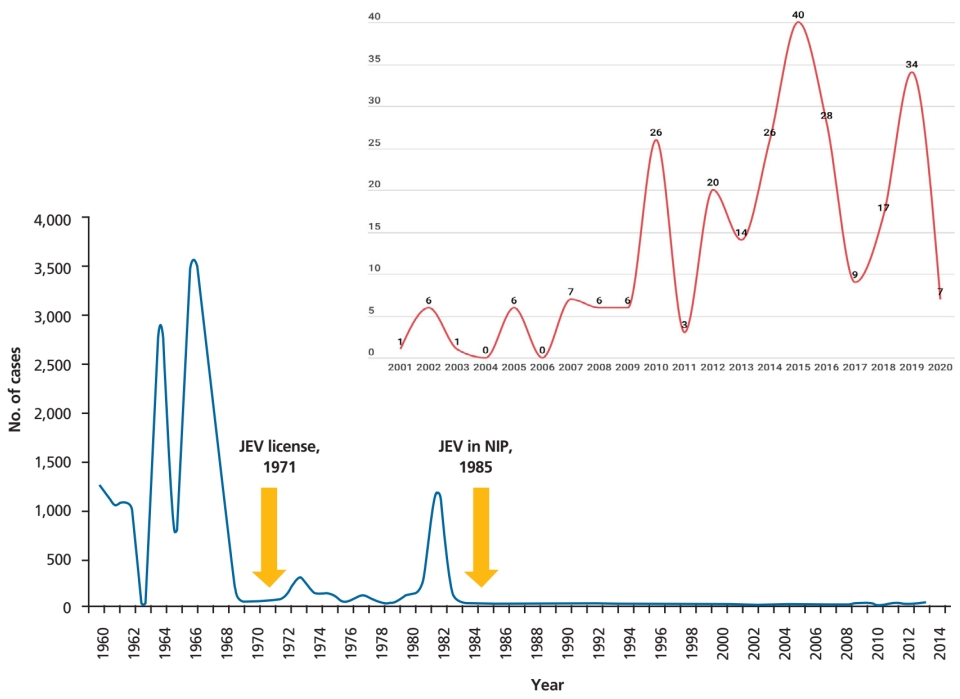
11. Arai S, Matsunaga Y, Takasaki T, Tanaka-Taya K, Taniguchi K, Okabe N, et al. Vaccine preventable diseases surveillance program of Japan. Japanese encephalitis: surveillance and elimination effort in Japan from 1982 to 2004. Jpn J Infect Dis 2008;61:333–8.


13. Tseng HF, Tan HF, Chang CK, Huang WL, Ho WC. Seroepidemiology study of Japanese encephalitis neutralizing antibodies in southern Taiwan: a comparative study between urban city and country townships. Am J Infect Control 2003;31:435–40.


14. Korea Centers for Disease Control and Prevention. Infectious diseases surveillance yearbook 2019. Cheongju (Korea): Korea Centers for Disease Control and Prevention, 2020.
15. Yun KW, Lee HJ, Park JY, Cho HK, Kim YJ, Kim KH, et al. Long-term immunogenicity of an initial booster dose of an inactivated, Vero cell culture-derived Japanese encephalitis vaccine (JE-VC) and the safety and immunogenicity of a second JE-VC booster dose in children previously vaccinated with an inactivated, mouse brain-derived Japanese encephalitis vaccine. Vaccine 2018;36:1398–404.


16. The Korean Pediatric Society. Japanese encephalitis vaccines. In: Kim JH, editor. Immunization guideline. 9th ed. Seoul (Korea): The Korean Pediatric Society, 2018:186–202.
17. Cha SH. The history of vaccination and current vaccination policies in Korea. Clin Exp Vaccin Res 2012;1:3–8.

18. Choe YJ, Taurel AF, Nealon J, Seo HS, Kim HS. Systematic review of seroepidemiological studies on Japanese encephalitis in the Republic of Korea. Int J Infect Dis 2018;67:14–9.


20. Deuel RE Jr, Barwell MB, Matumoto M, Sabain AB. Status and significance of inapparent infection with virus of Japanese B encephalitis in Korean and Okinawa in 1946. Am J Hyg 1950;51:13–20.


21. Kim KH. Recent epidemiological features of Japanese encephalitis in the Republic of Korea. Korean J Infect Dis 1974;6:83–8.
22. Kim SO, Lee YJ, Jung BK, Lee HW. The distribution of hemagglutination inhibition antibody for Japanese encephalitis in residents of Seoul areas. Choeshin Ui-hak 1976;19:21–6.
23. Lee YT, Lee CH. Serological study on Japanese encephalitis in Koreans and fowls, 1975. Korean J Infect Dis 1976;8:75–82.
24. Lee YT, Lee CH. The distribution of hemagglutination inhibition antibodies for Japanese encephalitis virus against the Koreas 1976. J Korean Soc Microbiol 1977;12:51–6.
25. Lee CH, Ko KK. The distribution of hemagglutination inhibition antibodies for Japanese encephalitis virus in Korea (1977, 1978). Choeshin Ui-hak 1979;113–9.
26. Lee CH, Lee YT, Ko KJ, Moon KS, Kim OJ. The distribution of hemagglutination inhibition antibodies for Japanese encephalitis virus in Koreans 1979. Korean J Virol 1980;10:65–9.
27. Lee YT, Youm BJ. A hemagglutination inhibition antibody test for Japanese encephalitis virus among the Koreans, 1984-1985. Korean J Virol 1985;15:1–9.
28. Abe M, Okada K, Hayashida K, Matsuo F, Shiosaki K, Miyazaki C, et al. Duration of neutralizing antibody titer after Japanese encephalitis vaccination. Microbiol Immunol 2007;51:609–16.


30. Kwak BO, Kwon YS, Hong YJ, Shin SH, Eun BW, Ahn YM, et al. Immunogenicity and safety of the third booster dose of the inactivated Japanese encephalitis vaccine in Korean. Vaccine 2021;39:1929–32.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


