Topics
- Page Path
-
- HOME
- TOPICS
- Topics
- Topics
-
- Adolescence Medicine (4)
- Allergy (64)
- Cardiology (81)
- Critical Care Medicine (15)
- Developmental and Behavioral Medicine (24)
- Emergency Medicine (5)
- Endocrinology (65)
- Gastroenterology (76)
- General Pediatrics (58)
- Genetics and Metabolism (26)
- Hematology (20)
- Immunology (16)
- Infection (82)
- Neonatology (Perinatology) (127)
- Nephrology (Genitourinary) (54)
- Neurology (96)
- Nutrition (33)
- Oncology (19)
- Neurobehavior (12)
- Pulmonology (35)
- Rheumatology (4)
- Other (44)
- Guideline
- Infection
- Recommendation for use of 15- and 20-valent pneumococcal conjugate vaccines in Korean infants and children
- Ki Wook Yun, Dong Hyun Kim, Jong Gyun Ahn, Byung-Wook Eun, Jin Lee, Jina Lee, Taek-Jin Lee, Hyunju Lee, Dae Sun Jo, Eun Young Cho, Hye-Kyung Cho, Soo-Han Choi, Young June Choe, Ui Yoon Choi, Yun-Kyung Kim; The Committee on Infectious Diseases of the Korean Pediatric Society
- Clin Exp Pediatr. 2026;69(1):76-83. Published online December 30, 2025
-
Compared to PCV13, PCV15 includes 2 (22F and 33F), and PCV20 includes 7 (8, 10A, 11A, 12F, 15B, 22F, and 33F) additional serotypes. The vaccination schedule remains the same: primary doses at 2, 4, and 6 months, and a booster at 12–15 months. If PCV13 was administered in the primary series, PCV15 and PCV20 may be used to complete it or as a booster.
- Clinical Note
- Neonatology (Perinatology)
- External tracheal compression and mucosal injury in a neonate with cervical teratoma: a rare airway challenge
- Rhodora Guillen, Arijit Lodha, Prashanth Murthy
- Clin Exp Pediatr. 2026;69(1):73-75. Published online December 4, 2025
-

- Original Article
- Other
- Comparing ethyl chloride and 10% lignocaine spray for pediatric intravenous cannulation pain relief
- Susmitha Vellanki, Malavika Kulkarni, H.D. Arun Kumar, Deepali Shetty, Nikhil Karthik B, Mathew Tom
- Clin Exp Pediatr. 2026;69(1):65-72. Published online November 21, 2025
-

Background: Intravenous cannulation (IVC) is a routine yet distressing procedure in pediatric patients, often provoking significant anxiety and procedural pain. Although eutectic mixtures such as eutectic mixture of local anesthetic cream are widely used, their delayed onset limits their applicability in time-sensitive settings. Ethyl chloride vapocoolant spray and 10% lignocaine spray have been proposed as rapid-onset alternatives, yet direct comparative...
- Critical Care Medicine
- High-dose methylprednisolone and tocilizumab improve survival of patients with high-risk pediatric acute necrotizing encephalopathy
- Chaonan Fan, Fei Li, Kechun Li, Zheng Li, Yiyang Mao, Lijuan Wang, Gang Liu, Yingchao Liu, Quan Wang, Suyun Qian
- Clin Exp Pediatr. 2026;69(1):56-64. Published online October 22, 2025
-

Question: Which immunomodulatory strategies can reduce mortality in children with acute necrotizing encephalopathy (ANE)?
Finding: High-dose methylprednisolone (30 mg/kg/day) significantly improved the survival of high-risk patients, particularly when combined with tocilizumab.
Meaning: These findings support the use of a severity-based immunotherapy approach to optimize the outcomes of pediatric ANE.
- Rheumatology
- Recurrent immunoglobulin A vasculitis in children and adolescents: prevalence and associated risk factors
- Nootsara Atchariyaphuk, Maynart Sukharomana, Thanaporn Chaiyapak, Sirirat Charuvanij
- Clin Exp Pediatr. 2026;69(1):46-55. Published online October 22, 2025
-

Question: What can predict immunoglobulin A vasculitis (IgAV) recurrence, and when does it occur? How do childhood- and adolescent-onset IgAV compare?
Finding: The IgAV recurrence rate was 35.6%. It usually occurred within 12 months and was associated with corticosteroids treatment.
Meaning: Childhood-onset IgAV more commonly featured gastrointestinal and musculoskeletal manifestations and required hospitalization. Adolescent-onset IgAV more commonly featured renal involvement. Vigilant monitoring for recurrence is necessary, particularly with corticosteroids treatment.
- Allergy
- Maternal sleep disorders during pregnancy and subsequent risk of allergic diseases in Japanese children: the TMM BirThree Cohort Study
- Ami Uematsu, Masatsugu Orui, Mami Ishikuro, Keiko Murakami, Aoi Noda, Genki Shinoda, Taku Obara, Shinichi Kuriyama
- Clin Exp Pediatr. 2026;69(1):36-45. Published online October 22, 2025
-

Question: Associations have been made between maternal sleep disorders during pregnancy and allergic diseases including bronchial asthma, atopic dermatitis, food allergy, and allergic conjunctivitis/rhinitis/hay fever in their children.
Finding: In the crude model, sleep disorders during pregnancy were associated with all examined allergic diseases in children. After adjustment, significant associations remained for atopic dermatitis and allergic conjunctivitis/rhinitis/hay fever.
Meaning: The study highlights associations between maternal sleep and child allergic diseases.
- Gastroenterology
- Gut microbiota and metabolomic alterations in newborns of mothers with gestational diabetes mellitus
- Wan-Hsin Su, Yi-Wei Wang, Chien-Chang Chen, Ming-Wei Lai, Hsun-Chin Chao, Ming-Chou Chiang, Ren-Huei Fu, Pai-Jui Yeh
- Clin Exp Pediatr. 2026;69(1):26-35. Published online October 22, 2025
-

Question: Does maternal gestational diabetes mellitus (GDM) affect newborn gut microbiota and metabolomic profiles?
Finding: Neonates born to mothers with diet-controlled GDM exhibited reduced gut microbiota α-diversity, altered β-diversity, and metabolic shifts, including changes in fumarate and succinate levels, with peroxisome proliferator-activated receptor and adipocytokine signaling pathway activation.
Meaning: Maternal GDM affects early microbial colonization and metabolism in newborns and may have long-term health implications.
- Editorial
- Allergy
- Prioritizing maternal sleep: a public health strategy for preventing childhood allergic diseases
- Eunchae Lee, Seohyun Hong, Dong Keon Yon
- Clin Exp Pediatr. 2026;69(1):22-25. Published online December 18, 2025
-

Sleep disorders affect more than half of pregnancies worldwide and can harm maternal health and offspring outcomes. Prioritizing maternal sleep as a public health strategy may help prevent prenatal and pediatric allergic diseases and reduce their burden. Other maternal health strategies may also reduce the burden of offspring allergic diseases, while adequate maternal sleep is associated with other offspring outcomes, underscoring its importance as a key public health strategy.
- Review Article
- Gastroenterology
- Ingestion of foreign bodies and caustic substances in children: a narrative review on clinical evaluation and management update
- Maria Rogalidou
- Clin Exp Pediatr. 2026;69(1):11-21. Published online December 10, 2025
-

Foreign body and caustic substance ingestion in children aged 1–5 years can feature to severe and, sometimes life-threatening complications. High-risk items include batteries, magnets, and corrosive chemicals. Severity depends on object type, location, and ingestion timing. Prompt diagnosis and early endoscopic intervention are crucial. Individualized management, high clinical suspicion, and parental education are essential to improving outcomes and preventing immediate and long-term complications affecting a child’s quality of life.
- Endocrinology
- Pubertal induction in prepubertal males with hypogonadotropic hypogonadism: testosterone or gonadotropins?
- Paolo Cavarzere, Riccardo Battiston, Valentina Lupieri, Valentina Mancioppi, Claudio Maffeis
- Clin Exp Pediatr. 2026;69(1):1-10. Published online December 18, 2025
-

The pubertal induction process in males still poses a challenge for pediatric endocrinologists. The existing literature is limited, and it is not yet possible to make definitive recommendations. We described the various treatment for this condition and tried to analyze the unresolved questions to address the question posed in the title of our manuscript.
- Clinical Note
- Gastroenterology
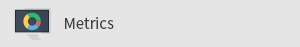
- Successful rescue after catastrophic bleeding of carotid artery pseudoaneurysm following button battery ingestion in a toddler
- Manjit Kaur, Ujjal Poddar, Basant Kumar, Abdul Muzil Munshi, Rajanikant R. Yadav, Moinak Sen Sarma, Anshu Srivastava
- Clin Exp Pediatr. 2025;68(12):1041-1044. Published online October 22, 2025
-
Button battery (BB) ingestion is an increasing hazard. Catastrophic gastrointestinal bleeding due to pseudoaneurysm rupture following BB impaction is often fatal. Here we report the case of an unwitnessed BB ingestion in an 18-month-old boy who presented with repeated massive UGIB due to a left CCA pseudoaneurysm that was successfully managed multidisciplinarily. BB ingestion should be considered in toddlers presenting with hematemesis.
- Original Article
- General Pediatrics
- Lipoprotein(a) prevalence trends in Portuguese children and adolescents: a real-world perspective
- Isabel Morais Ribeiro, Susete Vieira, Miguel Saraiva, Mónica Tavares, José Carlos Oliveira, Isabel Mangas Palma, Helena Ferreira Mansilha
- Clin Exp Pediatr. 2025;68(12):1031-1040. Published online November 24, 2025
-

Early lipid screening, including lipoprotein(a) (Lp(a)), in children/adolescents is key to identifying and managing dyslipidemia and reducing the risk of early-onset cardiovascular disease. This study shows that prevalence of elevated Lp(a) in high-risk Portuguese children is alarming, with over 30% at intermediate/high risk and nearly 1% at very high-risk (>430 nmol/L). Since Lp(a) is mostly genetically determined, one-time early screening in atrisk children is crucial for timely monitoring and prevention.
- Pulmonology
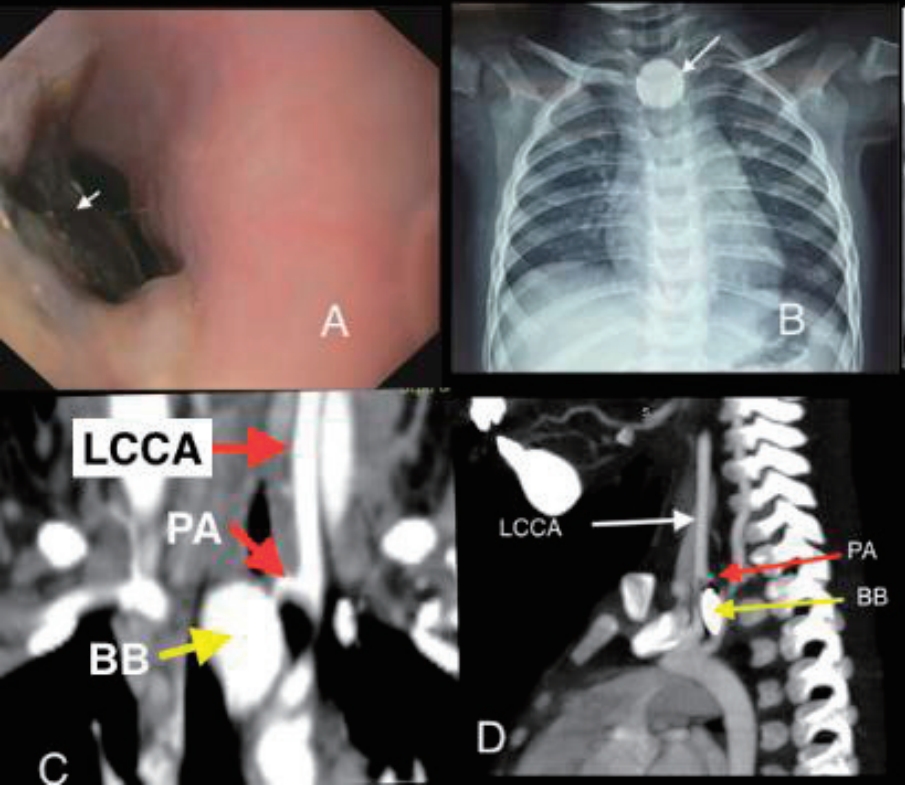
- Ciclesonide shows a lung-protective effect in neonatal hyperoxia-exposed rats
- Victoria Mielgo, Miguel A. Gomez-Solaetxe, Lara Olazar, Begoña Loureiro, Carmen Rey-Santano
- Clin Exp Pediatr. 2025;68(12):1023-1030. Published online October 2, 2025
-
Question: Bronchopulmonary dysplasia (BPD) is the most prevalent chronic lung disease of prematurity. Numerous nonpharmacological/pharmacological interventions have been investigated without clear consensus. Can ciclesonide, a new synthetic glucocorticoid, effectively treat BPD?
Finding: Ciclesonide mitigated hyperoxia-induced lung injury and right ventricular hypertrophy in newborn rats.
Meaning: These findings suggest that postnatal ciclesonide may be an alternative to existing corticosteroids for the treatment of BPD.
- Critical Care Medicine
- Cytokine profile of Post–cardiopulmonary bypass in children
- Kantara Saelim, Kanokpan Ruangnapa, Jirayut Jarutach, Pongsanae Duangpakdee, Smonrapat Surasombatpattana, Pharsai prasertsan
- Clin Exp Pediatr. 2025;68(12):1015-1022. Published online September 19, 2025
-

Question: Can cytokine levels predict low cardiac output syndrome (LCOS) in children post–cardiopulmonary bypass?
Finding: Elevated interleukin (IL)-6, IL-8, and tumor necrosis factor-α levels were associated with LCOS, with an increase in IL-8 of >56 pg/mL from baseline to immediately postoperative being the strongest predictor.
Meaning: Monitoring immediately postoperative IL-8 levels may help identify pediatric patients at risk of LCOS, enabling timely interventions to improve outcomes.
- Infection
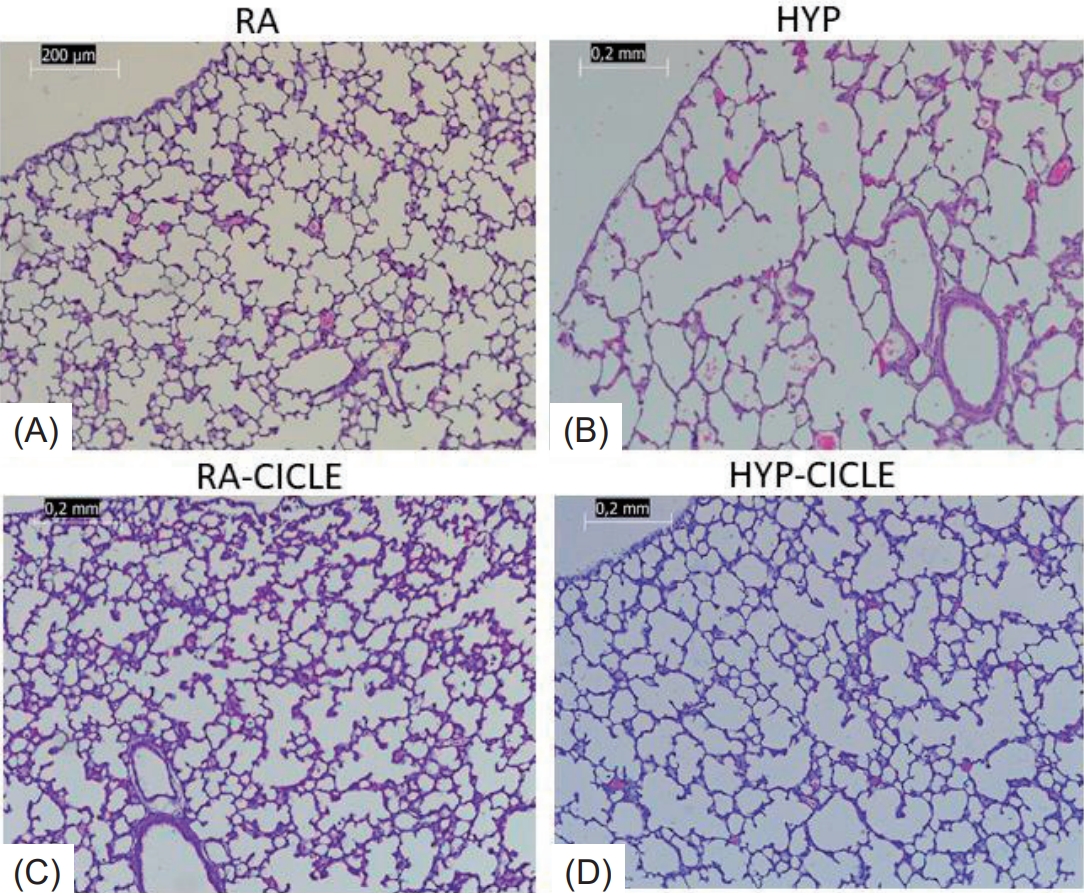
- Clinical outcomes and healthcare utilization of hospitalized children with influenza versus COVID-19
- David Chun-Ern Ng, Chuin-Hen Liew, Kah Kee Tan, Joanne Pereira, Muhammad Ihsan Roslan, Xiang Lin Cheng, Hui Yi Lim, Farah Nuruliayana A. Nazri, Asuwani Maran, Wan Fei Wong, Yasothai Chandran, Syaniza Shaharudin, Pon Ling Lau, Naveen Nair Gangadaran, Marlindawati Mohd Ali
- Clin Exp Pediatr. 2025;68(12):1007-1014. Published online October 2, 2025
-
Question: How do clinical presentations, healthcare resource utilization, and outcomes differ between children hospitalized with influenza versus coronavirus disease 2019 (COVID-19)?
Finding: Patients with influenza were older, were more symptomatic, and required greater healthcare resources, including intravenous fluids, empirical antibiotics, respiratory support, and pediatric intensive care unit admission.
Meaning: Influenza involves greater severity and a higher healthcare burden than COVID-19, highlighting the need for preventive strategies such as vaccination and hospital resource planning during seasonal outbreaks.
- Association between vitamin D polymorphisms and binding protein and COVID-19 risk and severity in children
- Victoria Giatraki, Helen Dimitriou, Georgia Martimianaki, Christos Tsatsanis, Emmanouil Galanakis, Chrysoula Perdikogianni
- Clin Exp Pediatr. 2025;68(12):998-1006. Published online October 22, 2025
-
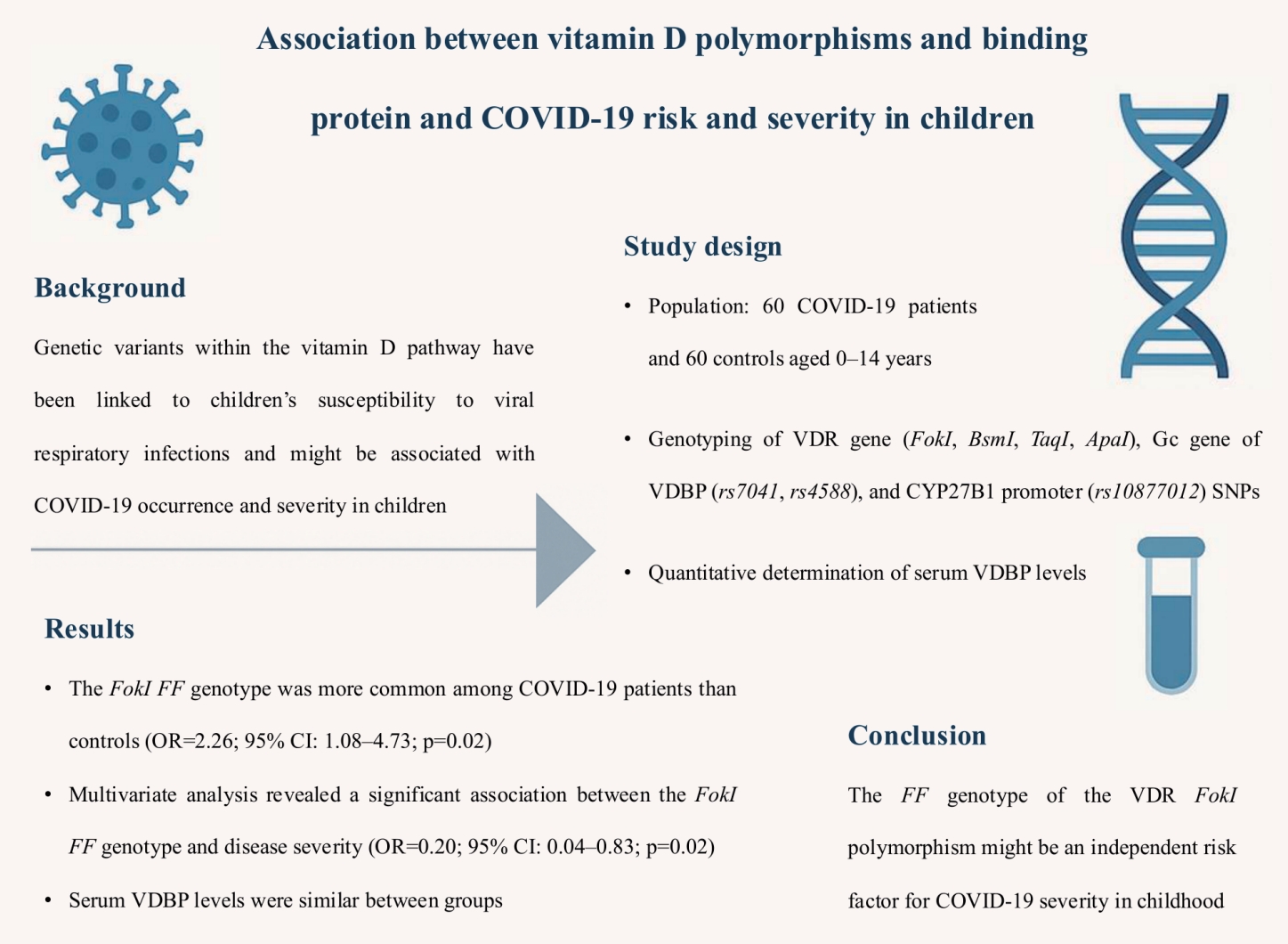
Question: Addressing crucial genetic variants within the vitamin D pathway and coronavirus disease 2019 (COVID-19) susceptibility, the vitamin D receptor, vitamin D binding protein, and CYP27B1-1260 polmorphisms might be associated with COVID-19 occurrence and severity in children.
Finding: The FokI FF genotype might be an independent risk factor for COVID-19 severity in childhood.
Meaning: This research may further elucidate genetic susceptibility to multisystem viral infections and establish genetic markers for severe clinical outcomes.
- Neonatology (Perinatology)
- Less invasive surfactant administration versus intubation-surfactant-extubation: a single-center retrospective study
- C.S. Jithin, A. Nalina, A. Shashidhar, P.N. Suman Rao
- Clin Exp Pediatr. 2025;68(12):991-997. Published online October 2, 2025
-
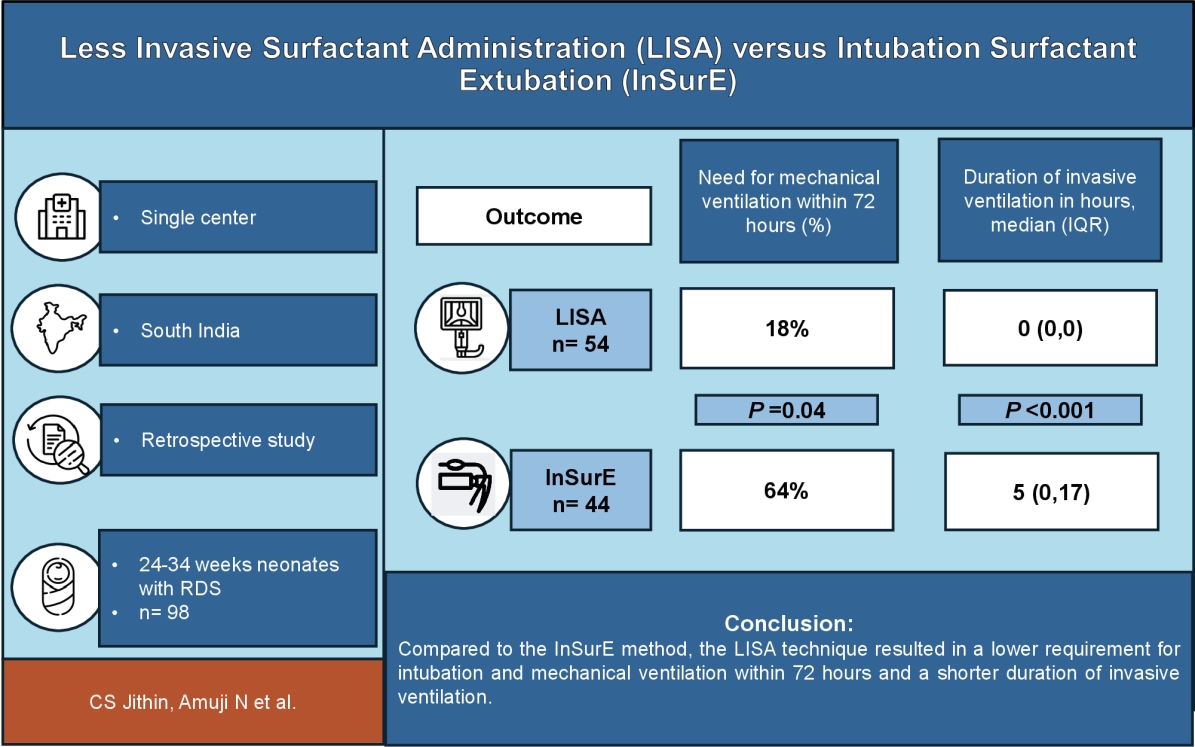
Question: Does less invasive surfactant administration (LISA) (vs. intubation-surfactant-extubation) improve clinical outcomes in preterm infants with respiratory distress syndrome?
Finding: LISA significantly reduced intubation and invasive mechanical ventilation needs within the first 72 hours and shortened the overall invasive respiratory support duration without increasing other morbidities.
Meaning: LISA is a less invasive and safer surfactant delivery alternative. Larger multicenter trials are needed to confirm its long-term safety and efficacy, especially in low- and middle-income countries.
- Hematology
- Assessment of natural killer cell subpopulations in pediatric patients with transfusion-dependent β-thalassemia major
- Fathia Ibrahim Elbassal, Mohamed Abdel Rehim Soliman, Nourhan Hossam Eldin Mohamed, Mai El-Sayad Abd El-Hamid, Hanan Hassan El-Sheity
- Clin Exp Pediatr. 2025;68(12):981-990. Published online September 12, 2025
-
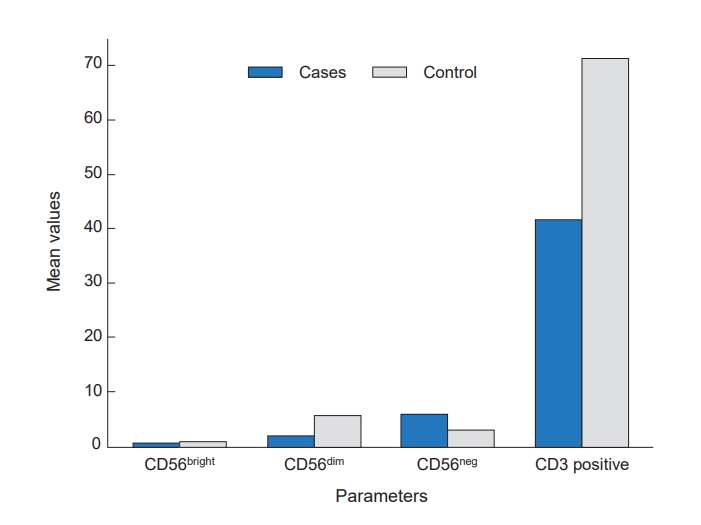
Question: How does iron overload affect immunity in pediatric patients with transfusion-dependent β-thalassemia major?
Finding: Iron overload in these patients is associated with disrupted natural killer (NK) cell subpopulations, reflecting impaired innate immunity.
Meaning: This highlights the need to monitor immune profile alongside iron status during thalassemia management.
- Oncology
- HLA‒B*58:01 and skin reactions in pediatric hematology and oncology patients treated with allopurinol
- Parisa Maneechai, Cholada Ratanatharathron, Jassada Buaboonam, Kleebsabai Sanpakit
- Clin Exp Pediatr. 2025;68(12):974-980. Published online October 2, 2025
-
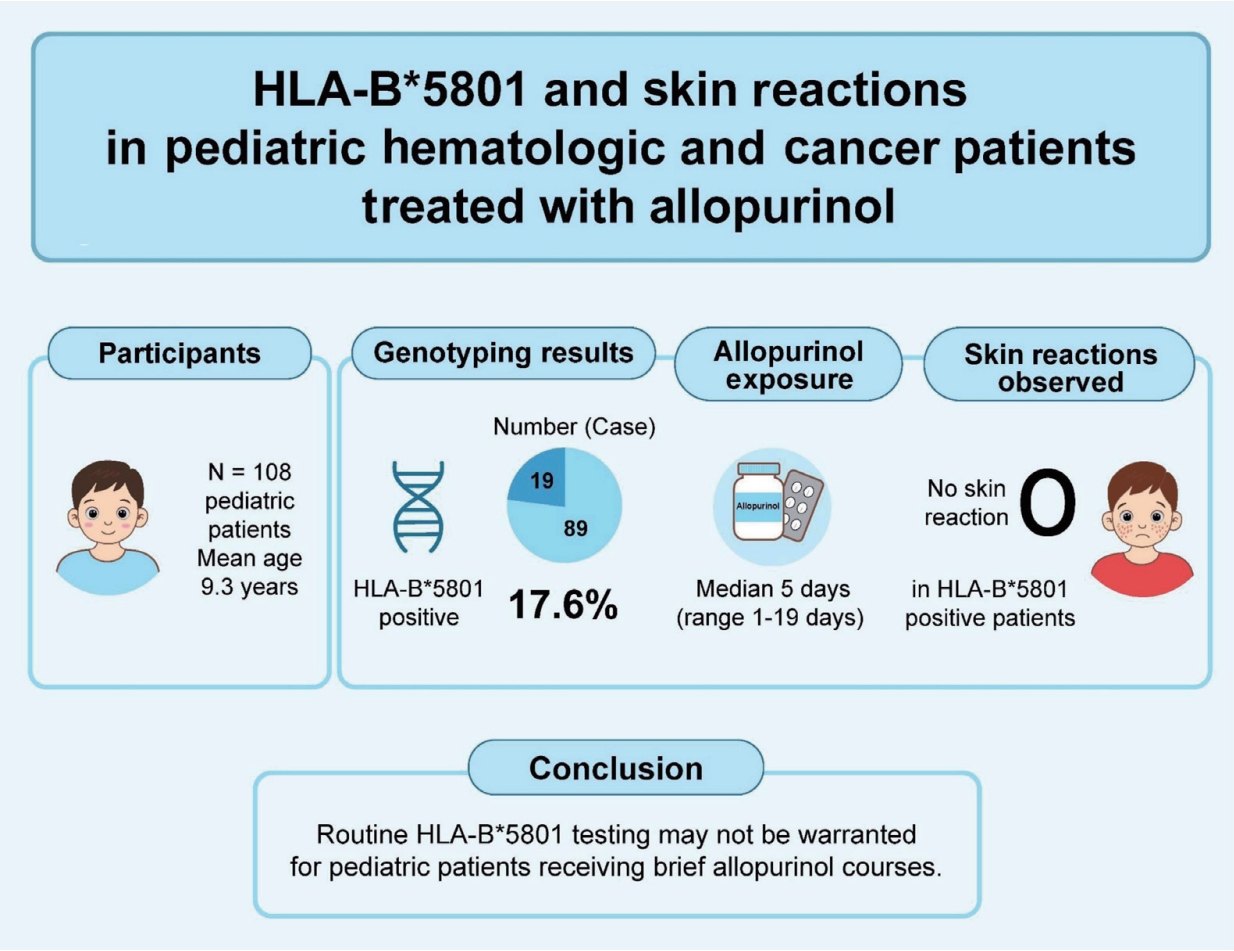
Question: Does human leukocyte antigen (HLA)–B*58:01 increase the risk of cutaneous reactions in pediatric patients with hematological and oncological diseases receiving allopurinol?
Finding: : Of 108 patients, 17.6% carried HLA–B*58:01 but none developed skin reactions. The only rash occurred in an HLA-B*58:01–negative patient.
Meaning: Short-duration allopurinol may mitigate severe cutaneous adverse reaction risk regardless of genotype. Routine HLA-B*58:01 screening may be unnecessary in pediatric patients with hematological and oncological diseases briefly receiving allopurinol.
- Editorial
- Infection
- Beyond COVID-19: meeting the challenge of evolving pediatric invasive group A streptococcal disease
- Han Wool Kim
- Clin Exp Pediatr. 2025;68(12):971-973. Published online November 26, 2025
-
Pediatric for invasive group A Streptococcus has resurged globally with increasing severity and toxin-mediated presentations. Beta-lactams remain the first-line treatment, but linezolid has emerged as a safe alternative in cases refractory to β-lactams. Early intravenous immunoglobulin use may improve outcomes in severe streptococcal toxic shock syndrome cases, while C-reactive protein and procalcitonin aid early risk stratification. Integrating global surveillance and individualized therapy is crucial in the postpandemic era.
- Review Article
- Nutrition
- Exploring nutritional screening tools for hospitalized children: a narrative review
- Pankaj Soni, Amit Agrawal, Gaurav Jadon
- Clin Exp Pediatr. 2025;68(12):963-970. Published online October 22, 2025
-
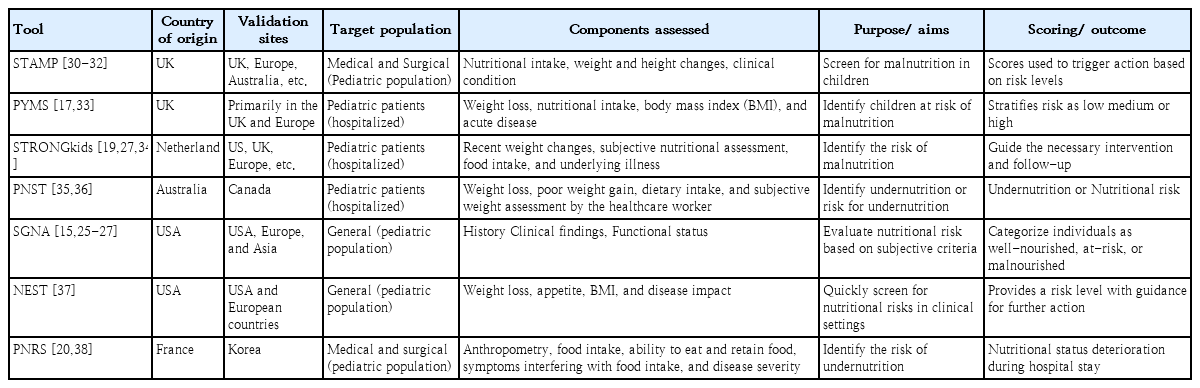
Malnutrition is frequently identified in hospitalized children, and the use of nutritional screening tools is crucial for assessing their nutritional status during their hospital admission and stay. Common tools include the Pediatric Yorkhill Malnutrition Score, Screening Tool for Assessment of Malnutrition in Pediatrics, and Screening Tool for Risk of Nutritional Status and Growth. However, these tools have varying sensitivities and specificities, and none is recommended for all hospitalized children.
- Oncology
- Breaking the barrier: a guidelines-based review of antiangiogenesis drug resistance in pediatric cancer therapy
- Nader Shakibazad, Mahdi Shahriari, Mani Ramzi
- Clin Exp Pediatr. 2025;68(12):952-962. Published online November 24, 2025
-
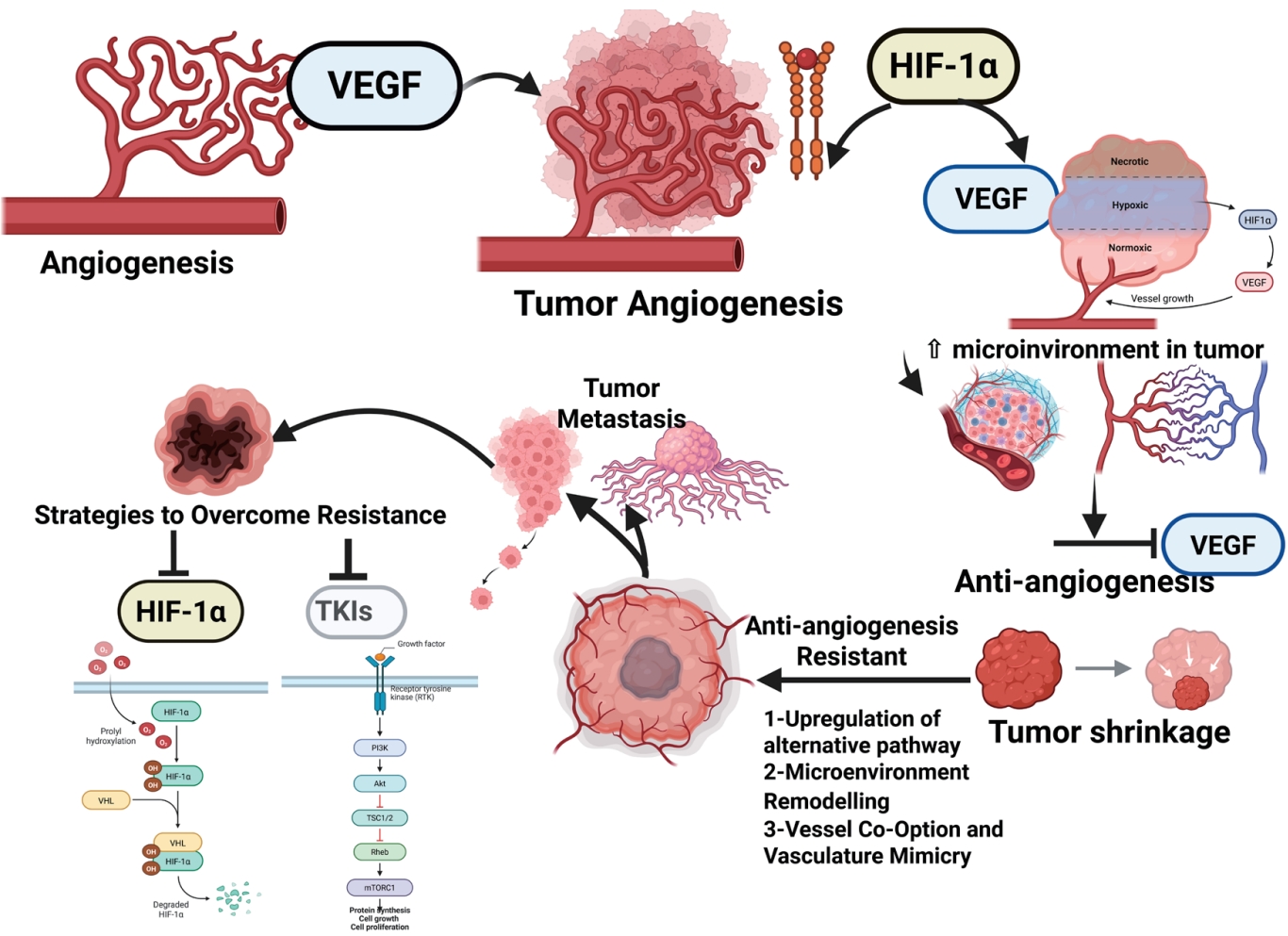
Antiangiogenic therapy resistance in pediatric cancers involves alternative angiogenic pathways, microenvironmental support, hypoxia-driven signaling, metabolic reprogramming, and structural adaptations such as vascular co-option. Metabolic adaptation highlights tumor plasticity. Effective treatments combine immunotherapy with biomarkers. To address vascular endothelial growth factor limitations, emerging targets include hypoxia-inducible factor-2α, endoglin, CXCR4, angiopoietin/Tie2, and bispecific antibodies. In resource-constrained settings, the guidelines recommend low-dose chemotherapy plus oral multiantiangiogenic agents to ensure improved accessibility and treatment outcomes.
- Original Article
- General Pediatrics
- Effectiveness of Kinder Lebensqualität Fragebogen (KINDL) and Children’s Somatic Symptom Inventory-24 (CSSI-24) for measuring postacute sequelae of COVID-19 in children: a diagnostic validation study
- Lawrence Shih-Hsin Wu, Pei-Chi Chen, Xiao-Ling Liu, Shu-Tsen Liu, Chi-Hung Wei, Yu-Lung Hsu, Kai-Sheng Hsieh, Huan-Cheng Lai, Chien-Heng Lin, Chieh-Ho Chen, An-Chyi Chen, I-Ching Chou, Wen-Jue Soong, Hui-Ju Tsai, Chung-Ying Lin, Jiu-Yao Wang
- Clin Exp Pediatr. 2025;68(11):944-951. Published online September 12, 2025
-

Question: Although children with postacute sequelae of coronavirus disease 2019 (PASC) may experience persistent symptoms that affect their quality of life (QoL), a screening tool for identifying high-risk children is lacking.
Finding: Kinder Lebensqualität fragebogen (KINDL) and Children's Somatic Symptom Inventory-24 (CSSI-24) were significantly correlated. An optimal KINDL cutoff score (74.75) detected those at high risk of a reduced QoL.
Meaning: Integrating KINDL and CSSI-24 into routine pediatric outpatient care may enable timely identification and interventions for children at risk of PASC-related impairments.
- Gastroenterology
- Fecal microbiome profiles in infants with biliary atresia versus nonbiliary atresia cholestasis: a pilot study
- Nur Azizah, Fadilah Fadilah, Silvia Werdhy Lestari, Muzal Kadim, Fithriyah Sjatha, Hanifah Oswari
- Clin Exp Pediatr. 2025;68(11):932-943. Published online August 20, 2025
-

Question: How does the gut microbiota profile of infants with biliary atresia (BA) differ from that of infants with non-BA cholestasis and healthy infants in the Indonesian population?
Finding: The unique fecal microbiome composition of the BA group differed significantly from that of the other 2 groups.
Meaning: There is an urgent need to improve dysbiosis in BA and non-BA cholestasis to prevent worsening liver injury in cholestasis.
- Infection
- Evolving treatment strategies for invasive Streptococcus pyogenes in children in the postpandemic era
- Laura Buricchi, Giuseppe Indolfi, Marco Renni, Elisabetta Venturini, Luisa Galli, Elena Chiappini
- Clin Exp Pediatr. 2025;68(11):921-931. Published online August 11, 2025
-

Question: What are the roles of linezolid, intravenous immunoglobulin (IVIG), and corticosteroids in pediatric invasive group A streptococcal infection (iGAS)? Can any improve outcomes beyond beta-lactams and clindamycin?
Finding: Two of 46 patients with iGAS died. Nearly all received beta-lactams plus clindamycin. Linezolid was effective in refractory cases. IVIG and corticosteroids had variable efficacies.
Meaning: Linezolid may be valuable in refractory cases. IVIG may be considered in severe presentations. The role of corticosteroids remains less clearly defined.
- Serum copper and ceruloplasmin levels as biomarkers reflecting liver fibrosis in children with autoimmune hepatitis
- Salma Abdel Megeed Nagi, Mai Ibrahim Elashmawy, Amany E. Elashkar, Mohamed Zaeim Hafez, Ashraf A.E. Emara, Osama Mohammad Abdelhay, Albayoumi A.B. Fouda, Mohamed AbdelAziz Doma, Ahmad Mohamed Awad, Ahmed Mohammed Saba, Hesham Abdelrahman Ahmed, Ahmed Mohamed Gad Allah, Fatma Mahmoud Abdelraheem, Mohamed A. Gad, Mohamad A. Soliman, Tamer I. Abdalrhman, Khaled Hassaan Awad, Ismael A.K.M. El-lebedy, Mostafa M. Abdelnaser, Mohammed Z. Abdel Kareem, Marwa Fekry Hassan, Shymaa Sobhy Menshawy Khalifa
- Clin Exp Pediatr. 2025;68(11):909-920. Published online August 6, 2025
-

· A total of 159 children with autoimmune hepatitis (AIH; 60.3% female, 13.2% type 2 AIH) were identified. According to a global study, the estimated annual incidence of AIH in Egypt is 1.28 cases per 100,000 inhabitant-years.
· No studies to date have examined the serum levels of copper or ceruloplasmin in children with AIH. Therefore, here we investigated whether serum copper and ceruloplasmin levels are useful for identifying liver fibrosis in children with AIH.
· Serum copper and ceruloplasmin levels may provide important information for the identification of advanced liver fibrosis in children with AIH.
- Hematology
- Evaluation of Bak and Bcl-Xl gene expression among pediatric patients with acute primary immune thrombocytopenia
- Amira Zaki Badawy, Samia Hassan Kandel, Iman Aly Ahmedy, Mahmoud Ahmed Elhawy, Sally Mohamed El-Hefnawy, Dina Fouad Sief El-Nasr Zidan, Hanan Hassan El-sheity
- Clin Exp Pediatr. 2025;68(11):901-908. Published online August 6, 2025
-

The B-cell lymphoma protein 2 family proteins Bak and Bcl- Xl, important markers of apoptosis, may contribute to primary immune thrombocytopenia (ITP). Thus, their expression may serve as biomarkers for the diagnosis and monitoring of pediatric ITP. Targeting these pathways may improve platelet survival, particularly in treatment-resistant cases. Personalized treatments based on apoptotic profiles can optimize therapy and reduce the unnecessary use of immunosuppressive drugs.
- General Pediatrics
- Comparative analysis of goal attainment for helmet therapy versus conservative management for positional plagiocephaly in infants
- Bjoern Vogt, Ariane Deutschle, Georg Gosheger, Adrien Frommer, Andrea Laufer, Henning Tretow, Robert Roedl, Gregor Toporowski
- Clin Exp Pediatr. 2025;68(11):892-900. Published online October 2, 2025
-

Question: Is helmet therapy more effective than conservative management in treating positional plagiocephaly?
Finding: Both approaches reduced cranial asymmetry with comparable correction speed. Helmet therapy showed a trend toward greater severity reduction.
Meaning: Early treatment initiation was the strongest predictor of improvement. Helmet therapy may offer additional benefit in more severe cases.
- Endocrinology
- Long-term epidemiological insights into rickets: a nationwide population-based retrospective study
- Chun-Hao Chu, Ying-Chuan Chen, Pei-Yao Liu, Chun-Chieh Hu, Yu-Lung Lin, Feng-Chih Kuo, Chieh-Hua Lu, Tzu-Ju Hsu, Yu-Tung Hung, Fuu-Jen Tsai, Chien-Ming Lin
- Clin Exp Pediatr. 2025;68(11):879-891. Published online August 20, 2025
-

Question: What are the nationwide trends and mortality risk factors of nutritional versus hereditary rickets among children in Asia?
Finding: In 2012–2018, the incidence of rickets steadily increased, whereas mortality rates declined. Mortality is associated with a low household income, anemia, chronic kidney disease, secondary hyperparathyroidism, and a prolonged hospital stay.
Meaning: Early diagnosis and targeted interventions addressing social and medical vulnerabilities are critical to reducing ricket-related mortality.
- Nutrition
- Success rates of conservative treatment and optimal surgical timing for pediatric chylothorax
- Pakwan Kaewchusen, Narumon Densupsoontorn, Supaluck Kanjanauthai, Puthita Saengpanit
- Clin Exp Pediatr. 2025;68(11):871-878. Published online August 6, 2025
-

Question: What is the success rate of conservative treatment for pediatric chylothorax, and when should surgical intervention be employed?
Finding: Overall success rate of conservative treatment was 83.3%. Surgically related etiologies and lower peak pleural fluid drainage rates were significantly associated with successful conservative management of pediatric chylothorax.
Meaning: If chylous drainage persists at ≥10 mL/kg/day beyond 2 weeks of optimal conservative treatment, surgical intervention should be considered.
-

-
-
6.02024CiteScore98th percentilePowered by
-
Impact Factor3.6
-
- TOPICS
- ARTICLE CATEGORY
- Editorial Office
-
Korean Pediatric Society
#1606 Seocho World Officetel, 19 Seoun-ro, Seocho-ku, Seoul 06732, Korea
Tel: +82-2-3473-7306 Fax: +82-2-3473-7307 E-mail: office@e-cep.org
Clinical and Experimental Pediatrics is an open access journal. All articles are distributed under the terms of the Creative Commons Attribution NonCommercial License (http://creativecommons.org/licenses/by-nc/4.0/)
Copyright © 2026 by Korean Pediatric Society.