Article Contents
| Clin Exp Pediatr > Volume 67(2); 2024 |
|
Abstract
Background
Purpose
Methods
Results
Footnotes
Fig. 1.
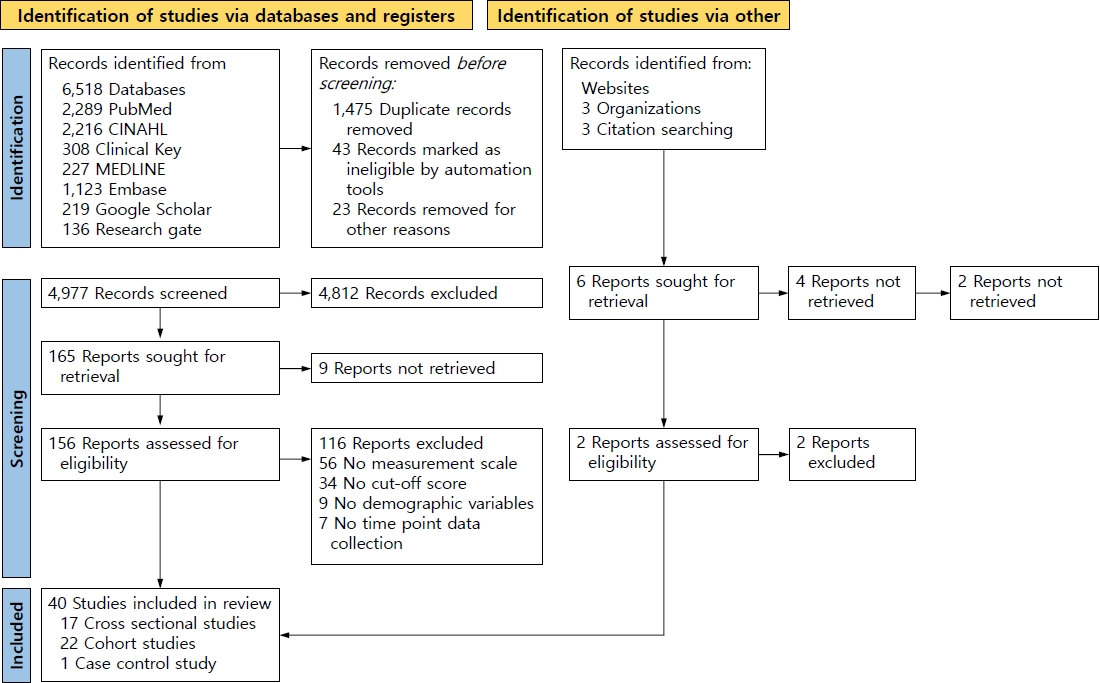
Fig. 2.
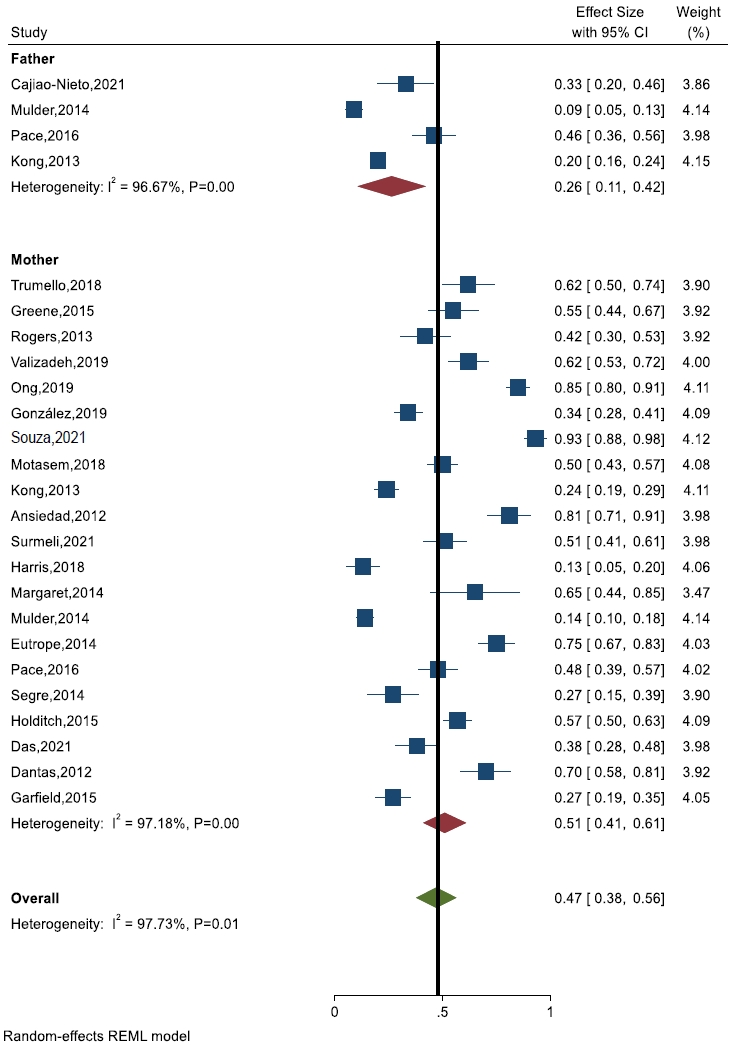
Fig. 3.
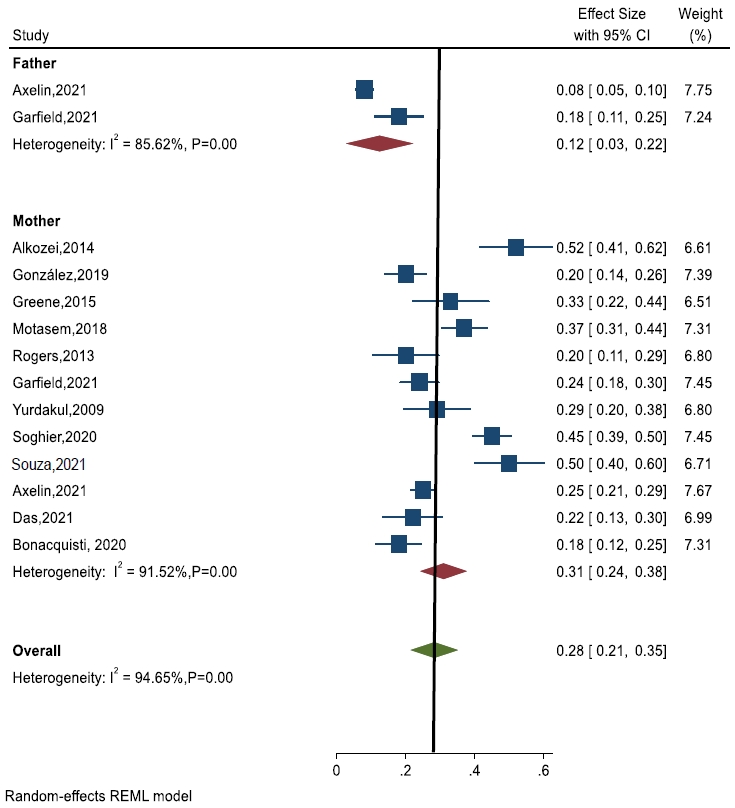
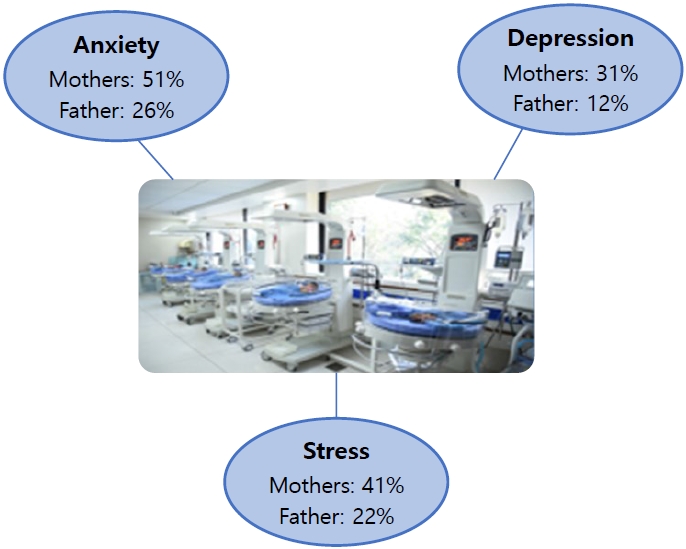
Fig. 4.
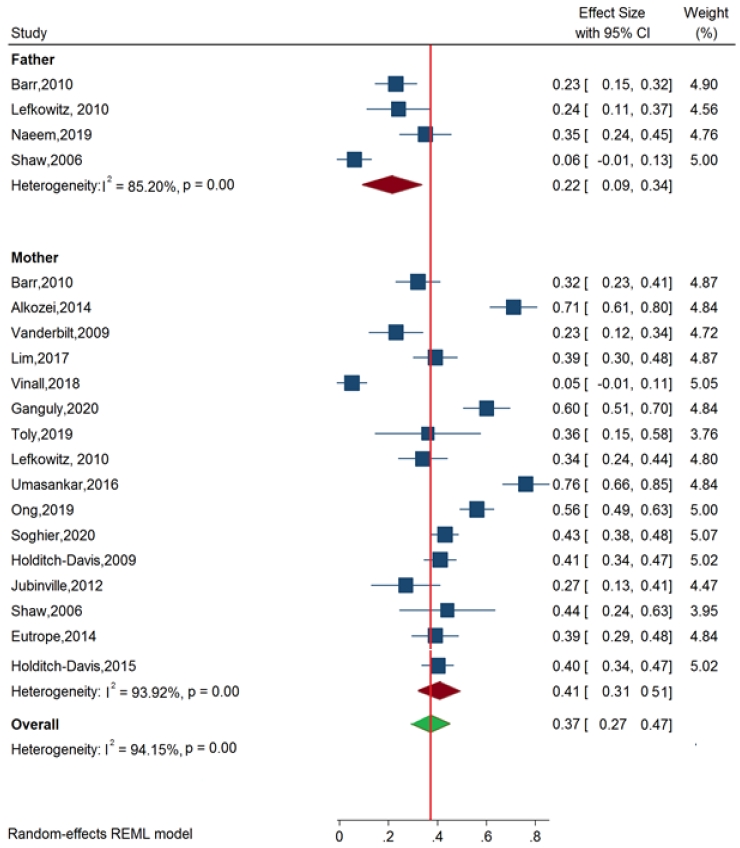
Fig. 5.
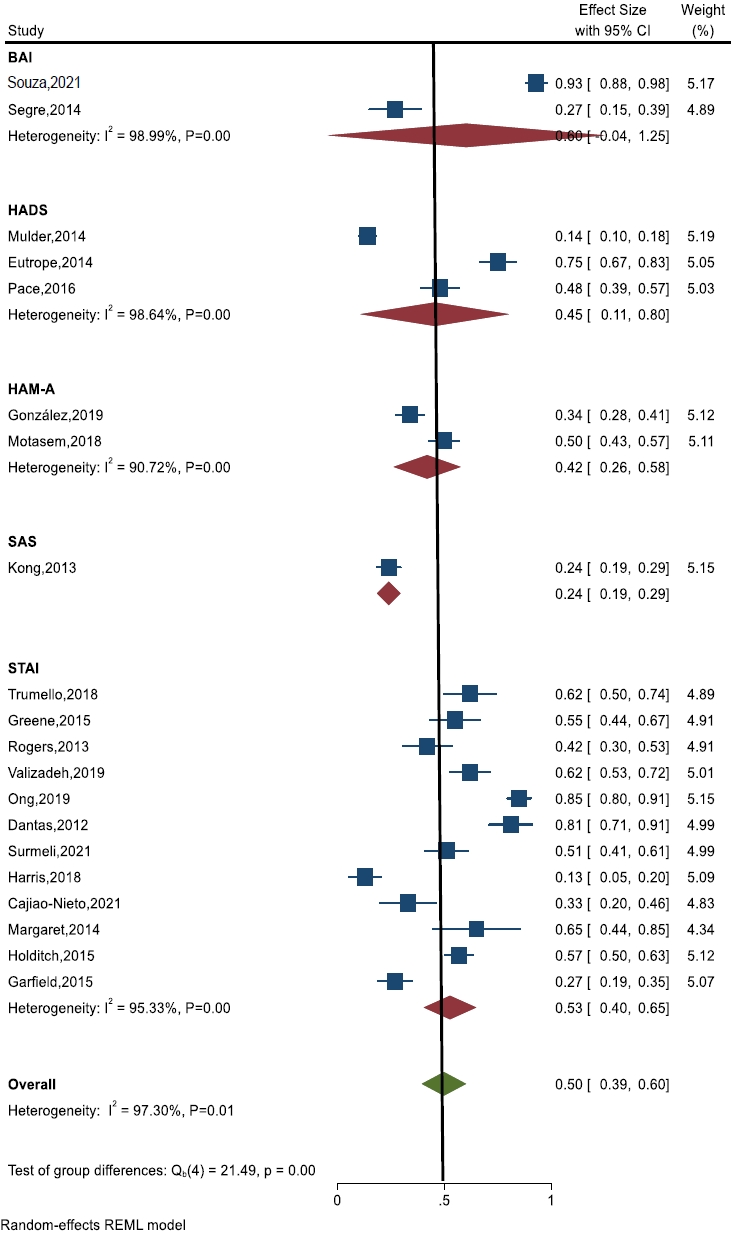
Fig. 6.
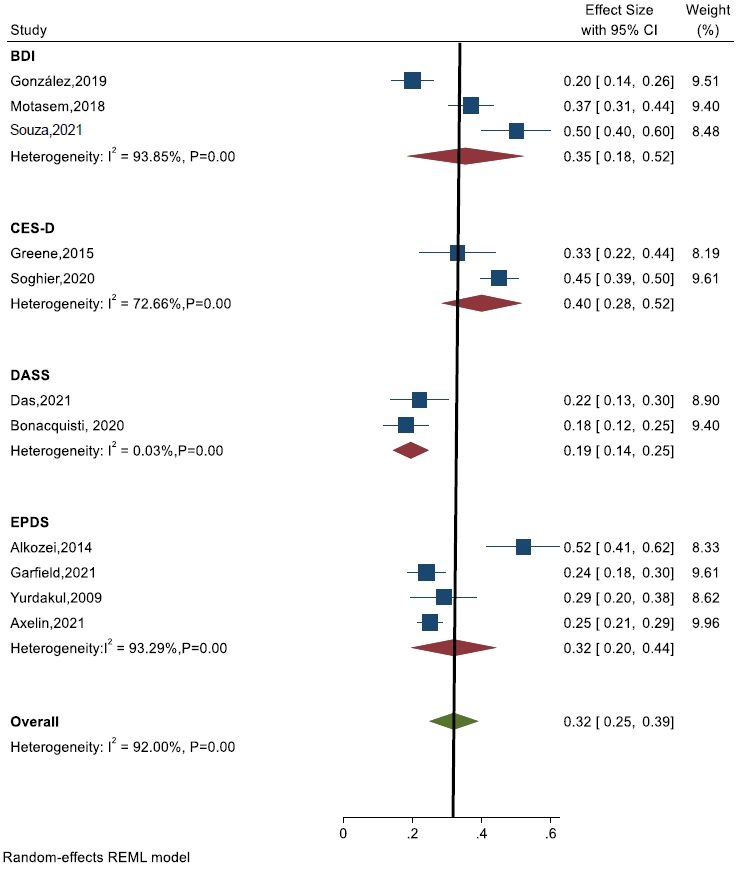
Fig. 7.
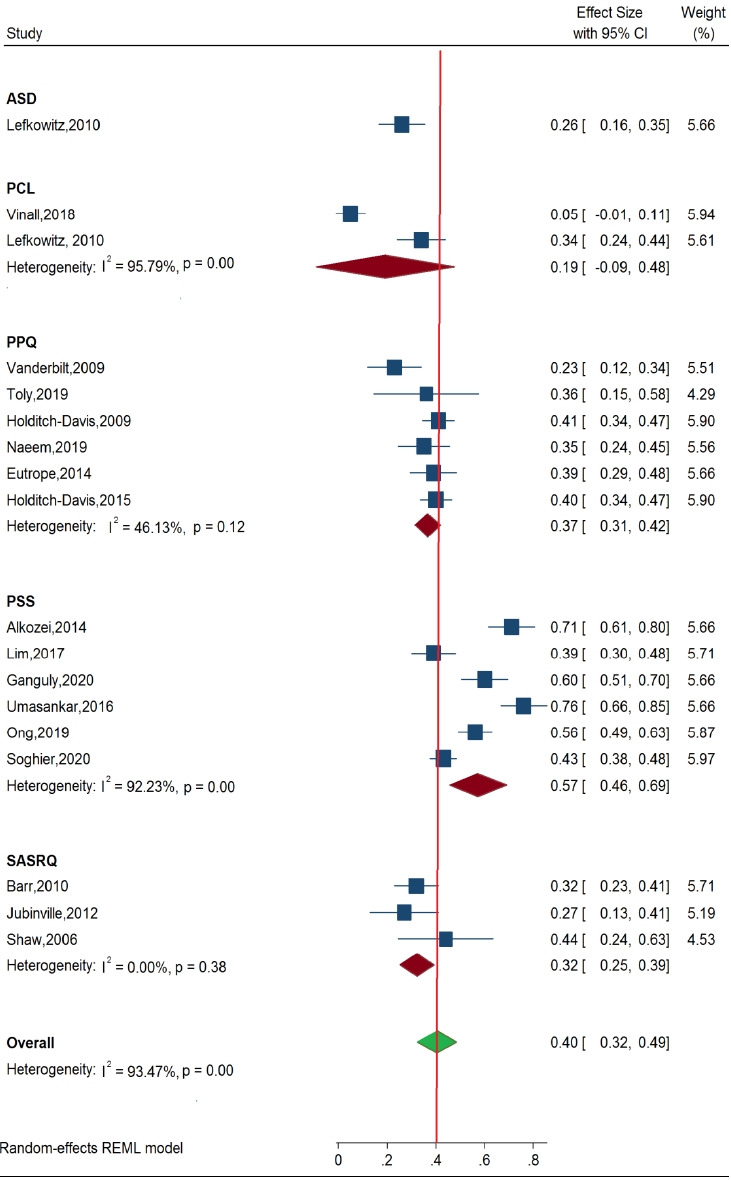
Table 1.
| Study | Country | Representativeness of samples >70% response (1) | Sample size >200 (2) | Response rate >80% (3) | Validated tool with cutoff (4) | Detail statistical information, not required further calculations (5) | Total Scores | Study quality |
|---|---|---|---|---|---|---|---|---|
| Carter et al. [44] (2007) | NZ | * | * | * | * | * | 5/5 | Low risk |
| Yurdakul et al. [6] (2009) | Turkey | * | - | * | - | * | 3/5 | Low risk |
| Vanderbilt et al. [22] (2009) | USA | * | - | * | - | * | 3/5 | Low risk |
| Holditch-Davis et al. [23] (2009) | USA | * | * | * | * | * | 5/5 | Low risk |
| Holditch-Davis et al. [24] (2015) | USA | * | - | * | * | * | 4/5 | Low risk |
| Lefkowitz et al. [25] (2010) | USA | * | - | * | - | * | 3/5 | Low risk |
| Barr [26] (2010) | Australia | * | - | * | * | * | 4/5 | Low risk |
| Dantas et al. [52] (2012) | Brazil | * | - | * | * | * | 4/5 | Low risk |
| Jubinville et al. [27] (2012) | Canada | * | - | * | * | * | 4/5 | Low risk |
| Kong et al. [7] (2013) | China | * | * | * | - | * | 4/5 | Low risk |
| Alkozei et al. [8] (2014) | USA | * | - | * | - | * | 3/5 | Low risk |
| Eutrope et al. [28] (2014) | France | * | - | * | - | * | 3/5 | Low risk |
| Mulder et al. [29] (2014) | NZ | * | - | * | - | * | 3/5 | Low risk |
| Margaret et al. [9] (2014) | India | * | - | * | * | * | 4/5 | Low risk |
| Segre et al. [10] (2014) | USA | * | * | * | - | * | 4/5 | Low risk |
| Garfield et al. [11] (2015) | USA | * | - | * | * | * | 4/5 | Low risk |
| Umasankar et al. [12] (2016) | Sri Lanka | * | - | * | - | * | 3/5 | Low risk |
| Pace et al. [30] (2016) | Australia | * | * | * | - | * | 4/5 | Low risk |
| Lim et al. [13] (2017) | Malaysia | * | * | * | - | * | 4/5 | Low risk |
| Harris et al. [31] (2018) | USA | * | - | * | * | * | 4/5 | Low risk |
| Salah et al. [14] (2018) | Palestine | * | - | * | * | * | 4/5 | Low risk |
| Vinall et al. [32] (2018) | Canada | * | - | * | - | * | 3/5 | Low risk |
| Trumello et al. [33] (2018) | Italy | * | - | * | * | * | 4/5 | Low risk |
| Valizadeh et al. [15] (2019) | Iran | * | - | * | * | * | 4/5 | Low risk |
| Ong et al. [34] (2019) | Malaysia | * | - | * | * | * | 4/5 | Low risk |
| González-Hernández et al. [35] (2019) | Mexico | * | * | * | - | * | 4/5 | Low risk |
| Toly et al. [36] (2019) | USA | * | - | * | * | * | 4/5 | Low risk |
| Ganguly et al. [16] (2020) | India | * | - | * | - | * | 3/5 | Low risk |
| Bonacquisti et al. [43] (2020) | USA | * | - | * | - | * | 3/5 | Low risk |
| Soghier et al. [17] (2020) | USA | * | - | * | * | * | 4/5 | Low risk |
| Axelin et al. [37] (2021) | Finland | * | - | * | * | * | 4/5 | Low risk |
| Cajiao-Nieto et al. [38] (2021) | Spain | * | - | * | - | * | 3/5 | Low risk |
| Das et al. [18] (2021) | USA | - | - | * | * | * | 3/5 | Low risk |
| Garfield et al. [39] (2021) | USA | * | - | * | * | * | 4/5 | Low risk |
| Souza et al. [19] (2021) | Brazil | * | - | * | * | * | 4/5 | Low risk |
| Greene et al. [40] (2015) | USA | - | - | * | * | * | 3/5 | Low risk |
| Rogers et al. [41] (2013) | USA | * | - | * | * | * | 4/5 | Low risk |
| Surmeli Onay et al. [20] (2021) | Turkey | * | - | * | * | * | 4/5 | Low risk |
| Naeem et al. et al. [42] (2019) | Iran | * | - | * | * | - | 3/5 | Low risk |
Table 2.
| Study | Country | Study design | Sample size |
Characteristics parents |
Characteristics of newborn |
Measurement tool |
Outcome of individual studies | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participants | Mean age in years range b/w | Mean education above HS | Mean GA range b/w (wk) | Mean weight range b/w (kg) | Name of scale | Cutoff score | Point of data collection | |||||
| Carter et al. [44] (2007) | NZ | Cohort | 447 | Parents | M-30.1 | * | 35.1 | 2.47 | HADS | >12 | <3 Weeks | After 9 months of hospitalization parents were not reported anxiety or depression symptoms. |
| M-242 | F-33.1 | |||||||||||
| F-205 | ||||||||||||
| Yurdakul et al. [6] (2009) | Turkey | CS | 88 | NICU | 30 | 60 | 32.6 | 1.95 | EPDS | >13 | <4 Weeks | Depression and anxiety correlated each other among NICU mothers. |
| Mother | ||||||||||||
| Vanderbilt et al. [22] (2009) | USA | Cohort | 59 | Mother | 29 | 39 | 34 | 2.35 | PPQ | >6 | <7 days | Early intervention was reduced the posttraumatic stress. |
| Holditch-Davis et al. [23] (2009) | USA | Cohort | 177 | Mother | 25.8 | * | 28.3 | 1.10 | PPQ | >6 | During admis | GA, away from home and hospitalization were trigger factors heighten the mental stress in NICU mother. |
| Holditch-Davis et al. [24] (2015) | USA | Cohort | 232 | Mother | 27 | 31 | 27.2 | 1.06 | STAI | >47 | During admis | Neonate mother indicating different kind of psychological distress to NICU units. |
| PPQ | >6 | |||||||||||
| Lefkowitz et al. [25] (2010) | USA | Cohort | 128 | Parents | M-29 | M-21 | <30 | * | ASD | >1 symptom | <7 days | Parents were reported depression and anxiety during hospitalization of their newborn infants. |
| M-87 | F-33 | F-9 | ||||||||||
| F-41 | ||||||||||||
| Dantas et al. [52] (2012) | Brazil | CS | 60 | Mother | 26.5 | 11 | 31.5 | 1.49 | STAI | >40 | During admission | Mother reported high prevalence of anxiety during admission of their newborn baby in NICU unit. |
| Jubinville et al. [27] (2012) | Canada | Cohort | 40 | Mother | 29.2 | 24 | 29 | 1.37 | SASRQ | >38 | <7 days | Safe hospital environment may reduce the psychological distress among NICU parents. |
| Alkozei et al. [8] (2014) | USA | CS | 85 | Mother | 31.9 | 51 | 30.1 | 1.37 | EPDS | >10 | <7 days | NICU mother already psychological disturbed, addition stressor factors including away from home further increases the anxiety & depression. |
| PSS (NICU) | >3 | |||||||||||
| Eutrope et al. [28] (2014) | France | Cohort | 100 | Mother | 29.8 | 79 | <32 | 1.32 | PPQ | >19 | <7 days | Known history of trauma & present birth weight significantly increased anxiety & depression in NICU mother. |
| HADS | >8 | |||||||||||
| Mulder et al. [29] (2014) | NZ | Cohort | 447 | Parents | M-30.1 | M-126 | 35 | 2.47 | HADS | >11 | During admission | There was no long-term mental distress among mother of NICU babies. |
| M-242 | F-33.1 | F-* | ||||||||||
| F-205 | ||||||||||||
| Margaret et al. [9] (2014) | India | CS | 20 | Mother | 20-35 | 12 | 30-34 | 0.75-3.5 | STAI | >40 | <7 days | Mothers exhibit anxiet y towards hospitalization. |
| Segre et al. [10] (2014) | USA | CS | 200 | Mother | 28.1 | 14 | 34 | 0.37-3.7 | BAI | >16 | 2 Weeks | The risk factors like premature, infant illness were prime reason for anxiety and depression in NICU mother. |
| Garfield et al. [11] (2015) | USA | CS | 113 | Mother | 24.7 | 49 | <37 | 1.07 | STAI | * | <4 Weeks | Low income & poor family support demonstrated higher psychological problems in NICU mother. |
| PSS | >6 | |||||||||||
| Umasankar et al. [12] (2016) | Sri Lanka | CS | 75 | Mother | 30 Manually | * | 30-36 | 1.5 | PSS (NICU) | >3 | <7 days | Alteration in parenteral role & hospitalization heighten the stress among NICU mother. |
| Pace et al. [30] (2016) | Australia | Cohort | 214 | Parents | M-32.7 | 92 | 27.7 | 1.02 | HADS | >8 | Before D/C | The anxiety and depression elevated in beginning of NICU and it became declines over period of times. |
| M-113 | F-34.7 | |||||||||||
| F-101 | ||||||||||||
| Lim et al. [13] (2017) | Malaysia | CS | 104 | Parents | 30.1 | 49 | * | * | PSS (NICU) | >3 | <7 days | Considerably more stress reported in NICU mother than father of newborn admitted in NICU. |
| M-62 | ||||||||||||
| F-42 | ||||||||||||
| Harris et al. [31] (2018) | USA | Cohort | 37 | Mother | 29.7 | * | 32 | 1.10 | STAI | >33 | <7 days | There was no psychological difference between termed and preterm babies of NICU mother. |
| Salah et al. [14] (2018) | Palestine | CS | 195 | Mother | 28.2 | 90 | * | 2.76 | BDI | >10 | Social factors increase the psychological distress in NICU mother. | |
| HAM-A | >17 | |||||||||||
| Vinall et al. [32] (2018) | Canada | Cohort | 36 | Mother | 31 | * | <37 | * | PCL | >33 | Before/C | Traumatic procedure in neonatal unit increased the maternal stress among NICU mother. |
| Trumello et al. [33] (2018) | Italy | Cohort | 62 | Mother | 34 | 20 | <32-37 | 1.68 | STAI | >39 | <7 days | Newborn admission was negatively impact and increases emotional distress. |
| Valizadeh et al. [15] (2019) | Iran | CS | 100 | Mother | ±31 | 56 | 34 | 1.85 | STAI | >40 | <7 days | Mother with higher education and prematurity babies demonstrated state anxiety during hospitalization. |
| Ong et al. [34] (2019) | Malaysia | Cohort | 180 | Mother | 29.3 | 104 | 31.1 | 1.46 | STAI | >40 | After first week | Mothers exhibit high anxiety symptoms during NICU admission of their babies. |
| PSS (NICU) | * | |||||||||||
| González-Hernández et al. [35] (2019) | Mexico | Cohort | 188 | Mother | 24.7 | 9 | * | * | HAM-A | >18 | <2 Weeks | Age and occupation were significance with anxiety and depression of NICU mother. |
| BDI | >10 | |||||||||||
| Toly et al. [36] (2019) | USA | Cohort | 19 | Mother | 25.6 | 11 | 29.7 | 1.54 | PPQ | >19 | During admission | Signif icance dif ference bet ween depression and stress among mother of premature babies admitted in NICU unit. |
| Ganguly et al. [16] (2020) | India | CS | 100 | Parents | F-27 | 36 | * | 1.5 | PSS (NICU) | * | After 24 hr of admission | Stress was not significance between mother and father but length of hospitalization significances to stress among NICU parents. |
| M-30 | ||||||||||||
| Bonacquisti et al. [43] (2020) | USA | Cohort | 127 | Mother | 29.6 | 26% | * | * | DASS | .>21 | During admission | Mother and newborn separation increases the psychological symptoms among NICU mothers. |
| Ganguly et al. [16] (2020) | India | CS | 100 | Parents | F-27 | 36 | * | 1.5 | PSS (NICU) | * | After 24 hr of admission | Stress was not significance between mother and father but length of hospitalization significances to stress among NICU parents. |
| M-30 | ||||||||||||
| Bonacquisti et al. [43] (2020) | USA | Cohort | 127 | Mother | 29.6 | 26% | * | * | DASS | .>21 | During admission | Mother and newborn separation increases the psychological symptoms among NICU mothers. |
| Soghier et al. [17] (2020) | USA | CS | 300 | Parents | 30 | 225 | 28-37 | 1-2.5 | CESD-10 | >10 | Before D/C | Even term infant parents demonstrated high depression. Social support inversely proportional to depression. |
| M-267 | PSS | >3 | ||||||||||
| F-33 | ||||||||||||
| Axelin et al. [37] (2021) | Finland | Cohort | 1101 | Parents | M-31 | M-337 | 31.8 | 1.58 | EPDS | >13 | During D/C | Provision of family center care may improve mental wellbeing of parents of newborn admitted in NICU unit. |
| M-635 | F-33 | F-231 | ||||||||||
| F-466 | ||||||||||||
| Cajiao-Nieto et al. [38] (2021) | Spain | Cohort | 51 | Father | 20-45 | 39 | <37 | * | STAI | * | 3rd day | Father repor ted anxiet y towards parenthood and NICU unit during hospitalization. |
| Das et al. [18] (2021) | USA | CS | 96 | Mother | 28.4 | * | 35.2 | 2.33 | DASS | .>21 | Before 44 weeks | Early screening may reduce the psychological symptoms among NICU mothers. |
| PHQ | >9 | |||||||||||
| Garfield et al. [39] (2021) | USA | Cohort | 431 | Parents | M-33 | M-175 | 31.5 | 1.87 | EPDS | >13 | <7 days | Parents were demonstrated depression symptoms during NICU admission of their babies. |
| M-230 | F-35.1 | F-149 | ||||||||||
| F-201 | ||||||||||||
| Souza et al. [19] (2021) | Brazil | CS | 91 | Mother | >18 | 48 | 37 | 2.69 | BAI | >1 | Before D/C | Social factors heighten the psychological discomfort among NICU parents. |
| BDI | >10 | |||||||||||
| Greene et al. [40] (2015) | USA | Long | 69 | Moher | 27 | 52 | 27.5 | 0.95± 0.24 | STAI | >40 | Before 2nd Weeks | Psychological problems often reported in primipara mothers than multipara. Therefore, distractive intervention targeting these populations. |
| Cohort | CES-D | >16.6 | ||||||||||
| >19 | ||||||||||||
| Rogers et al. [41] (2013) | USA | Long | 73 | Mother | 27.2 | 39 | 25.5 | * | STAI | >40 | At time of D/C | Factors related to family, marital status, parental role and newborn characteristic increased the psychological problems among NICU mothers. Therefore, planned intervention may reduce these problems. |
| Cohort | * | * | ||||||||||
| Surmeli Onay et al. [20] (2021) | Turkey | CS | 93 | Mother | 30.6 | 28 | 28 | 2.5 | STAI | >40 | <7 days | Tendency of psychological symptoms of NICU mothers were not affect the EBF in preterm infants. |
| Naeem et al. et al. [42] (2019) | Iran | Cohort | 80 | Parents | * | M-47 | 34-36 | * | PPQ | >19 | 3-5 Days after birth | GA was major reason for psychological symptoms NICU parents. Onset psychological symptom earlier in mothers than fathers. fathers indicated delayed onset of PTSD symptoms. |
| F-33 | ||||||||||||
b/w, between; M, mother; F, father; HS, higher secondary; GA, gestational age; NZ, New Zealand; CS, cross-sectional study; NICU, neonatal intensive care unit; HADS, Hospital Anxiety and Depression Scale; EPDS, Edinburgh Postnatal Depression Scale; PPQ, perinatal posttraumatic stress disorder; STAI, State-Trait Anxiety Inventory; ASD, acute stress disorder; SASRQ, Stanford Acute Stress Reaction Questionnaire; SAS, Self-Rating Anxiety Scale; PSS, Parental Stressor Scale; BAI, Beck’s Anxiety Inventory; BDI, Beck Depression Inventory; CES-D, Center for Epidemiological Studies Depression Scale; HAM-A, Hamilton Anxiety Rating Scale; PCL, posttraumatic checklists; DASS, Depression Anxiety and Stress Scale; CESD-10, Center for Epidemiological Studies Depression Scale; PHQ, Patient Health Questionnaire.
Table 3.
CI, confidence interval; STAI, State-Trait Anxiety Inventory; HADS, Hospital Anxiety and Depression Scale; HAM-A, Hamilton Anxiety Rating Scale; BAI, Beck’s Anxiety Inventory; SAS, Self-Rating Anxiety Scale; BDI, Beck Depression Inventory; EPDS, Edinburgh Postnatal Depression Scale; CES-D, Center for Epidemiological Studies Depression Scale; DASS, Depression Anxiety and Stress Scale; CESD-10, Center for Epidemiological Studies Depression Scale; PPQ, perinatal posttraumatic stress disorder; PSS, Parental Stressor Scale; SASRQ, Stanford Acute Stress Reaction Questionnaire; PCL, posttraumatic checklists; ASD, acute stress disorder; NICU, neonatal intensive care unit.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


