Article Contents
| Clin Exp Pediatr > Volume 67(2); 2024 |
|
To the editor,
Micronutrient malnutrition is an emerging health issue among the developing world. Recently, vitamin B12 has been labelled as micronutrient of public health importance. As per Comprehensive National Nutrition Survey findings, 14% of preschool children aged 1–4 years, 17% of school-age children aged 5–9 years and 31% of adolescents aged 10–19 years had vitamin B12 deficiency [1]. Owing to lower concentration of vitamin B12 in vegetarian diet, vegans are at increased risk of developing vitamin B12 deficiency, which runs as a vicious cycle among malnourished vitamin B12 deficient mothers passing it onto their progeny. Thus, highlighting the role of vitamin B12 supplementation among pregnant, lactating females and infants to ensure adequate vitamin B12 stores and intact neuro-developmental outcome. We conducted the present study to estimate the burden and risk factors of vitamin B12 deficiency among admitted anemic children.
This was a cross-sectional study conducted in the Pediatric ward of a tertiary care hospital of northern India over a period of 1 year after seeking approval from the institutional ethics committee (SRMSIMS/2017-18/106). After taking written informed consent from the parents/caregivers, children aged 6 months to 18 years, with hemoglobin levels below age specific values were included in the study [2]. Children with chronic illnesses like tuberculosis, cancer or immunocompromised states, history of blood transfusion in preceding 6 weeks prior to admission, history of intake of vitamin B12 supplements were excluded. Anemia, leucopenia and thrombocytopenia were defined as per the standard guidelines [3,4]. Deficiency of vitamin B12 was considered when vitamin B12 levels were less than 150 pg/mL [4]. Demographic details, clinical history and examination of the enrolled children were recorded in preformed proforma. Vitamin B12 assay was done using chemiluminescence technique.
Statistical tests applied for qualitative data and quantitative data were chi square test and student t test respectively, using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) [5]. P value less than 0.05 was considered significant
During the study period, 145 cases of anemia were admitted, of which 30 children had history of hematinics intake, 12 children received blood transfusion, 3 children were diagnosed with hematological malignancies and parents of 15 children did not give consent for participation into this study. Therefore 85 children were included in the final analysis. Of the 85 anemic children, 40 (47%) had vitamin B12 deficiency. As per this study, 32.5% of infants aged 6–12 months, 22.5% of toddlers aged 1–3 years, 5% of preschool children aged 3–6 years, 17.5% of children aged 6–12 years, and 22.5% of adolescents aged 12–18 years had vitamin B12 deficiency.
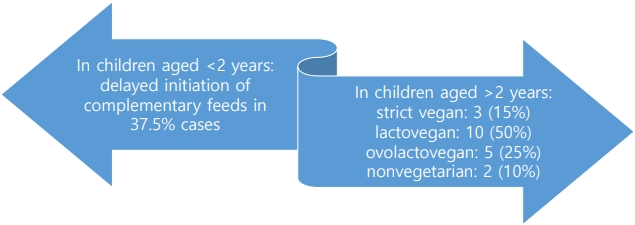
India is facing the threat of micronutrient malnutrition as the silent epidemic. We evaluated 85 anemic children aged 6 months to 18 years, during the study period. As per the findings from our study, the average value of vitamin B12 level obtained among infants aged 6–12 months, children aged 1–3 years, 3–6 years, 6–12 years, and 12–18 years was 223.7, 314.4, 284.5, 413.3, and 343.4 pg/mL, respectively. Vitamin B12 deficiency was reported in 47% cases, reasons for such high prevalence could be a hospital-based study receiving relatively more sick and morbid children, thereby unmasking the underlying micronutrient deficiencies in at risk population. The prevalence of vitamin B12 deficiency is variable in other hospital-based studies reported from India, ranging from 16.66% to 64.8%.[6,7]. This difference could be attributed to variation in socio-cultural beliefs and feeding habits. In a multicenter cross-sectional study on urban school going children by Awasthi et al, vitamin B12 deficiency was found to be 33.4%.8) In the present study vitamin B12 deficiency was found most commonly in the age group 6 months to 3 years (55%) followed by 12 to 18 years (22.5%), 6 years to 12 years (17.5%), and 3 years to 6 years (5%). Reasons for higher prevalence of cobalamin deficiency in infants and toddlers seen in our study (Fig. 1) are manifold. Exclusive breastfeeding by malnourished cobalamin deficient mothers confers additional risk of developing vitamin B12 deficiency in their nursing infants Delayed initiation of complementary feeding and inadequate bovine milk intake further limit dietary intake of infants aged 6 months and above children. The observations serve as an alarming call to action, emphasizing on vitamin B12 supplementation in expectant and lactating mothers as we practice with regards to folic acid intake. Bimodal age distribution of vitamin B12 deficiency was observed in our study, adolescence is a phase of rapid growth, thus necessitating increased micronutrients intake.
India is a country of great socio-cultural diversity with varying dietary beliefs and practices, predominantly being the vegan diet followers. Strict vegetarians, or vegans, eat plant foods and reject all animal products—meat, poultry, fish, eggs, dairy products. Those who also eat dairy products are called lacto vegetarians. Vegetarians who eat both dairy and eggs are called lacto-ovo vegetarians [9]. Vitamin B12 deficiency was correlated with vegetarian diet in 65% cases, in our study (Fig. 1). An striking observation of more deficient cases in lacto-vegan group (50%) as compared to pure vegans (15%) was made in this study. It could be due to consumption of lesser quantity or diluted bovine milk. Previous studies have analyzed children till 5 years of age, while the present study evaluated adolescent age group in addition to infants and toddlers bringing out more clarity.
Micronutrient deficiency is aptly labelled as “Hidden hunger,” which can occur without a deficit in energy intake as a result of consuming an energy-dense, but nutrient-poor diet [10]. In accordance with this, nutritional status was found normal in 62.5% cases with decreased vitamin B12 in the present study (Table 1). Active screening for vitamin B12 deficiency needs to be undertaken by clinicians even if the growth parameters remain normal.
Our study faced several limitations. Being a hospital-based study, the findings could not be generalized over a large population. Maternal vitamin B12 levels were not studied and correlated with their vitamin B12 deficient infants. Assessment of novel biomarkers like homocysteine, methylmalonic acid, holoTc (biologically active form of vitamin B12 in plasma) could have been more valid and confirmatory in diagnosing vitamin B12 deficiency.
Acknowledgments
The author(s) acknowledge the contribution of faculty and residents of Department of Pathology, SRMSIMS, Bareilly. Special thanks to participating children and their parents/caregivers for their willingness to participate in the study.
Table 1.
Correlation between nutritional status and vitamin B12 deficiency in anemic children
References
1. Ministry of Health and Family Welfare; Government of India; UNICEF and Population Council. Comprehensive National Nutrition Survey 2016-2018. New Delhi (India): Ministry of Health and Family Welfare, Government of India, 2019.
2. Kliegman RM, Stanton BF, St. Geme JW III, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th International ed. Philadelphia (PA): Elsevier, 2016:2310.
3. Kliegman RM, Stanton BF, St. Geme JW III, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th International ed. Philadelphia (PA): Elsevier, 2016:3466.
4. Sachdeva A. Practical pediatric hematology. 2nd ed. New Delhi (India): Jaypee; 2015:23.
5. Mahajan BK. Methods in biostatistics. 7th ed. New Delhi (India): Jaypee; 1997:85.
6. Kumar K, Parihar RK, Sharma P. Prevalence and clinic hematological profile of vitamin B12 deficiency associated megaloblastic anemia in children of Jammu region - a hospital based observational study. Panacea J Med Sci 2022;12:524-7.

7. Umasanker S, Bhakat R, Mehta S, Rathaur VK, Verma PK, Bhat NK, et al. Vitamin B12 deficiency in children from Northern India: time to reconsider nutritional handicaps. J Family Med Prim Care 2020;9:4985-91.



8. Awasthi S, Kumar D, Mahdi AA, Agarwal GG, Pandey AK, Parveen H, et al. Prevalence of specific micronutrient deficiencies in urban school going children and adolescence of India: a multicenter cross-sectional study. PLoS One 2022;17:e0267003.



9. Digging a vegetarian diet: plant-based eating can reap rewards [Internet]. Bethesda (MD): National Institutes of Health; 2012 [cited 2023 Nov 6]. Available from https://newsinhealth.nih. gov/2012/07/digging-vegetarian-diet.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


