Article Contents
| Clin Exp Pediatr > Volume 66(6); 2023 |
|
Abstract
Background
Preterm babies are born before completion of 37 weeks of gestational. Compared to term neonates, preterm babies are difficult to adjust to extra uterine life and 15 million babies (11%) born before 37 weeks of gestation.
Purpose
This systematic review and meta-analysis aimed to evaluate evidence concerning the efficacy of body position on gastric residual volume among preterm infants.
Methods
We conducted a systematic search of studies trials published in PubMed, MEDLINE, CINHAL, Clinical Key, Cochrane Library, and Google scholar. Two authors independently appraised the selected randomized control trials for evaluating the effectiveness of body position on gastric emptying. This systematic review and meta-analysis was conducted based on the Cochrane risk bias assessment tool using Revman 5.3 software.
Results
On assessment this systematic review and meta-analysis comprised 289 preterm infants from the included 7 trials, with the sample size ranging from 20–63. The gestational age ranged from 28–37 weeks, with an average gestational age of 31.7 weeks. The age of the participants postnatal ranged from 6.6 days to 33.4 days, with an average age of 18±6 days. The weight of the participants during data collection ranged from 1,272–2,683 g, with an average of 1,795 g.
Graphical abstract
“Preterm birth” describes all live births occurring before 37 weeks’ gestation from the first day of the last menstrual period [1]. Globally, 15 million infants are born preterm for a global preterm birth rate of 11% [2]. With compromised anatomical and functional capabilities and premature nervous function of the gastrointestinal system, preterm babies experience digestive issues [3,4]. Thus, proper enteral nutrition must be established for preterm infants to decrease their mortality rate and shorten their hospital stay [5,6]. Gavage feeding, which is initiated soon after birth in preterm infants [7], intends to provide energy of 110–135 kcal/kg as well as protein of 4–4.5 g/kg for those weighing less than 1 kg and 3.5–4 g/kg for those weighing 1–1.8 kg [8].
Gavage feeding/enteral nutrition involves providing breast milk or formula directly into the baby’s stomach via a nasogastric tube. Gavage feeding is indicated in babies who are premature and too small or weak to suck effectively from the breast or bottle, those who cannot coordinate their sucking and swallowing, and those born with anomalies of the throat, esophagus, heart, or lungs [9].
The nutritional status of preterm infants is measured based on the gastric residual volume, the amount of food residue from the last feeding to that at the start of the next feeding. The residual gastric volume is usually measured before feeding and includes an analysis of the gastric acid and enzymes. Gastric emptying depends on numerous factors, such as milk type (mother milk or milk powder) and volume, physical condition, and postfeeding position [10].
Preterm infants are most commonly placed in supine, prone, right lateral, or left lateral positions after feeding for varying durations of time. Each position has its advantages and disadvantages. The prone position increases arterial oxygen saturation, decreases regurgitation, and reduces apnea. However, preterm infants in the prone position are susceptible to sudden infant death syndrome and delayed muscular development. A few studies have reported that placing the infant in a prone position for an hour after feeding attenuates gastric residual volume and regurgitation [11,12]. This finding was reiterated by Chen et al. [13], who reported that the gastric residual volume was lower among infants placed in the prone versus right lateral position. In contrast, Cohen et al. [14] reported that gastric residual volume was not significantly different at 3 hours after feeding among infants placed in the prone, supine, right lateral, and left lateral positions. Hussein reported that at 1 hour after feeding, placing the infant in the right lateral and supine positions did not effectively lower the gastric residual volume [15].
Despite years of research on preterm infants and enteral nutrition, consensus is lacking on the appropriate position for preterm infants after feeding to reduce gastric residual volume. With the growing need for reliable evidence of the best postfeeding position for preterm infants, here we conducted a systematic review and meta-analysis to analyze the effect of position on gastric residual volume among premature infants after gavage feeding.
This systematic review and meta-analysis was registered in PROSPERO (National Institute for Health Research-International prospective register of systematic reviews) and assigned the number CRD42021245833.
This systematic review and meta-analysis aimed to evaluate evidence concerning the efficacy of body position on gastric residual volume among preterm infants.
The quantitative systematic review and meta-analysis evaluated the efficacy of body position on gastric residual volume among preterm infants. The review was performed based on Cochrane collaboration guidelines [16] and reported according to the Preferred Reporting Items for Systematic Reviews and MetaAnalysis statement [17].
The search scheme was developed using the search keywords connected to PICO (population or patient, intervention, comparator or control, and outcome). Two authors independently searched the MEDLINE, Clinical Key, Cumulative Index to Nursing and Allied Health Literature, Cochrane Library, and Google Scholar databases without limitations imposed on study period. Studies that employed an experimental design to evaluate the effectiveness of position on gastric residual volume among preterm infants were retrieved for further analysis.
Medical subject headings terms used during the online search were “newborn” OR “neonate” OR “preterm” AND “left lateral position” OR “right lateral position” OR “prone position” OR “supine position” AND “gastric empty” OR “residual volume” OR “gastric residual volume.” We manually searched the reference lists of the included articles for additional resources. Duplicate records were removed after title and abstract screening, and the remaining original full-text articles were screened against the inclusion criteria.
The participants of this review were preterm infants (born before 37 weeks’ gestation) admitted to the neonatology department and randomly allocated to the treatment or control group.
Preterm infants in the experimental group were placed in the supine/prone/right lateral/left lateral body position after feeding.
Preterm infants in the control group were placed in a supine/ prone/right lateral/left lateral body position after the feeding, a body position that differed from the preterm infants in the experimental group.
Gastric residual volume was the primary outcome of this systematic review and meta-analysis.
Regarding the nature of the subjects, many authors failed to report the component variables. Noninvasive interventions, such as postfeeding postures, are vital elements in enhancing feeding tolerance and mechanical functions of the gastrointestinal tract among preterm infants. For instance, we set the minimum inclusion criteria during study selection process.
Studies in which the participants were preterm infants, gastric residual volume was the primary outcome variable, studies that evaluated the efficacy of body position on gastric residual volume, and studies published in English were selected.
The search scheme retrieved 654 studies from various databases and 3 from printed materials. During the initial screening, 193 duplicate articles were excluded. The remaining 461 articles were screened, of which 440 were removed after title and abstract review, as they did not meet the predetermined inclusion criteria of the review. The remaining 21 articles were read fully and screened for eligibility; 14 were removed for not reporting sample sizes of the intervention versus control groups, not mentioning whether random allocation was used, or not specifying primary outcomes or statistical information. Finally, 7 articles [13,14,18-22] were included in the narrative synthesis and meta-analysis. The study selection process is illustrated in Fig. 1.
Two authors independently extracted data from the 7 articles, and any disagreement between the first 2 authors was settled by discussion with the third author. The data extraction process captured the following: author name, country, year of publication, study design, sample size, body position, infant weight, sex, gestational age, and outcome measures.
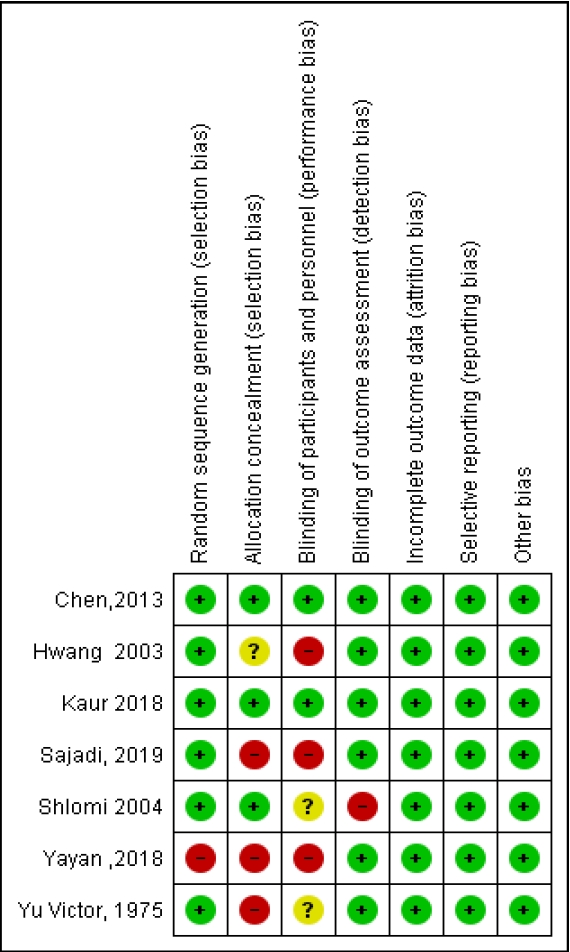
Study quality was assessed by Cochrane’s collaboration’s risk of bias assessment tool, which assesses random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data, and selective reporting [23]. The studies were appraised and categorized according to the risk of bias (low, high, and unclear). The risk of bias assessment is shown in Fig. 2.
The primary outcome of this systematic review and meta-analysis was to compare the gastric residual volume of preterm infants in the right lateral, left lateral, prone, and supine positions.
This meta-analysis was performed after pooling the findings from the included studies. The effects of body position on gastric residual volume were calculated using a random-effects model to compute the weighted mean differences and standardized mean differences between the experimental and control groups. The standardized mean difference was calculated after adjusting for standard deviation. The study heterogeneity was analyzed using I2 value. The chi-square test was used for the subgroup analysis. We used RevMan software v5.3 for computing and analyzing the data. To provide quality and strength of evidence, the Grading of Recommendations, Assessment, Development and Evaluation approach and guidelines were adopted [24].
This systematic review and meta-analysis comprised 289 preterm infants from the included 7 trials with sample sizes of 20–63. Gestational age was 28–37 weeks (mean, 31.7 weeks). Participant ages were 6.6–33.4 days (mean, 18±6 days). Participant weights were 1,272–2,683 g (mean, 1,795 g). All included studies but one adopted a random crossover design [19]. Seven trials were included to assess the efficacy of body position on gastric residual volume (Table 1). The results of the included studies were analyzed and are shown as forest plots.
On assessment of the gastric residual volume 30 minutes after the feeding, the pooled data revealed that the probability of gastric residual volume in the right lateral position was lower than that in the supine position (standard mean of the difference, -1.25; 95% confidence interval, -2.47 to -0.03; P=0.04; I2=90%). Similarly, on comparing the gastric residual volume in the right lateral position with the left lateral position at 30 minutes after the feeding, the gastric residual volume was lower in the right lateral position (-1.17 [-2.37 to 0.02]; P=0.05; I2=88%), but this was not statistically significant. However, on comparing the right lateral position with the prone position at 30 minutes after the feeding, no statistically significant difference in gastric residual volume was found (-0.27; [-1.39 to -0.86]; P=0.64; I2=88%). The effect of studies on body position 30 minutes after a feeding on gastric residual volume is depicted in Fig. 3.
Comparison of the gastric residual volume 30 minutes after the feeding in the prone versus left lateral (-0.99 [-1.37 to -0.61], P=0.00001; I2=0%) and supine (1.11 [0.59 to 1.64]; P<0.0001; I2=59%) positions revealed that the gastric residual volume was lower in the prone position. Similarly, gastric residual volume was lesser at 30 minutes after the feed in the supine versus left lateral position (-0.07 [-0.40 to 0.26]; P=0.68; I2=1%), but the difference was not statistically significant. The overall study heterogeneity was (-0.28 [-0.80 to 0.23]; P<0.00001; I2=92%), and the differences on the subgroup analysis were statistically significant (χ2=46.30; degrees of freedom [df]=5; P<0.00001). The effect of body position at 30 minutes after feeding on residual gastric volume is depicted in Fig. 3.
On evaluation of the efficiency of the body position in gastric residual volume at 60 minutes after the feeding, the pooled data indicated that the probability of gastric residual volume was lower in the right lateral than left lateral (-0.85 [-1.72 to 0.02]; P=0.05; I2=87%), supine (-0.98; -2.35 to 0.38; P=0.16; I2=94%), and prone (-0.07 [-0.36 to 0.22]; P=0.62; I2=0%) positions, respectively. Comparison of the gastric residual volume at 60 minutes after the feeding in the supine versus prone (1.07 [0.05 to 2.09]; P=0.04; I2=91%) and supine versus left lateral (0.13 [-0.44 to 0.69]; P=0.66; I2=71%) positions, the supine position was not efficient at reducing the gastric residual volume. However, the overall study heterogeneity was (-0.18 [-0.65 to 0.29); P<0.00001; I2=93%), and the subgroup analysis was statistically significant (χ2=12.68; df=5; P=0.46). The effect of body position at 60 minutes after a feeding on residual gastric volume is depicted in Fig. 4.
Similarly, we evaluated the effect of body position on gastric residual volume at 120 minutes after a feeding. The pooled data indicated that the probability of gastric residual volume was lower in the right lateral than left lateral (-0.74 [-1.46 to -0.02]; P=0.04; I2=71%) and supine (-0.25 [-0.60 to 0.11]; P=0.18; I2=00%) positions. However, at 120 minutes after a feeding, the prone position significantly reduced gastric residual volume (0.78 [-0.19 to 1.38]; P=0.010; I2=77%). Similarly, the prone position was more effective than the supine position (1.03 [0.40 to 1.65]; P=0.001; I2=67%) or the left lateral position (-1.37 [-3.05 to 0.32]; P=0.11; I2=94%) at reducing the gastric residual volume. The overall study heterogeneity was (-0.01 [-0.55 to 0.53]; P<0.00001; I2=93%), and the subgroup analysis of different positions revealed a statistically significant difference (χ2=27.08; df=5; P<0.0001). The effect of body position at 60 minutes after a feeding on residual gastric volume is depicted in Fig. 5.
When evaluating the efficiency of body position on gastric residual volume at 180 minutes after a feed, the pooled data indicated that the probability of gastric residual volume in the right lateral position was lower than that in the left lateral (-0.62 [-1.43 to 0.18]; P=0.13; I2=88%), supine (-0.41 [-1.15 to 0.33]; P=0.27; I2=83%), and prone (-0.15 [-0.43 to 0.14]; P=0.31; I2=12%) positions, respectively. The prone position reduced the gastric residual volume versus the supine position (0.42 [-0.35 to 1.18]; P=0.29; I2=84%), the supine position reduced the gastric residual volume versus the left lateral position (-0.04 [-0.45 to 0.36]; P=0.83; I2=47%), and the prone position reduced the gastric residual volume versus the left lateral position (-0.55 [-1.37 to 0.27; P=0.19; I2=88%). The overall study heterogeneity was (-0.25 [-0.53 to 0.03]; P<0.00001; I2=83%). The subgroup analysis findings were not statistically significant (χ2=5.11; df=5; P=0.40). The effect of body position at 180 min after a feeding on gastric residual volume is depicted in Fig. 6.
As few trials were included in the systematic review and meta-analysis, the potential for publication bias was not assessed.
The initiation of prompt nutrition significantly influences the short- and long-term health of preterm infants. Halting or delaying enteral feeding may result in extrauterine growth restriction, a known predisposing factor for poor neurodevelopmental and growth outcomes in preterm and very low birth weight infants.
The gastric residual volume of preterm infants is often evaluated and purported as an index of feeding intolerance and necrotizing enterocolitis among those fed enterally [25]. Although gastric residual volume is regularly evaluated to plan future feedings [26], there is a scarcity of scientific evidence of this practice [27]; moreover, it can be harmful [28]. Numerous factors influence (antenatal steroid therapy [29]) and delay (formula milk) [30] diseases such as hypoxemia [31], sepsis, hypotension, and acute respiratory distress [25].
Enteral feeding timing, type, and mode influences gastric emptying. The prompt initiation of enteral nutrition enhances duodenal motor activity [32]. Compared to formula, breast milk results in faster gastric emptying in premature infants [33]. Ewer and Yu [34] found that the fortification of breast milk results in delayed gastric emptying. Breast feeding is the ideal and easily digestible nutrition for newborns, keeping them healthy and protecting them against allergies, sickness, obesity, and infectious diseases. Although breast milk is the preferred source of enteral nutrition [32], fortification is sometimes warranted to meet the neonate’s nutritional requirements. Although breast milk supplies all of the growth needs of more mature preterm (33–36 weeks’ gestation), less mature infants (those at 28–32 weeks’ gestation) failed to achieve adequate growth rates compared to infants with a high protein intake [35]. A high protein intake can have a detrimental effect on a child’s intelligence quotient [36]. However, no feeding tolerance was found in terms of the fortification of breast milk by Gathwala et al. [37]. Continuously infused enteral feeding tends to accelerate gastric emptying by enhancing the duodenal motor response compared to bolus feeding [38]. In contrast, a Cochrane review found inadequate evidence to underpin the use of continuous enteral feeding versus bolus feeding [39].
The early establishment of breast feeding [40] and appropriate body positions favor the normal milestone development of preterm infants. Body position affects the gastric emptying rate and, hence, residual gastric volume. Increased residual gastric volume results in increased gastric distension and gastroesophageal reflux [41].
Regarding systematic bias, we excluded many sound studies for various reasons, such as advanced gestational age (>37 weeks), preterm infant sickness, extremely low birth weight, and use of formula or parenteral nutrition. However, the findings of this systematic review and meta-analysis indicate that appropriate positioning of preterm infants improves gastric emptying. Our review found that the right lateral and prone positions significantly reduced gastric residual volume in preterm infants. Several studies have reported that the prone versus supine position could help reduce gastric residual volume [18,19,22], while few studies reported that the right lateral position is more effective at reducing gastric residual volume [42]. The prone and right lateral positions had the lowest gastric residue and highest probability of nutrient absorption [12,19]. The effect of body position on gastric residue varied with time after the feeding [43].
Gastric residue is an indirect marker of feed tolerance/intolerance. We agree that it is difficult to differentiate between pathological and physiological conditions. Gastric residues are the simplest and most common surrogate marker for feeding intolerance in day-to-day neonatal practice. There is an urgent need for evidence-based guidelines on the specific position to be adopted after a feeding to decrease the gastric residual volume among preterm infants. An appropriate position would reduce the residual gastric volume and promote preterm development.
In conclusion, this systematic review and meta-analysis found that preterm infants placed in the right lateral and prone positions after a feeding had reduced gastric residual volume compared to those placed in the supine and left lateral positions. Preterm infants placed in right lateral or prone position for the initial 30–60 minutes after a feeding had significantly reduced gastric residual volumes.
Our meta-analysis findings were based on 7 comparative randomized crossover studies; all but one reported using randomization. Due to the nature of the subjects and study topic, we could not analyze the component variables and lactation factors. And finally, the majority of the included randomized controlled trials did not report the use of study blinding or the clinical registration number.
Globally, this is the first systematic review and meta-analysis on this topic, and the authors strongly believe that its findings provide the highest level of evidence. Furthermore, this systematic review and meta-analysis as well as future prospective double-blinded clinical trials will help build universal clinical guidelines.
Footnotes
Acknowledgments
We are extremely thankful to Dr. Shashidar YN for proofreading and editing this review.
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis)–compliant flow diagram of the study selection process.
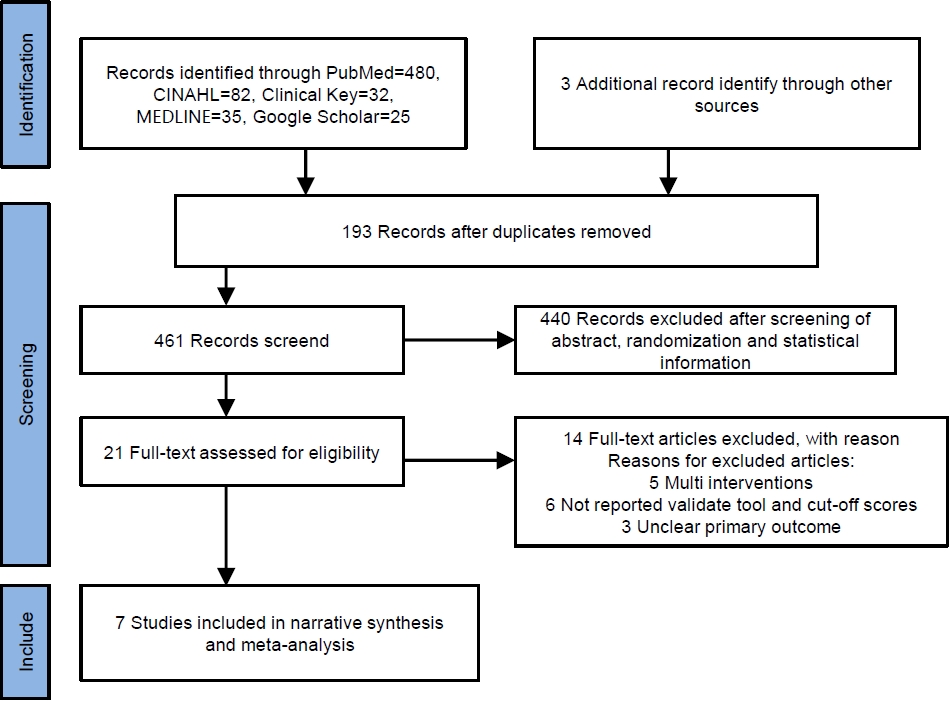
Fig. 3.
Effect of body position on gastric residual volume at 30 minutes after a feeding. SD, standard deviation; CI, confidence interval; df , degrees of freedom.
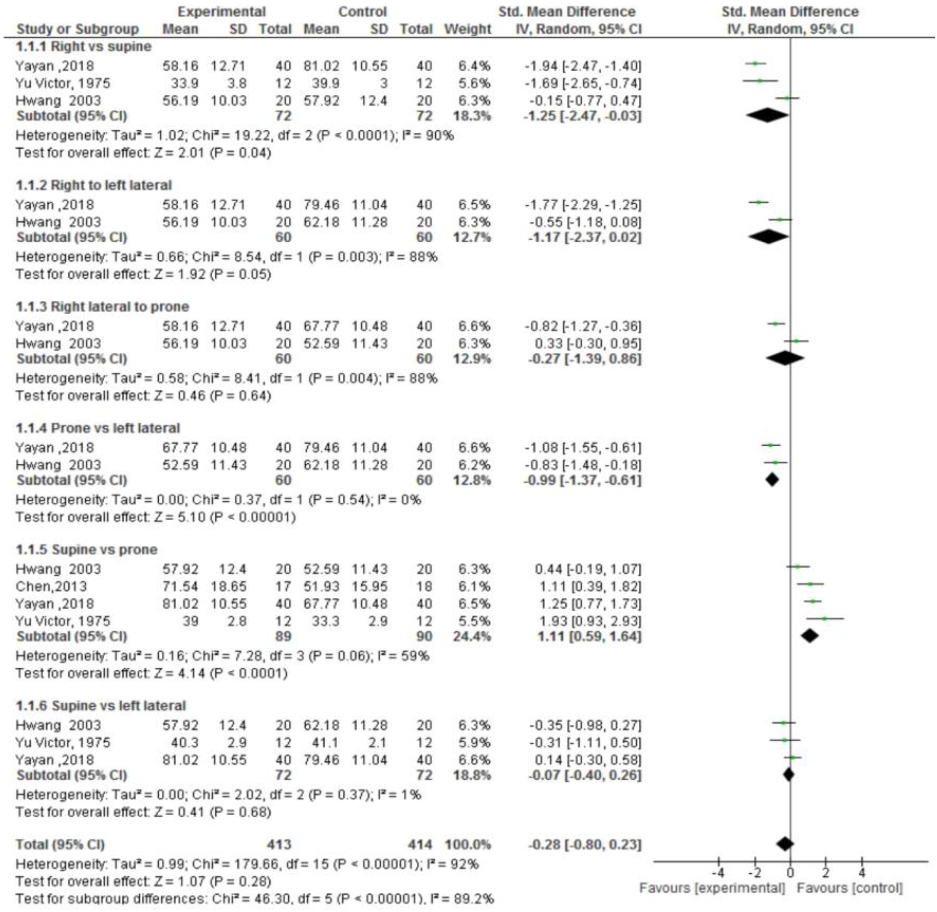
Fig. 4.
Effect of body position on gastric residual volume at 60 minutes after a feeding. SD, standard deviation; CI, confidence interval; df , degrees of freedom.
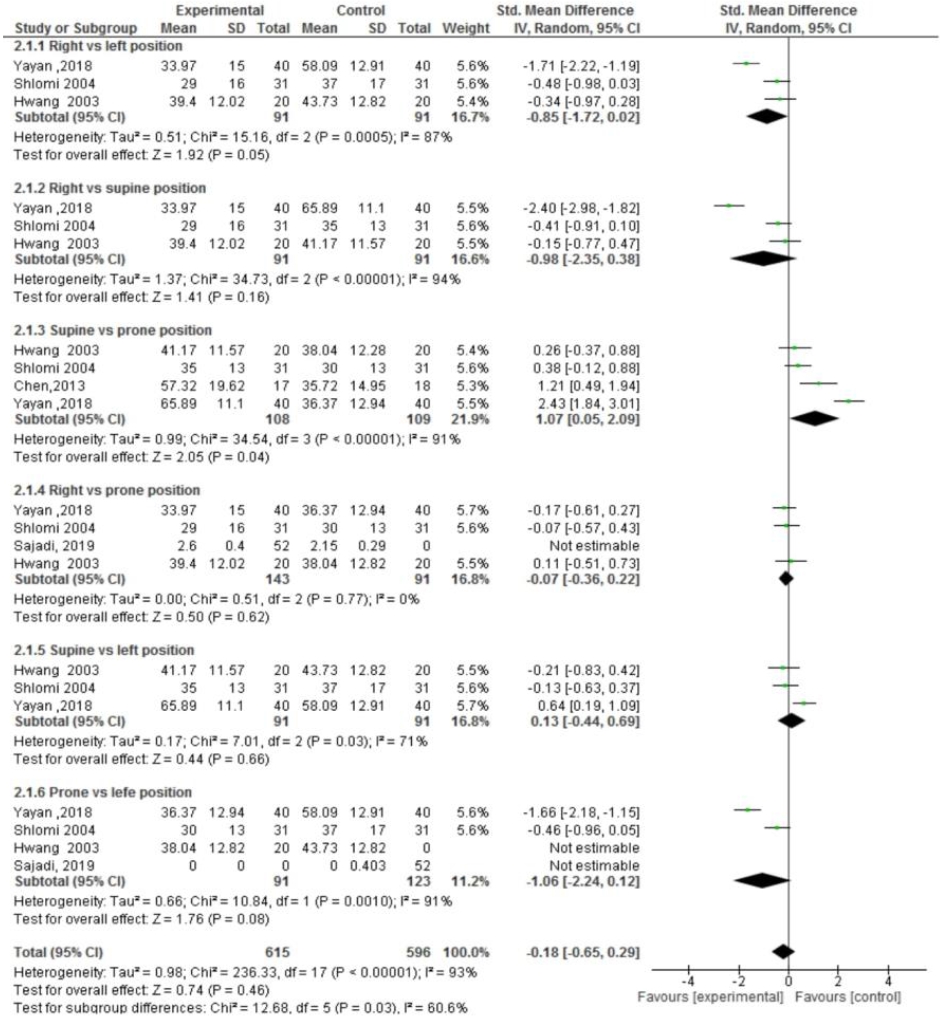
Fig. 5.
Effect of body position on gastric residual volume at 120 minutes after a feeding. SD, standard deviation; CI, confidence interval; df , degrees of freedom.
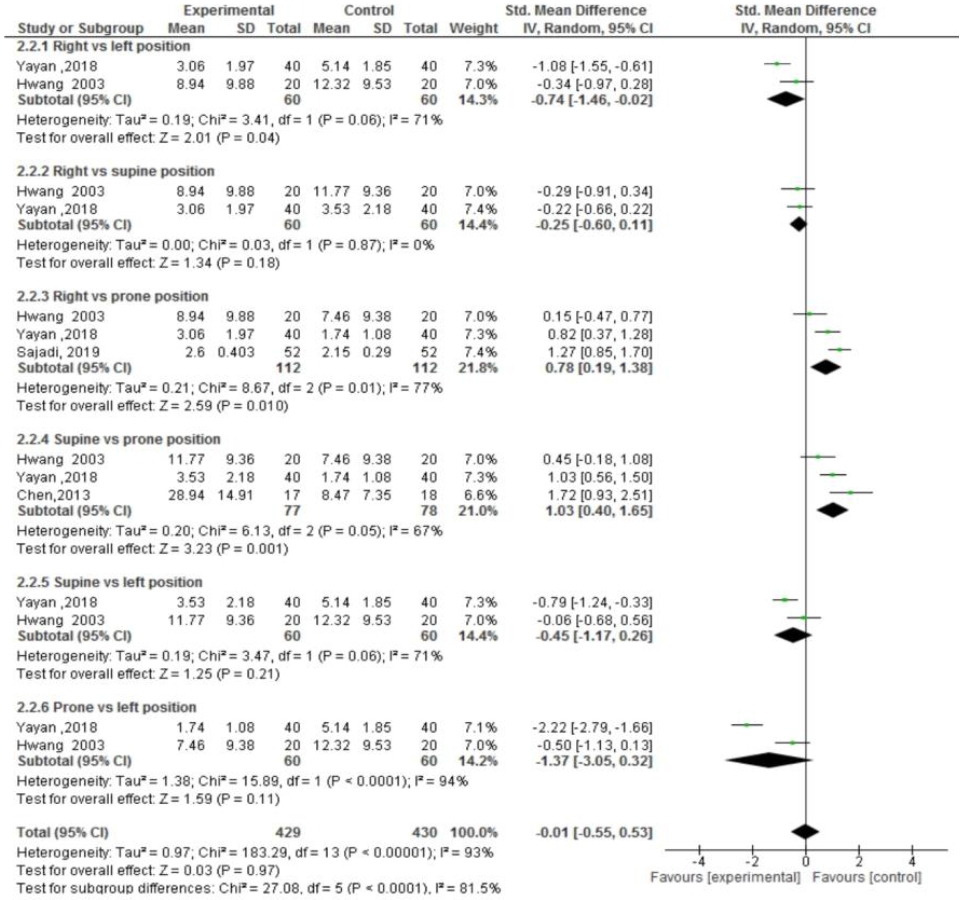
Fig. 6.
Effect of body position on gastric residual volume at 180 minutes after a feeding. SD, standard deviation; CI, confidence interval; df , degrees of freedom.
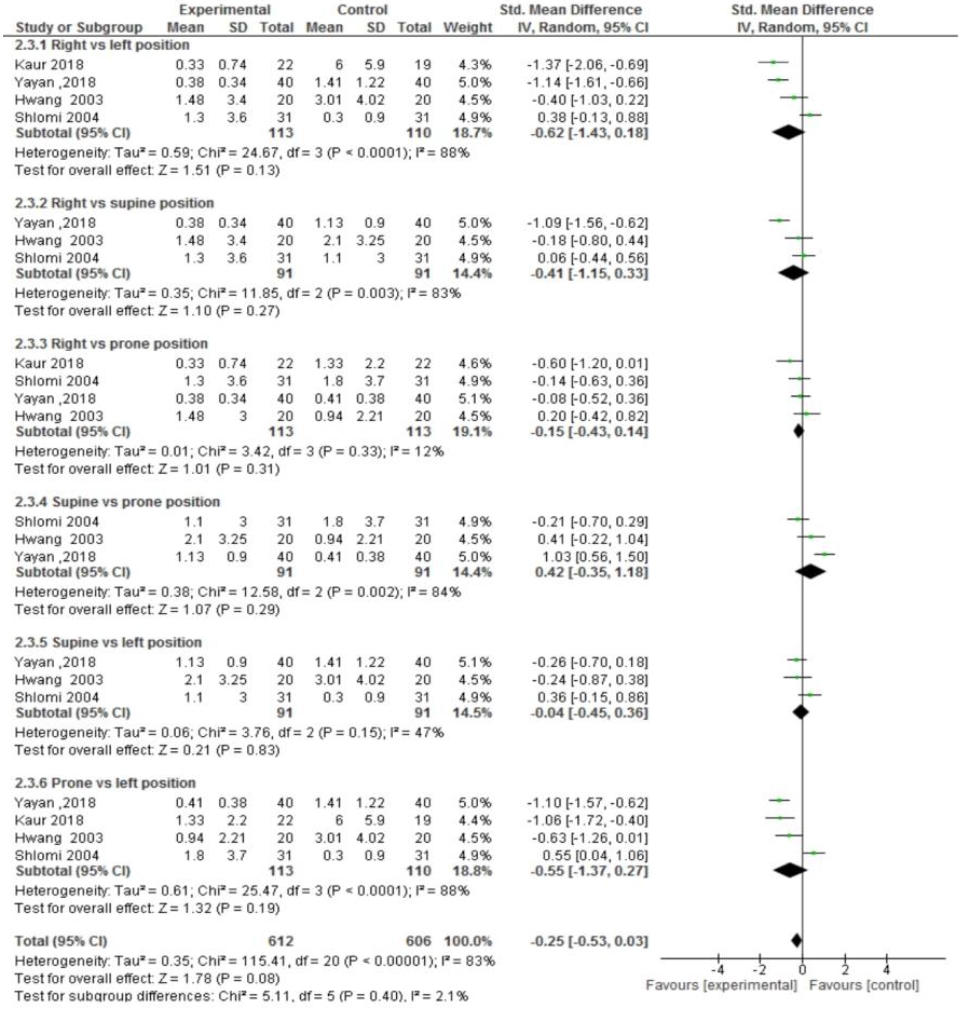
Table 1.
Summary of study characteristics
| Study | Type of study design and clinical trial number | Sample size | Sex, male:female | Postnatal age, mean±SD | Weight of babies (g) | Average gestational age (wk) |
Intervention |
Time interval (min) | Outcome measures | |
|---|---|---|---|---|---|---|---|---|---|---|
| Type of body position in intervention group | Control | |||||||||
| Victor [18] 1975 | RCT (cross over random design) | 48 | - | 12.3±1.6 | 2,683 | 37 | After feeding, newborn was placed randomly to supine, prone, left lateral and right lateral position. | Compared the gastric residual volume in all 4 positions. | 30 | Gastric residual volume was lower in prone and right-lateral positions. |
| Sajadi et al. [20] 2019 | RCT (cross over design) (IRCT 2017203037731N1) | 52 | 24:28 | 10.38±9.6 | 1,902±53 | 28-36 | After feeding, preterm babies placed in prone and right lateral positions | Compared gastric residual volume at 30, 60, 90, and 120 minutes. | 30–120 | The mean gastric residual volume was lower in prone position (P=0.001). |
| Birth weight | ||||||||||
| 1,825.4±568.2 | ||||||||||
| Hwang et al. [21] 2003 | RCT (repeated measures design) | 20 | 10:10 | 31.75±22.56 | 1934.25±203.84 | 31.90±2.47 | Randomly assigned to prone, left lateral, supine, right anterior oblique and right lateral position. | Compared the gastric residual volume in all 4 positions. | 30–180 | The right anterior oblique or prone position lowered the gastric residual volume |
| Birth weight | ||||||||||
| 1,634.75±178.59 | ||||||||||
| Yayan et al. [19] 2018 | A semiexperimental study (number and date: 2015/23 | 40 | 23:17 | - | 1,420.56±283.47 | 30.42±3.62 | Preterm infants were sequentially placed in 4 positions and feed given before change in each position. | The gastric residual measured at 30, 60, 120, and 180 minutes after each feeding. | 30–180 | Right lateral and prone position lowered the gastric residual volume. |
| Birth weight | ||||||||||
| 1,231.2–452.3 | ||||||||||
| Kaur et al. [22] 2018 | RCT (randomized cross trial design) (CTRI/2015/06/0058 95) | 63: left lateral position (n=19), right lateral position (n=22), prone position (n =22) | 39:24 | 6.6±4.4 | 1,272±307 | 31±2 | Newborns were randomly assigned to 3 nursing positions i.e., left lateral, right lateral, and prone position in double cross over fashion for 3 consecutive days. | Compared gastric residual volume in 3 positions. | 120 | Gastric residual volume reduced in prone and right lateral position. |
| Total 4 feed given in same position, then the average residual volume was checked. | ||||||||||
| Chen et al. [13] 2013 | RCT (cross over) | 35 | 17:18 | 31.64±2.64 | 1,269-1,308±376 | 29.76±2.4 | After feed neonates were placed in 3 different positions. | Compared gastric residual volume at 30, 60, 90, 120, and150 minutes. | 60–180 | Prone position subsequently reduces residual volume first 30-minute postfeeding. |
| No. C07172 | ||||||||||
| Cohen et al. [14] 2004 | RCT (prospective cross over) | 31 | - | 33.4±1.5 | 1,478±238 | 30.5±1.8 | After feed neonates were randomly assigned to different positions. | Compared gastric residual volume at one and 3 hours. | 60 & 80 | Gastric residuals decreased in right lateral and prone position. |
| Study approved from Review board for human subject (Lis Maternity Hospital, Tel Aviv) | Average | 1,795 | 31.7 | |||||||
| 15.57 days | ||||||||||
| 18±6 days | ||||||||||
References
1. Quinn JA, Munoz FM, Gonik B, Frau L, Cutland C, Mallett-Moore T, et al. Preterm birth: case definition & guidelines for data collection, analysis, and presentation of immunisation safety data. Vaccine 2016;34:6047–56.



3. Riezzo G, Indrio F, Montagna O, Tripaldi C, Laforgia N, Chiloiro M, et al. Gastric electrical activity and gastric emptying in term and preterm newborns. Neurogastroenterol Motil 2000;12:223–9.


4. Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr 2003;92:721–7.


6. Hari AB. Approach to enteral nutrition in the premature infant - UpToDate [Internet]. [cited 2021 Sep 17]. Available from: https://www.uptodate.com/contents/approach-to-enteral-nutrition-in-the-premature-infant.
7. Embleton ND. When should enteral feeds be started in preterm infants? Paediatr Child Health 2008;18:200–1.

8. Enteral feeding of preterm infants [Internet]. [cited 2021 Sep 17]. Available from: https://www.clinicalguidelines.scot.nhs.uk/nhsggc-paediatric-clinical-guidelines/nhsggc-guidelines/neonatology/enteral-feeding-of-preterm-infants/.
9. Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol 2014;20:8505–24.



10. Yasuda H, Kondo N, Yamamoto R, Asami S, Abe T, Tsujimoto H, et al. Monitoring of gastric residual volume during enteral nutrition. Cochrane Database Syst Rev 2021;9:CD013335.



11. Picheansathian W, Woragidpoonpol P, Baosoung C. Positioning of preterm infants for optimal physiological development: a systematic review. JBI Libr Syst Rev 2009;7:224–59.


12. Khatony A, Abdi A, Karimi B, Aghaei A, Brojeni HS. The effects of position on gastric residual volume of premature infants in NICU. Ital J Pediatr 2019;45:6.




13. Chen SS, Tzeng YL, Gau BS, Kuo PC, Chen JY. Effects of prone and supine positioning on gastric residuals in preterm infants: a time series with cross-over study. Int J Nurs Stud 2013;50:1459–67.


14. Cohen S, Mandel D, Mimouni FB, Solovkin L, Dollberg S. Gastric residual in growing preterm infants: effect of body position. Am J Perinatol 2004;21:163–6.


15. Hussein HA. The difference between right side and semi recumbent positions after feeding on gastric residual volume among infants. J Am Sci 2012;8:127–32.
16. Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions [Internet]. Cochrane Training [cited 2021 Sep 17]. Available from: https://training.cochrane.org/handbook/current.
17. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1.




18. Victor YH. Effect of body position on gastric emptying in the neonate. Arch Dis Child 1975;50:500–4.



19. Yayan EH, Kucukoglu S, Dag YS, Karsavuran Boyraz N. Does the postfeeding position affect gastric residue in preterm infants? Breastfeed Med 2018;13:438–43.


20. Sajadi M, Akbari M, Alinejad S, Khosravi S. Comparison of effect of prone and right lateral positions on gastric residual volume in preterm newborns. Iran J Neonatol 2019;10:55–60.
21. Hwang SK, Ju HO, Kim YS, Lee HZ, Kim YH. Effects of body position and time after feeding on gastric residuals in LBW infants. Taehan Kanho Hakhoe Chi 2003;33:488–94.



22. Kaur V, Kaur R, Saini SS. three nursing positions for reducing gastric residuals in preterm neonates: a randomized crossover trial. Indian Pediatr 2018;55:568–72.



23. Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing risk of bias in a randomized trial [Internet]. Cochrane Training [cited 2021 Sep 17]. Available from: https://training.cochrane.org/handbook/current/chapter-08.
24. Schünemann HJ, Higgins JPT, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘summary of findings’ tables and grading the certainty of the evidence [Internet]. Cochrane Training [cited 2021 Sep 17]. Available from: https://training.cochrane.org/handbook/current/chapter-14.
25. Bertino E, Giuliani F, Prandi G, Coscia A, Martano C, Fabris C. Necrotizing enterocolitis: risk factor analysis and role of gastric residuals in very low birth weight infants. J Pediatr Gastroenterol Nutr 2009;48:437–42.


26. Krishnamurthy S, Gupta P, Debnath S, Gomber S. Slow versus rapid enteral feeding advancement in preterm newborn infants 1000-1499 g: a randomized controlled trial. Acta Paediatr 2010;99:42–6.


27. Parrish CR, McClave SA. Checking gastric residual volumes: a practice in search of science? Pract Gastroenterol 2008;32:33–47.
28. Li YF, Lin HC, Torrazza RM, Parker L, Talaga E, Neu J. Gastric residual evaluation in preterm neonates: a useful monitoring technique or a hindrance? Pediatr Neonatol 2014;55:335–40.


29. Costalos C, Gounaris A, Sevastiadou S, Hatzistamatiou Z, Theodoraki M, Alexiou EN, et al. The effect of antenatal corticosteroids on gut peptides of preterm infants--a matched group comparison: corticosteroids and gut development. Early Hum Dev 2003;74:83–8.

30. Ewer AK, Durbin GM, Morgan ME, Booth IW. Gastric emptying in preterm infants. Arch Dis Child Fetal Neonatal Ed 1994;71:F24–7.



31. Szabo JS, Stonestreet BS, Oh W. Effects of hypoxemia on gastrointestinal blood flow and gastric emptying in the newborn piglet. Pediatr Res 1985;19:466–71.


32. Berseth CL. Effect of early feeding on maturation of the preterm infant's small intestine. J Pediatr 1992;120:947–53.


33. Van Den Driessche M, Peeters K, Marien P, Ghoos Y, Devlieger H, Veereman-Wauters G. Gastric emptying in formula-fed and breast-fed infants measured with the 13C-octanoic acid breath test. J Pediatr Gastroenterol Nutr 1999;29:46–51.


34. Ewer AK, Yu VY. Gastric emptying in pre-term infants: the effect of breast milk fortifier. Acta Paediatr 1996;85:1112–5.


35. van Goudoever JB. Nutrition for preterm infants: 75 years of history. Ann Nutr Metab 2018;72 Suppl 3(Suppl 3): 25–31.

36. Goldman HI, Goldman J, Kaufman I, Liebman OB. Late effects of early dietary protein intake on low-birth-weight infants. J Pediatr 1974;85:764–9.


37. Gathwala G, Shaw C, Shaw P, Yadav S, Sen J. Human milk fortification and gastric emptying in the preterm neonate. Int J Clin Pract 2008;62:1039–43.


38. de Ville K, Knapp E, Al-Tawil Y, Berseth CL. Slow infusion feedings enhance duodenal motor responses and gastric emptying in preterm infants. Am J Clin Nutr 1998;68:103–8.


39. Premji SS, Chessell L. Continuous nasogastric milk feeding versus intermittent bolus milk feeding for premature infants less than 1500 grams. Cochrane Database Syst Rev 2011;2011:CD001819.



41. van Wijk MP, Benninga MA, Dent J, Lontis R, Goodchild L, McCall LM, et al. Effect of body position changes on postprandial gastroesophageal reflux and gastric emptying in the healthy premature neonate. J Pediatr 2007;151:585–90. 590.e1–2.


42. Blumenthal I, Pildes RS. Effect of posture on the pattern of stomach emptying in the newborn. Pediatrics 1979;63:532–6.



43. Mora J, Punthmatharith B, Wattanasit P. Effect of positioning on gastric residual volume in preterm infants. Songklanagarind J Nurs 2017;37:35–46.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


