Introduction
Pulmonary crytococcosis that is caused by the inhalation of Cryptococcus neoformans (C. neoformans) is uncommonly recognized in childhood1). Because it has commonly occurred in immunocompromised subjects, little is known about pulmonary cryptococcosis in immunocompetent subjects, especially in those with no clinical symptoms2, 3). We report herein a 16-year-old boy who had asymptomatic isolated pulmonary cryptococcosis confirmed by needle aspiration biopsy.
Case report
A 16-year-old boy presented at our clinic with the presence of round opacity in the left lower lobe on chest x-rays that were taken for routine preoperative workup due to ankle fracture. He had no significant past and family histories. He had no respiratory symptoms such as cough, sputum or dyspnea but has a history of close contact with pigeons. The boy frequently used to visit a village with traditional houses, where many pigeons lived and kept some birds at home, too.
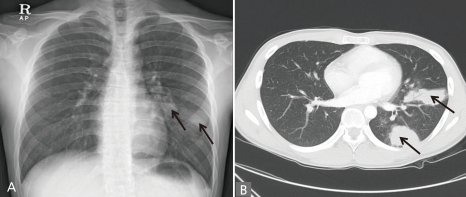
On physical examination, he appeared healthy. Pulmonary auscultation and percussion revealed no abnormal findings. A simple chest x-ray (Fig. 1A) showed round opacity on left lower lobe. Chest computerized tomography (CT) revealed round and well defined nodules in the left lower lobe, multiple subpleural and parenchymal nodules in left upper lobe and enlarged lymph nodes in the left hilar area (Fig. 1B). Because radiographs of patients with pulmonary cryptococcosis are non-specific and can easily be confused with pulmonary tuberculosis, we performed AFB staining and AFB culture from sputum and got a negative result.
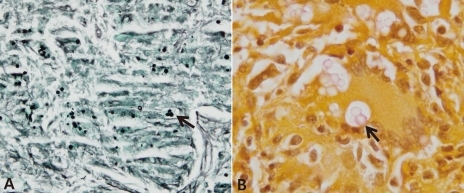
Under local anesthesia, fluoroscope guided fine needle aspiration was conducted and a lung specimen received from left lower lobe. PCR from tissue specimen was negative for tuberculous and nontuberculous Mycobacterium. The specimen exhibited multiple non-necrotizing granulomatous lesions by hematoxylin-eosin staining and round, black yeast-like bodies by Gomori methenamine silver staining (Fig. 2A). Since the bodies were suspicious of fungus, PAS staining and Mayer's mucicarmine staining (Fig. 2B) were performed, which identified the rose-red capsules of C. neoformans.
Routine laboratory findings including: white blood cell counts 12,500/µL (neutrophil 75%, absolute neutrophil count 7,575/µL), hemoglobin 12.9 g/dL, aspartate aminotransferase 14 IU/L, alanine aminotransferase 9 IU/L, showed no specific findings, c-reactive protein 15.2 mg/L showed mild elevation.
No abnormal findings were noticed in humoral antibody levels (IgG 1,430 mg/dL, IgA 282 mg/dL, IgM 176 mg/dL, and IgE 2.7 IU/mL), cellular immunological parameters (lymphocytes 1657/µL, CD4+ T cell 410/µL, and CD8+ T cell 340/µL), C3 (104 mg/dL), C4 (19.6 mg/dL) and CH50 (40.6 mg/dL). The patient was negative for the human immunodeficiency virus antibody test. Since cryptococcosis is reported to frequently occur in the central nervous system, he underwent brain magnetic resonance imaging, which showed no abnormal findings.
Discussion
The patient presented with isolated pulmonary cryptococcosis without immunological abnormalities. Although cryptococcosis usually occurs in immunocompromised subjects, it has been reported that pulmonary cryptococcosis is also discovered in the immunocompetent host2, 4). Cryptococcosis is thought to be acquired by inhalation of fungus contained in the excretion of birds such as pigeons, canaries and cockatoos into the respiratory system. It may also be found on fruits and vegetables, or carried by cockroaches5). Several reports indicated that pulmonary cryptococcosis among children is particularly uncommon1, 4), however, others suggest that exposure to this fungus is common among children, especially those living in an urban area6, 7). This suggests that cryptococcal infection may be common in children, but the infection is subclinical or not recognized4).
The characteristics of pulmonary cryptococcosis in immunocompetent subjects have not yet been understood well. An interesting aspect of pulmonary cryptococcosis is the potential for developing asymptomatic disease especially in immunocompetent subjects3, 8). Healthy individuals might also present with symptoms such as cough, fever, night sweating4). Since mild and non-specific symptoms appear and lesions are localized to the lungs with good clinical outcomes, it is inferred that host immune status may affect clinical manifestations9). Lesions due to C. neoformans vary in terms of inflammation depending on the host and the affected organ. Thus lesions seen in immunocompetent hosts and in the lungs tend to be more granulomatous than lesions seen in immunocompromised patients or in the brain10). A high index of clinical suspicion is required for the diagnosis of pulmonary cryptococcosis in immunocompetent children without clinical symptoms.
The most common radiologic findings of pulmonary cryptococcosis are solitary or multiple nodules11). The patient had multiple nodules in the parenchyma and subpleural space of the left lower lobe. Misdiagnosis to pulmonary tuberculosis or sarcoidosis is possible because tuberculosis infection is relatively common in Korea12). A definitive diagnosis of pulmonary cryptococcosis can be established by histological identification of the fungus in lung biopsy specimens. Generally, Hematoxylin-eosin staining of the specimen shows granulomatous lesions, which should be distinguished from tuberculosis and sarcoidosis11). In general, as well as in this case, yeast-like cells are seen by Gomori methenamine silver staining and the characteristic rose-red capsule of C. neoformans is identified by Mayer's mucicarmine staining, which is the most specific staining for Cryptococcosis 1).
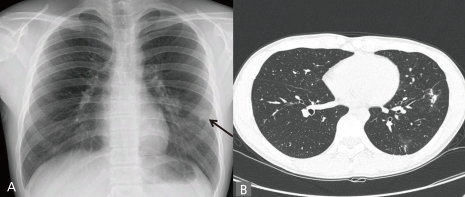
Fluconazole therapy is recommended in immunocompetent patients with asymptomatic cryptococcosis confined to the lungs13). The patient received oral fluconazole therapy for 8 weeks, and the follow-up chest CT showed resolution of the lesions. A substantial proportion of patients with cryptococcosis are apparently asymptomatic, especially in immunocompetent subjects. For this reason, pulmonary cryptococcosis should be considered as a differential diagnosis for asymptomatic pulmonary nodules, especially in cases showing well-delineated nodules.



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


