Introduction
Prevalence
Growth deficiency affects 10% of the rural outpatient population. The same percentage applies to high risk groups such as the homeless9).
FTT accounts for 1 to 5% of pediatric hospital admission for children younger than 2 years in the United State. National and state surveys indicate that as many as 10% of the children seen in primary care practice have signs suggesting inadequate growth5).
In inner city emergency department, approximately 15 to 30% of young children who receive acute care services show signs of growth deficits5).
Up to 15 to 20% of hospitalized children younger than 2 years from a medically indigent population met the criteria of FTT5).
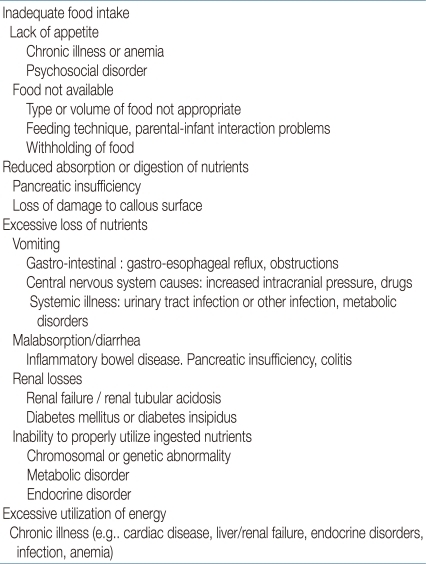
Etiology
Clinical approach to failure to thrive
Feeding: breast feeding or formula feeding, formula preparation, volume consumed, who feeds the infants, position and placement of the infant for feeding, timing and introduction of solids, stool or vomiting patterns associated with feeding, strength of suck. Accurate measurement of caloric intake of infants and children should be done by proper diet history.
Developmental history: gestational and perinatal history (age and parity of mother, medical complication of pregnancy, use of medications, use of drugs, use of alcohol, substance abuse, smoking, complications during delivery), developmental milestones, temperament.
There may be specific behavior characteristics of the child that play an important role. These characteristics include disrupted sleeping and eating patterns and behavior that is moody, demanding, rejecting, or distractible. Some authors have suggested that a subset of infants may refuse to eat in an attempt to achieve some degree of autonomy and control over their mothers and have termed this infantile anorexia nervosa.
Psychosocial history: family composition, employment and financial status, stress, potential isolation, child rearing beliefs, history of maternal depression, the caretaker's history of childhood neglect or abuse.
Family history: heights, weights, illness, development that may indicate constitutional short stature, inherited disease, developmental delay.
Physical examination
Head circumference, weight and height are proportionately reduced in infants and children who have hereditary and congenital defects.
Head circumference is normal and weight is slightly reduced proportionate to height in children with constitutional growth delay, genetic dwarfism or endocrinologic disorders.
Head circumference is normal and weight is reduced out of proportion to height in most infants with FTT, especially if malnutrition results from inadequate caloric intake, malabsorption, or altered metabolism.
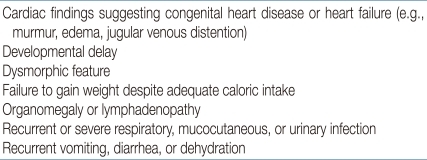
Investigations
Management
Provision of adequate calories, protein, and other nutrients
Nutritional counseling to the family
Monitoring of growth and nutritional status
Specific treatment of complications or deficiencies
Long term monitoring and follow up
Education of the family on social land nurturing techniques
Supportive economic assistance



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


