Introduction
The masticator space is defined as the separate fascial compartment containing the pterygoid, masseter and temporalis muscles and the mandible1,2). Masticator space abscess represents an advanced stage of a commonly odontogenic infection indicated by buccal pain, swelling and trismus3). Jaw swelling and trismus after a dental procedure are the typical clinical manifestations of a masticator space abscess in adults4,5). Masticator space abscess without dental procedure is an uncommon infection and can be seen with poor sucking, irritability, fever and dehydration in the infant. It is imperative that a meticulous medical history be obtained and a thorough physical examination be completed in infants with such clinical symptoms1). The clinical diagnosis is usually obvious, but it is confirmed by ultrasonography (US) or computed tomography (CT)1,5).
Masticator space abscess has not been reported in newborns, and rarely been reported in infants. Here we report a 47 day old male diagnosed as masticator space abscess with nonspecific symptoms without evidence of dental disease, traumatic injuries to the head and neck, or parotid swelling1).
Case report
A 47 day old male was admitted for fever, poor oral intake, irritability and right side mild bluish buccal swelling which have persisted for two days ago. He was born 3.47 kg at term by repeated Caesarean section. He was admitted for neonatal jaundice at the 5th day of life, but was generally healthy after discharge. He had no airway compromise, respiratory symptoms, or traumatic injuries. He received a bacille de calmette-guerin vaccine, and a first and second hepatitis B vaccination on schedule. He was fed by breast milk. He had no known drug allergies and was not taking any medication. He had no specific family history of recurrent infections except the cervical cancer of his aunt.
There were no inflammatory sign in the oral cavity and no discharge from Stensen's duct orifice. There were no other abnormal findings on physical examination.
Laboratory findings were as following: leukocytes 19,110/µL (segmented neutrophil 47.3%), platelet 516,000/µL, hemoglobin 12.6 g/dL, sodium 137 mmoL/L, potassium 5.47 mmoL/L, chloride 100 mmoL/L, amylase 7 IU/L, CRP 7.425 mg/dL, and mumps virus immunoglobulin M negative. Staphylococcus aureus (methicillin sensitive staphylococcus aureus, MSSA) was cultured from blood.
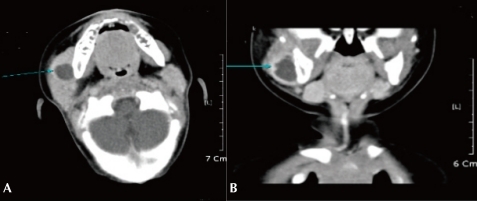
The first US taken at second hospital day revealed a mild cellulitis of the right cheek and soft tissue. Follow up ultrasonography was taken at the 5th hospital day. Early abscess formation at the right masticator space was suspected, but there was no inflammatory sign at the right parotid area on the second US (Fig. 1A). CT scan taken at 8th hospital day showed abscess formation at the right masticator space with adjacent cellulitis (Fig. 2).
The patient was referred to the Dental and Otorhinolaryngologic Department for a complete evaluation of odontogenic and oral/pharyngeal inflammation. No dental or gingival disease were observed.
The abscess was aspirated under the third US guidance at the 10th hospital day. One milliliter of turbid pus was aspirated and sent for culture and susceptibility tests. Ampicillin and cefotaxime was given intravenously to cover gram positive and gram negative bacteriae from the date of admission and clindamycin was added to cover anaerobes after the confirmation of abscess formation and aspiration of pus. S. aureus was isolated from the aspirated pus. The second blood culture sampled at the 6th hospital day showed no bacterial growth.
Fever had been subsided and swollen area had been reduced in size. The patient was discharged on the 16th hospital day with oral cefnidir. Antibiotics were continued for 5 days in outpatient clinic. Follow up US taken after a week from discharge showed no abscess in right masticator space, but right masseter muscle swelling and cortical irregularity on right mandible were still present. We checked the US taken after a month from discharge showed an improved state of the previously observed right masseter muscle and mandible lesion (Fig. 1B).
Discussion
A lesion arising within the masticator space tends to displace the parapharyngeal space posteromedially as it expands6). Children with deep neck abscesses, defined as involving the retropharyngeal or parapharyngeal regions; anterior or posterior triangle; the submandibular or submental areas and the parotid glands, present clinically different from adults7). Children younger than 4 years of age sometimes present with fever, agitation, nutritional problems caused by dysphagia, drooling, poor oral intake and respiratory illnesses like cough, stridor and respiratory distress7). Children younger than 6 years of age do not often present with trismus1).
The hallmark of masticator space abscesses under one year of age is not obvious, but it may manifest by the swelling of the cheek2) and irritability during pressure on the affected site.
The most common lesions underlying the masticator space abscess are odontogenic infections, which are encountered more frequently than neoplasm3,6). Most infections of the masticator space arise from the molars, especially the third molar2). The most common route of spread is posteriorly and medially extending to the temporal space without breakdown of the space barriers or it can break through the cervical fascia and spread medially to the parapharyngeal space2). Infiltration of the muscles by infectious spread from dental caries or as a complication of tooth extractions are frequently seen6). However, there was no case originated from odontogenic infections in children without dental procedure. The patient in this report had the masticator space abscess without a dental procedure and no obvious source of infection in the oral cavity.
Daramola et al.8) reported that there were parotid space, submandibular space, posterior neck and submandibular masticator space abscesses in pediatric patients and other studies showed that pediatric neck abscesses may arise from necrotic lymph nodes in limited cases. Small uncomplicated deep neck space abscesses may respond to intravenous antibiotics alone or antibiotics with needle aspiration7,9,10). Recently, ultrasonography had been recognized not only as diagnostic tool in the management of abscesses in the maxillofacial region but also as therapeutic tool11).
This patient presented with right posterior buccal swelling, thus parotitis had to be excluded2). Palpation is quite helpful in differential diagnosis since in parotid swelling, tenderness is mostly felt at the region of the gland along the posterior border of the masseter muscle, while a submasseteric abscess causes tenderness anteriorly2). A thorough history must always be taken, and parotid disease can be suspected if pain increases during meals2). Clinical suspicion of masticator space abscess could be given in this patient because he showed irritability during pressure on the anterior border of the affected parotid region and no abnormality of the right parotid gland was observed by ultrasonogarphy.
CT scanning with contrast is performed as an important tool because it can locate the site of lesion and extent of head and neck infections. Whether it is a cellulitis or an abscess, its size, and its location are particularly revealed in relation to the great vessels12).
In this patient, CT scan showed abscess formations in the right masseter muscle with adjacent cellulitis with no parotid space inflammation. Ultrasound-guided aspiration of masticator space abscess was done and 1ml of pus from the abscess was obtained. The S. aureus we obtained from the culture of pus is also the most common organism responsible for parotid disease13). According to Coticchia et al.7), it is also the most common causative organism in infants younger than 12 months of age with deep neck infections, whereas group A streptococcus is more frequently identified in older children. The patient has no clearly identifiable source of infection, but S. aureus was cultured from the initial blood test.
Daramola et al.8) reported that empiric antibiotic coverage for deep neck space abscesses must consider aerobic and anaerobic pathogens that synthesize beta-lactamase. According to Yang et al.14), Penicillin G is the drug of choice for infections caused by streptococci, and non-penicillinase-producing staphylococci, which represent the majority of aerobic organisms. Clindamycin is effective against all streptococci, most pneumococci, and most penicillin-resistant (but not methicillin-resistant) staphylococci. Third-generation parenteral cephalosporins have a broad spectrum of activity against enteric gram-negative rods. The patient was managed with ampicillin, cefotaxime, and clindamycin and the result of second blood culture showed no growth. He took the third generation cephalosporin drug, cefnidir, after discharge. MSSA cultured from this patient was sensitive to cephalothin, cefazolin, and cefotaxime. However, we think the first generation cephalosporin drugs, cephalothin or cefazolin, were better than the third generation cephalosporin drug.
The patient had a follow-up US which showed an improved state of the previously observed right masseter muscle swelling after about 1 month from the hospital discharge. We will continue to observe for any changes in it.
In conclusion, an infant with nonspecific symptoms such as fever, poor oral intake, irritability and right side mild bluish buccal swelling may indicate deep neck infections. US and CT scans of the head and neck, detailed history taking and physical examination would be important in identifying and adequately treating this infection.




 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


