Article Contents
| Korean J Pediatr > Volume 56(7); 2013 |
Abstract
Purpose
The purpose of this study was to evaluate short-term thyroid dysfunction and related risk factors in pediatric patients who underwent hematopoietic stem cell transplantation (HSCT) during childhood.
Methods
We studied 166 patients (100 boys and 66 girls) who underwent HSCT at the Catholic HSCT Center from January 2004 through December 2009. The mean age at HSCT was 10.0±4.8 years. Thyroid function of the patients was tested before and during 3 months of HSCT.
Results
Out of 166 patients, 165 (99.4%) underwent allotransplantation. Acute graft-versus-host disease (GVHD, grades II to IV) developed in 76 patients. Conditioning regimens before HSCT include total body irradiation (n=57), busulfan (n=80), and reduced intensity (n=29). Forty-five (27.1%) had thyroid dysfunction during 3 months after HSCT (29 euthyroid sick syndrome [ESS], 6 subclinical hyperthyroidism, 4 subclinical hypothyroidism, 3 hypothyroxinemia, 2 overt hyperthyroidism, and 1 high T4 syndrome). In a univariate logistic regression analysis, age at HSCT (P=0.002) and acute GVHD (P=0.009) had statistically significant relationships with thyroid dysfunction during 3 months after HSCT. Also, in a univariate logistic regression analysis, ESS (P=0.014) showed a strong statistically significant association with mortality.
Hematopoietic stem cell transplantation (HSCT) after intensive chemotherapy or radiation therapy has become an important therapeutic modality for hematologic malignancy, malignant tumors, aplastic anemia, and congenital and acquired immune diseases1). HSCT has improved the prognosis of children with malignant or nonmalignant hematologic disease. However, it has had significant adverse effects on the endocrine system, including thyroid, pituitary, and gonadal dysfunction2,3). Subclinical hypothyroidism and overt hypothyroidism are common long-term thyroid dysfunctions after HSCT2,4-8); thyroid tumors were reported in a smaller number of patients5,6).
Relevant previous studies have mostly focused on long-term thyroid dysfunction after HSCT2,4,6,7,9); only a few have focused on short-term changes. Euthyroid sick syndrome (ESS) was reported to be the most common short-term thyroid dysfunction3,10). However, there is no study on the frequency, progress, and risk factors of short-term thyroid dysfunction. We investigated risk factors for thyroid dysfunction during 3 months after HSCT in childhood.
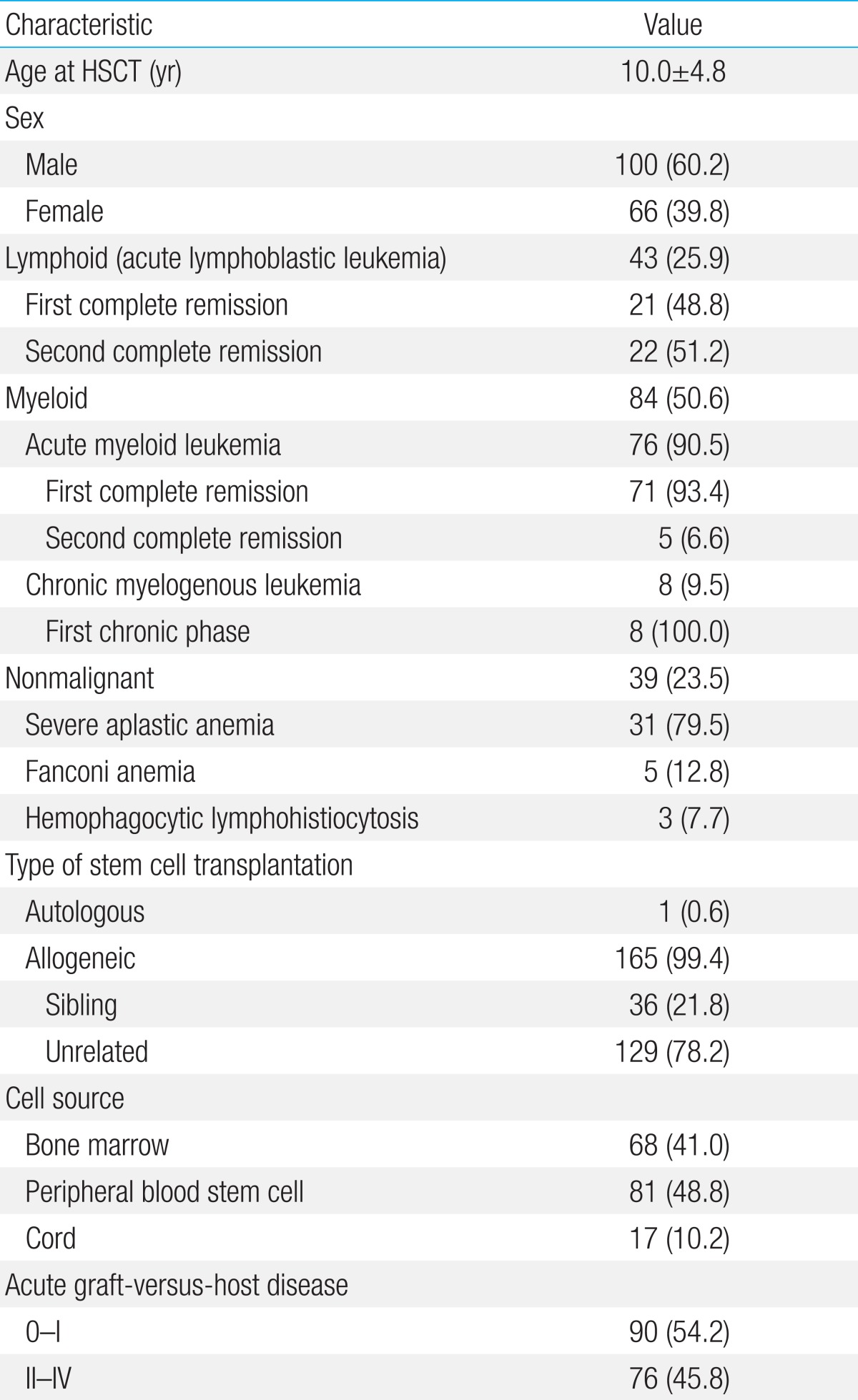
Out of 214 patients, 166 (100 females and 66 males) were included in the study. These patients had undergone HSCT at Seoul St. Mary's Hospital HSCT Center at the Catholic University of Korea from January 2004 through December 2009. Patients who were not evaluated for thyroid function (n=3), those with abnormal thyroid function before transplantation (n=28), those with solid tumor (n=13), and those who died within 3 months after HSCT (n=4) were excluded from the study. Patients underwent HSCT for malignant and nonmalignant hematological diseases (43 acute lymphoblastic leukemia, 79 acute myeloid leukemia, 8 chronic myelogenous leukemia, 31 aplastic anemia, 5 Fanconi anemia, 3 hemophagocytic lymphohistiocytosis). Twenty-one patients with acute lymphoblastic leukemia underwent transplantation after first complete remission and 22 patients underwent transplantation after second complete remission. Seventy-one patients with acute myeloid leukemia underwent transplantation after first complete remission, and 5 underwent transplantation after second complete remission. All 8 chronic myelogenous leukemia patients underwent transplantation after the first chronic phase (Table 1).
A grading system designed by Glucksberg in 1974 and modified by Keystone in 1994 was used to grade acute graft-versus-host disease (GVHD) according to the organs involved: skin, liver, and gastrointestinal tract11). The patients were suspected to have acute GVHD when the following symptoms manifested within the first 100 days after HSCT: skin rashes, blisters, excruciating abdominal pain with or without diarrhea, constant nausea and vomiting, and hepatitis (increase in bilirubin and liver enzyme levels). Seventy-six patients exhibited acute GVHD, grade II to IV, after HSCT.
Transplantation donors were patients themselves (n=1), siblings (n=36), and unrelated persons (n=129). The cell sources were bone marrow (n=68), peripheral blood (n=81), and cord blood (n=17) (Table 1). Preconditioning for transplantation was carried out according to the underlying diseases and the protocol used at the time of transplantation. Preconditioning regimens were classified according to the type of total body irradiation (TBI; 1,200 cGy, n=57), busulfan (n=80), and reduced intensity (n=29). Specifics of the conditioning regimen are outlined in Table 2.
Thyroid function was tested before and 3 months (averaging from 70 to 110 days after HSCT) after transplantation to assess thyroid-stimulating hormone (TSH), total triiodothyronine (T3), total thyroxine (T4), and free thyroxine (fT4). Serum was separated from obtained blood samples, and hormone levels were checked by radioimmune assay. Automated instrument (Adviacentaur, Siemens, Germany) was used for the assessment of TSH, T3, T4, and fT4.
The normal reference value of T3 was 0.8 to 2.1 ng/mL; free T4 was 0.8 to 2.2 ng/dL; T4 was 3.2 to 12.5 ng/dL; and TSH was 0.17 to 6.0 mIU/L. Diagnoses were based on the results of the thyroid function test and were as follows:
Cases with normal fT4 and TSH but decreased T3, or normal fT4 with decreased TSH and T3 were diagnosed as ESS12,13). Cases with only decreased TSH were diagnosed as subclinical hyperthyroidism. Cases with normal T3 and free T4 but TSH greater than 6 mIU/L were diagnosed as subclinical hypothyroidism. Cases with only decreased fT4 or T4 were diagnosed as hypothyroxemia. Cases with increased TSH and reduced fT4 were diagnosed as overt hypothyroidism. In addition, high T4 syndrome was diagnosed when only fT4 or T4 was increased12,13) (Table 3).
Descriptive Statistics are used to describe the clinical and treatment factors of patients. Values are expressed as mean±standard deviation. Univariate logistic regression analyses were performed to assess the risk factors that are considered to exert effects on thyroid dysfunction and the association between ESS during 3 months after HSCT and mortality. P values <0.05 were considered to be statistically significant. SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyses.
Compared with pre-HSCT data, test results 3 months after HSCT showed thyroid dysfunction in 45 patients (27.1%). Among the patients who showed thyroid dysfunction, 29 (64.4%) were ESS, 6 (13.3%) had subclinical hyperthyroidism, 4 (8.9%) had subclinical hypothyroidism, 3 (6.7%) had hypothyroxemia, 2 (4.5%) had overt hypothyroidism, and 1 (2.2%) had high T4 syndrome (Table 3).
According to univariate analysis, increase in age (P=0.002) and grade II acute GVHD or above (P=0.009) were significantly associated with thyroid dysfunction during 3 months after HSCT. The incidence of thyroid dysfunction showed no relationship with sex, underlying diseases or TBI in preconditioning regimen (Table 4).
The mean duration of follow-up was 5.9 years, ranging from 2.7 to 8.7 years. Among 166 patients, 48 patients died within average of 11 months. Cause of death was pneumonia (n=23), sepsis (n=12), GVHD (n=8), organ failure (n=3) and unknown (n=2).
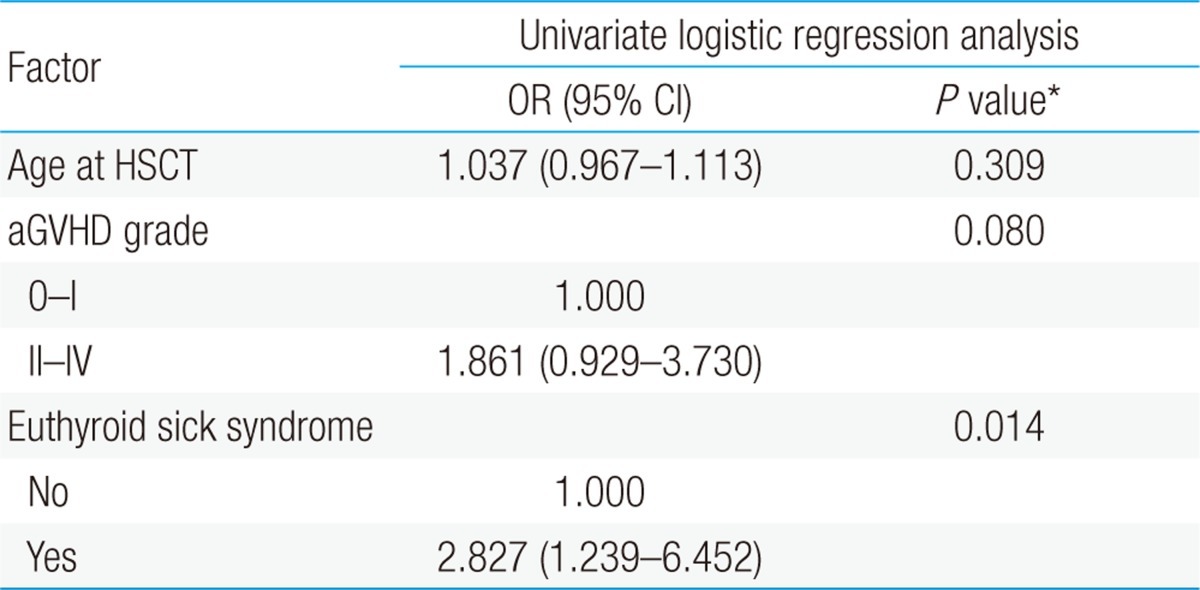
According to univariate analysis, mortality rate after HSCT was significantly higher in patients with ESS during 3 months after HSCT (P=0.014) as compared to the non-ESS group. Age (P=0.309) and grade of acute GVHD (P=0.080) showed no significant relationship with mortality (Table 5).
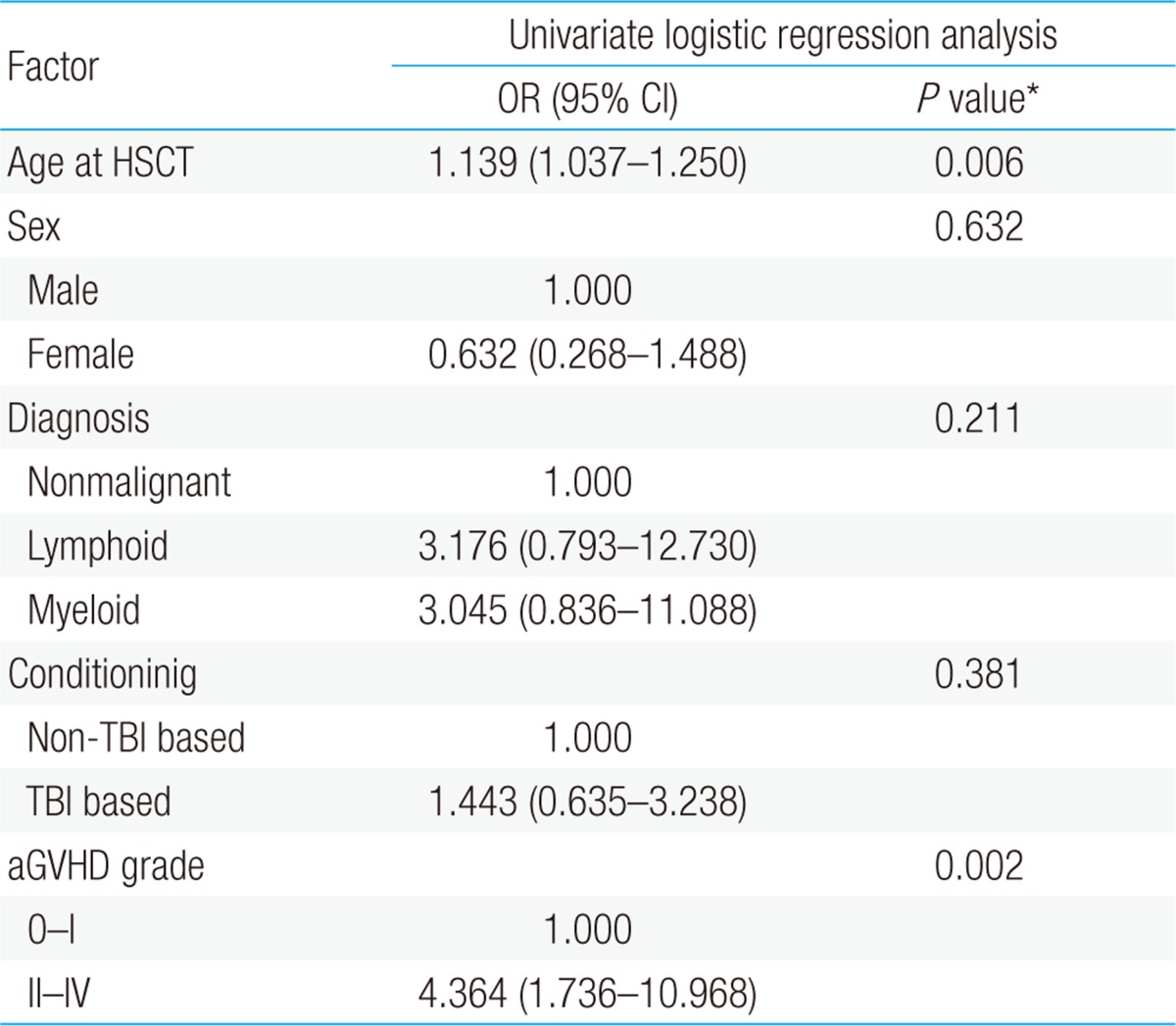
According to univariate analysis, the incidence rate of ESS was significantly higher in older children (P=0.006) and patients with acute GVHD of grade II or above (P=0.002). No statistical significance was shown between underlying diseases and preconditioning regimen (Table 6).
One of the most remarkable advances in modern medicine is the progress made in the field of transplantation technology, which has improved the survival rate of patients with malignant diseases, and these patients have made complete recovery7,8,14,15). The 5-year survival rate of childhood cancer has reached almost 80% and that of acute lymphoblastic leukemia or Hodgkins disease has increased up to 90%16). Endocrine complications have increased along with improved survival rate of patients. Approximately two thirds of possible complications occurring after transplantation are related to the endocrine system16). According to previous studies, endocrine complications such as developmental delays, gonadal dysfunction, and thyroid abnormalities were observed after transplantation1,16-19).
In this study, short-term thyroid dysfunction was detected in 27.1% (45 out of 166) of the patients. Among these 45 patients, ESS (64.4%, 29/45 patients) was the most common short-term thyroid dysfunction. ESS was also reported as frequent shortterm thyroid dysfunction by Toubert et al.3). A decrease in serum thyroid hormone level in ESS is often seen in stress-inducing conditions, such as starvation, sepsis, surgery, myocardial infarction, bone marrow transplantation, and, in fact, probably any severe illness. It is also called nonthyroidal illness syndrome (NTIS)12,13). With few exceptions, reports indicate that serum T3 level is low in patients with ESS. Serum T4 levels are reduced in ESS in proportion to the severity and probably the length of the illness13). The degree of alteration of thyroid hormones can predict the outcome in several disease processes12,13). In this study, mortality rate after HSCT was significantly higher in patients with ESS within 3 months during HSCT (P=0.014) compared to the non-ESS group. This result showed a close relationship between mortality rate and the incidence of ESS after HSCT. As presented above, ESS represents "hypothyroid state" which is disadvantageous to patients because thyroid hormone plays important role during illness by controlling metabolic rate13). Decrease in thyroid hormone could mean a critical damage in ability to overcome serious illness. Thus ESS patients may suffer more from illness and could lead to a worse prognosis. Therefore, ESS patients are more related to mortality rate than those who do not have ESS.
Another study including 80 patients from January 2004 to February 2006 was conducted in the same institute. The most observed short term thyroid dysfunction was ESS but most of them were reported to return to normal after 12 months follow-up. This difference can be explained by the fact that only part of ESS patients (27.5%, 22/80 patients) was followed up for their thyroid status after 12 months in previously mentioned study. These patients do not represent the whole group. Also, their survival after 12 months has not been discussed in the paper. Therefore, we could conclude that the focus of study was different.
There are 2 hypotheses to explain thyroid hormonal response in ESS: 1) the "hypothyroid" state is a physiologic response to illness that lowers metabolic rate-thereby conserving energy and assisting in recovery-or 2) the "hypothyroid" state is a maladaptive response that impairs tissue function and makes recovery from life threatening illness less likely12). In the latter case, thyroid hormone replacement might be beneficial, whereas if the former were true, such treatment would be harmful. Hence, hormone therapy for ESS is controversial12). De Groot13) reported that T3 levels in the pituitary are normal because of enhanced local deiodination. Thus, the pituitary is actually euthyroid, whereas the rest of the body is hypothyroid. The patient's serum and tissue hormone levels are truly low, and this is probably disadvantageous. However, Toubert et al.3) did not carry out any active treatment, because no advantage of thyroid hormone replacement therapy had been found in ESS patients. Moreover, Matsumoto et al.6) found that T3 levels in ESS patients normalized without treatment within 1 year after transplantation. In the present study, ESS patients did not receive thyroid hormone replacement after transplantation as benefits of the replacement are unclear.
While investigating pathogenesis of ESS, researchers have explored a number of possible mediators of ESS in recent years12,13). One study attempted to investigate the relationship between serum cortisol and T3 concentrations in patients with hyperpyrexia and ESS. However, administering steroids does not alter ESS in intensive care unit patients12). Free fatty acid (FFA), which commonly increases with fasting, stress, and some forms of ESS, can inhibit T4 binding. It may increase fT4 and decrease T4. However, a concentration of FFA in excess of 2 mmol/L is required to induce significant changes in T4 binding, and that is rarely seen in ESS. On the other hand, McIver and Gorman12) explained that interleukin-6 (IL-6) concentrations correlate inversely with T3 level in a number of ESS states, and IL-6 accounts for up to 30% of T3 variability. Many studies have also identified tumor necrosis factor alpha (TNF-α) as a reliable mediator that induces the reduction of T3 and TSH in ESS10,12).
Subclinical hyperthyroidism was found in 6 out of 45 patients (13.3%) with thyroid dysfunction occurring 3 month after HSCT. Subclinical hyperthyroidism can be associated with ESS, central hypothyroidism, pregnancy and use of drugs, such as steroids. Although additional examination, such as thyrotropin-releasing hormone test, is required to rule out these conditions, we did not carry out such a procedure. Such testing should be enforced after HSCT during following for thyroid function.
Overt hyperthyroidism was detected in 2 patients (4.5%) which is consistent with findings of previous studies. Ishiguro et al.9) reported 1 case of overt hyperthyroidism among 147 HSCT patients, and Sanders et al.14) reported 23 cases of overt hyperthyroidism among 791 HSCT patients.
Only 4 patients (8.9%) showed subclinical hypothyroidism, in contrast to previous reports where subclinical hypothyroidism was the most common complication in patients with long-term thyroid dysfunction after HSCT2,9,10). This difference could be due to the short-term focus of our study.
We sought to identify risk factors for thyroid dysfunction occurring 3 months after HSCT. Age and acute GVHD grade II or above were significantly associated with this outcome. No such relationship was found for TBI, sex, comorbidity, or type of preconditioning regimens. Our analysis of risk factors for ESS within 3 months after HSCT also identified age (P=0.002) and acute GVHD of grade II or above (P=0.009) as statistically significant. These findings are in keeping with results reported by Vexiau et al.20) who found more thyroid dysfunction in older children after HSCT compared to younger patients (19% vs. 38%). Moreover, Sanders et al.21) and Tauchmanova et al.22) reported that GVHD correlates linearly with endocrine complications in HSCT patients and it confers an adverse prognosis.
TBI has been reported to be a risk factor for thyroid dysfunction after HSCT, such as overt hypothyroidism and compensated hypothyroidism2,3,5,14,19). Sanders et al.14) and many other studies have reported more long-term thyroid dysfunction detected in patients who received TBI-based preconditioning15,17,23). However, this was not true in our study, because we focused on short-term thyroid dysfunction.
However, there are some limitations to this study. Although we mainly focused on short term thyroid dysfunction after HSCT in children, long term follow-up could have enabled us to compare our results with previous studies in depth. To overcome this limitation, longer follow-up and further evaluation of their thyroid function needs to be done.
In conclusion, we found that 27.1% of patients experienced thyroid dysfunction during 3 months after HSCT. Univariate analysis identified the relationship between age and acute GVHD of grade II or above with incidence of thyroid dysfunction. Moreover, ESS was found to be related to the mortality rate after HSCT. Thus, short term thyroid function needs to be evaluated after HSCT and any detected thyroid dysfunction should be closely observed for progression into other thyroid abnormalities. Furthermore, continual follow-up examination is crucial to ascertain the recovery of detected thyroid dysfunction.
References
1. Siekierska-Hellmann M, Babinska A, Obołonczyk L, Sworczak K, Hellmann A. One-year follow-up of TSH level and thyroid volume in patients with bone marrow or peripheral blood hematopoietic stem cell transplantation following chemotherapy. Pol Merkur Lekarski 2007;23:170–173.

2. Boulad F, Bromley M, Black P, Heller G, Sarafoglou K, Gillio A, et al. Thyroid dysfunction following bone marrow transplantation using hyperfractionated radiation. Bone Marrow Transplant 1995;15:71–76.

3. Toubert ME, Socie G, Gluckman E, Aractingi S, Esperou H, Devergie A, et al. Short- and long-term follow-up of thyroid dysfunction after allogeneic bone marrow transplantation without the use of preparative total body irradiation. Br J Haematol 1997;98:453–457.


4. Berger C, Le-Gallo B, Donadieu J, Richard O, Devergie A, Galambrun C, et al. Late thyroid toxicity in 153 long-term survivors of allogeneic bone marrow transplantation for acute lymphoblastic leukaemia. Bone Marrow Transplant 2005;35:991–995.


5. Katsanis E, Shapiro RS, Robison LL, Haake RJ, Kim T, Pescovitz OH, et al. Thyroid dysfunction following bone marrow transplantation: long-term follow-up of 80 pediatric patients. Bone Marrow Transplant 1990;5:335–340.

6. Matsumoto M, Ishiguro H, Tomita Y, Inoue H, Yasuda Y, Shimizu T, et al. Changes in thyroid function after bone marrow transplant in young patients. Pediatr Int 2004;46:291–295.


7. Sklar CA, Kim TH, Ramsay NK. Thyroid dysfunction among long-term survivors of bone marrow transplantation. Am J Med 1982;73:688–694.


8. Slatter MA, Gennery AR, Cheetham TD, Bhattacharya A, Crooks BN, Flood TJ, et al. Thyroid dysfunction after bone marrow transplantation for primary immunodeficiency without the use of total body irradiation in conditioning. Bone Marrow Transplant 2004;33:949–953.


9. Ishiguro H, Yasuda Y, Tomita Y, Shinagawa T, Shimizu T, Morimoto T, et al. Long-term follow-up of thyroid function in patients who received bone marrow transplantation during childhood and adolescence. J Clin Endocrinol Metab 2004;89:5981–5986.


10. Lee SJ, Lee JW, Lee DH, Kwon YJ, Park YS, Hwang HS, et al. Short-term follow up of thyroid function after pediatric hematopoietic stem cell transplantation. Korean J Pediatr 2006;49:1211–1215.

11. Jacobsohn DA. Acute graft-versus-host disease in children. Bone Marrow Transplant 2008;41:215–221.


13. De Groot LJ. Dangerous dogmas in medicine: the nonthyroidal illness syndrome. J Clin Endocrinol Metab 1999;84:151–164.


14. Sanders JE, Hoffmeister PA, Woolfrey AE, Carpenter PA, Storer BE, Storb RF, et al. Thyroid function following hematopoietic cell transplantation in children: 30 years' experience. Blood 2009;113:306–308.



15. Ricardi U, Corrias A, Einaudi S, Genitori L, Sandri A, di Montezemolo LC, et al. Thyroid dysfunction as a late effect in childhood medulloblastoma: a comparison of hyperfractionated versus conventionally fractionated craniospinal radiotherapy. Int J Radiat Oncol Biol Phys 2001;50:1287–1294.


16. Nandagopal R, Laverdiere C, Mulrooney D, Hudson MM, Meacham L. Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res 2008;69:65–74.



17. Jung MH, Cho KS, Lee JW, Chung NG, Cho B, Suh BK, et al. Endocrine complications after hematopoietic stem cell transplantation during childhood and adolescence. J Korean Med Sci 2009;24:1071–1077.



18. Sanders JE. Growth and development after hematopoietic cell transplant in children. Bone Marrow Transplant 2008;41:223–227.


19. Dvorak CC, Gracia CR, Sanders JE, Cheng EY, Baker KS, Pulsipher MA, et al. NCI, NHLBI/PBMTC first international conference on late effects after pediatric hematopoietic cell transplantation: endocrine challenges-thyroid dysfunction, growth impairment, bone health, & reproductive risks. Biol Blood Marrow Transplant 2011;17:1725–1738.



20. Vexiau P, Perez-Castiglioni P, Socie G, Devergie A, Toubert ME, Aractingi S, et al. The 'euthyroid sick syndrome': incidence, risk factors and prognostic value soon after allogeneic bone marrow transplantation. Br J Haematol 1993;85:778–782.


21. Sanders JE, Woolfrey AE, Carpenter PA, Storer BE, Hoffmeister PA, Deeg HJ, et al. Late effects among pediatric patients followed for nearly 4 decades after transplantation for severe aplastic anemia. Blood 2011;118:1421–1428.



Table 2
Preparative regimens for hematopoietic stem cell transplantation of 166 patients
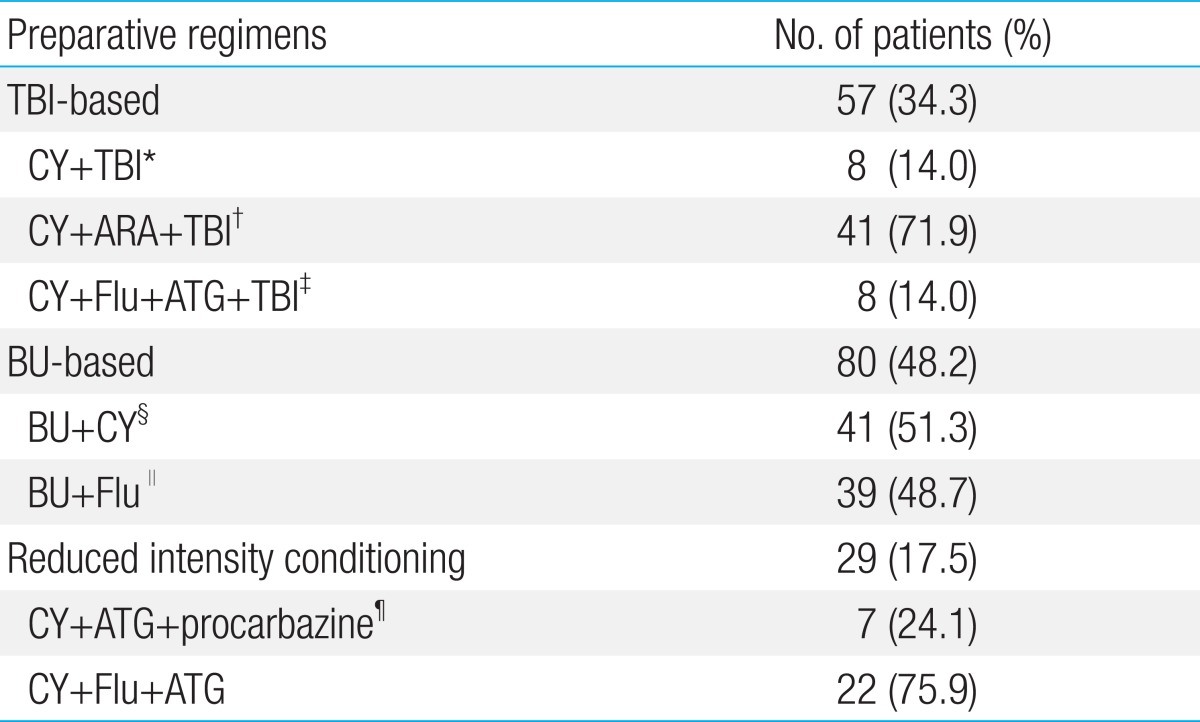
TBI, total body irradiation 1,200 cGy, 200 Gy/fraction, 2 fractions/day for 3 days; CY, cyclophosphamide; ARA, anthracycline; ATG, antithymocyte globulin; Flu, fludarabine; BU, busulfan; VP, Vepesid.
*CY 60 mg/kg for 2 days+TBI. †CY 60 mg/kg for 2 days+ARA 3 g/m2 twice per day for 2 days+TBI. CY 50 mg/kg for 4 days+Flu 30 mg/m2 for 6 days+ATG 1 V/20 kg for 3 days+TBI. §CY 60 mg/kg for 2 days+BU 0.8 mg/kg for 4 days. ∥BU 130 mg/m2 for 4 days+Flu 40 mg/m2 for 4 days. ¶CY 50 mg/kg for 4 days+ATG 1 V/20 kg for 3 days+procarbazine 12.5 mg/kg for 3 days.
-
METRICS

-
- 7 Crossref
- 0 Scopus
- 8,896 View
- 92 Download





 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation

