Article Contents
| Korean J Pediatr > Volume 58(6); 2015 |
|
Abstract
Purpose
The use of a 12-week steroid regimen (long-term therapy, LT) for the first episode of idiopathic nephrotic syndrome (NS) reportedly induces a more sustained remission and lower relapse rate than previous regimens, including an 8-week steroid regimen (short-term therapy, ST). Here, we assessed the potential for selective application of 2 steroid regimens (LT vs. ST) based on the days to remission (early responders [ER] vs. late responders [LR]) for the first idiopathic NS episode in children.
Methods
Patients were divided into 4 subgroups (ST+ER, ST+LR, LT+ER, and LT+LR) according to the initial steroid regimen used and rapidity of response; the baseline characteristics, relapse rates, and cumulative percentage of children with sustained remission were then compared among the 4 subgroups.
Results
Fifty-four children received ST, and the remaining 45 children received LT. As observed in previous studies, children receiving LT showed significantly lower relapse rates during the first year after the first NS episode than those receiving ST. The ST+ER group showed significantly lower relapse rates during the first one year and two years after the first NS episode than the the ST+LR group, whereas there were no significant differences of the relapse rates and duration to the first relapse between the ST+ER and LT+ER groups.
The 12-week steroid treatment regimen (long-term therapy, LT) including 6-week prednisolone (60 mg/m2 or 2 mg/kg daily) plus 6-week (40 mg/m2 or 1.5 mg/kg on alternative days) is the most commonly recommended regimen in the first episode of idiopathic nephrotic syndrome (NS) in children1,2). This regimen has produced more sustained remission and lower relapse rate than previously published regimens, including 8-week regimen (short-term therapy, ST) which comprises 4-week of prednisolone (60 mg/m2 or 2 mg/kg daily) plus 4 more weeks (40 mg/m2 or 1.5 mg/kg on alternative days)3). Recent studies such as the 16-week regimen4), long treatment tapering5) and addition of cyclosporine6) also failed to demonstrate a better outcome than LT.
On the assumption that all patients in the two regimen groups (LT vs. ST) have same number of days from the start of steroid therapy to remission in the first episode of NS, LT has additional 4 weeks of steroid treatment, especially 2 weeks of daily prednisolone after remission compared to ST. We speculated that this difference produces significant improvement in remission and relapse rates. This means that a longer duration of prednisolone therapy continued after remission during the first episode of NS is closely related to sustained remission and lower relapse rate. Moreover, Constantinescu et al.7) reported that if the remission occurred within the first week of initial steroid therapy, the patients without hematuria were more likely to show a lower relapse rate. Recently, a multicenter prospective study by Japanese Study Group of Renal Disease in Children also showed that the time to initial response ≥9 days is a significant predictor of frequent relapses8).
These two reports, in other words, also supported that longer duration of prednisolone therapy continued after remission during the first episode of NS can produce a lower relapse rate during follow-up.
The purpose of our study was to confirm the possibility of selective application of the two steroid treatment regimens (LT vs. ST) according to days to remission in the first episode of idiopathic NS in children.
We reviewed the medical records of the patients who were firstly diagnosed from 1990 up to the present with steroid-responsive idiopathic NS in Department of Pediatrics, Kyungpook National University Hospital, and divided these patients into two steroid regimen groups, ST versus LT, according to initial steroid therapy used. Renal biopsy was performed in only patients with frequent relapses or steroid dependency. All patients were followed up for at least two years. Although decision of treatment regimen was not taken for any specific reason, ST was usually used before 2000. Prednisolone was used in most of these patients, but in some patients, deflazacort (Calcort, Sanofi, Guildford, UK) was used. Five milligram of prednisolone was considered as the identical to 6 mg of deflazacort. The Institutional Review Board at Kyungpook National University Hospital, Daegu, South Korea reviewed and approved this study (IRB No. KNUMC_14-1014).
LT includes 6 weeks of prednisolone (60 mg/m2 or 2 mg/kg daily) plus 6 more weeks (40 mg/m2 or 1.5 mg/kg on alternative days), and ST includes 4 weeks of prednisolone (60 mg/m2 or 2 mg/kg daily) plus 4 more weeks (40 mg/m2 or 1.5 mg/kg on alternative days). NS is defined as the level of proteinuria over 40 mg/m2/hr and serum albumin below 2.5 g/dL. Remission is defined as the level of proteinuria below 4 mg/m2/hr or (-) or trace on urine a dipstick for 3 consecutive days, and relapse defined as level of proteinuria over 40 mg/m2/hr or over (++) on urine dipstick for 2 consecutive days. Enrolled patients had to have responded to initial steroid therapy and the eligible data of follow up for two years after initial episode to identify the remission and relapse rates. We defined the patients whose remission developed within the first week of initial steroid therapy as the "early responders (ER)", and those whose remission developed after the first week as the "late responders (LR)", giving four groups (LT+ER/LT+LR vs. ST+ER/ST+LR). We then compared the baseline characteristics, frequency of relapse and cumulative percentage of children with sustained remission among the 4 subgroups (Tables 1, 2).
Continuous variables were summarized by mean±standard deviation and, categorical variables were expressed as percentages. The differences in the distribution of the demographic and clinical characteristics between ST and LT group were detected by independent t-test or analysis of variance for continuous variables, and by chi-square test for categorical variables.
The survival curves were constructed by the Kaplan-Meier method with log-rank test to detect the difference among therapy groups (ST vs. LT and ST+ER vs. ST+LR vs. LT+ER vs. LT+LR). Cox proportional hazard regressions were performed to calculate the adjusted hazard ratios with 95% confidence interval, for effects of day to remission (ER vs. LR). The multivariate Cox proportional hazard regression model was adjusted for sex, age, hemoglobin, blood urea nitrogen (BUN), creatinine, total protein, albumin and total cholesterol. The statistical analyses were all performed with IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). P values less than 0.05 were considered significant.
In a total of 99 patients, 54 children received ST and the other 45 children received LT. There were no significant differences of clinical characteristics including mean age, serum albumin, total cholesterol and days to remission between these two groups (Table 1). Renal biopsy was performed in 36 of 54 children with ST and 27 of 45 with LT. Although some patients received additional immunosuppressive medications such as cyclosporine, chlorambucil and cyclophosphamide after renal biopsy, there was also no significant difference between these two groups. Total period of follow-up was 97.5±53.9 months in ST, 55.8±29.4 months in LT. As in other previous reports, the 45 children with LT showed significantly lower relapse rate during the first year after their first episode of NS, compared to children with ST (2.1±1.7 in ST vs. 1.3±1.4 in LT, P=0.014). In addition, the cumulative percentage of children with sustained remission in LT group was significantly higher than ST group (P=0.021) (Fig. 1).
Each of the therapy groups (ST vs. LT) was divided into 2 subgroups according to days to remission in the first episode of NS (ER vs. LR), so a total of 4 subgroups were compared (ST+ER/ST+LR and LT+ER/LT+LR). There were no significant differences of clinical characteristics including mean age, serum albumin and total cholesterol among these four subgroups. Days to remission in the first episode of NS were as follows: ST+ER, 5.9±0.9 days; ST+LR, 11.4±4.0 days; LT+ER, 5.6±1.4 days; LT+LR, 12.2±5.3 days (Table 2).
Compared with ST+LR, the ST+ER group showed a significantly lower relapse rate during the first one year (1.2±1.5/year vs. 2.5±1.7/year, P=0.001) and two years (2.1±2.3/year vs. 3.4±2.2/year, P=0.039). There were no significant differences of relapse rate between LT+ER and LT+LR.
On the other hand, there were no significant differences of the relapse rate during two years after the first episode of NS and the duration to the first relapse between ST+ER and LT+ER. The cumulative percentage of children with sustained remission in the ST+LR group was significantly lower than the other groups (ST+LR vs. ST+ER, P=0.004; ST+LR vs. LT+ER, P<0.001; ST+LR vs. LT+LR, P=0.041) and there was no significant difference of the cumulative percentage of children with sustained remission among ST+ER, LT+ER, and LT+LR (Fig. 2). In addition, in the multivariate Cox proportional hazard regression model adjusted for sex, age, hemoglobin, BUN, creatinine, total protein, albumin and total cholesterol, only ST+LR increased the adjusted hazard ratio of relapse more than 2.4 folds (95% confidence interval, 1.146-5.251) (Table 3).
The International Study of Kidney Diseases in Children (ISKDC) declared that an initial episode of minimal change NS (MCNS) is most susceptible to treatment with prednisone9), and various studies have analyzed the optimal duration of initial prednisone treatment ranging from 4 to 28 weeks3,4,5,9,10,11). At first, in 1981, the ISKDC suggested new prednisone regimen of 60 mg/m2/day for 4 weeks, followed by intermittent prednisone 40 mg/m2/day on 3 consecutive days out of 7 days for 4 weeks in the first episode of MCNS9). Arbeitsgemeinschaft für Pädiatrische Nephrologie (APN) compared the shorter regimen (prednisone 60 mg/m2/day until proteinuria had disappeared for 3 days, followed by 40 mg/m2/day per 48 hours until complete remission had occurred) to the 8-week regimen, it concluded that the 8-week regimen is better than the shorter regimen in the long-term prognosis10). However, APN proposed that an alternative day regimen would be better than the intermittent day regimen in 8-week regimen by ISKDC11). Since then, that 8-week steroid regimen made by the ISKDC9) and modified by the APN11) has been regarded as the standard steroid therapy for the initial attack of primary NS in children over ten years.
In 1993, a new 12-week regimen of prednisone therapy (60 mg/m2/day for 6 weeks, followed by 40 mg/m2/day on alternative days for 6 weeks) was compared to the 8-week regimen, and found a 30% reduction in risk of relapse at 12-24 months compared to the 8-week regimen2). Thus, it was concluded that the longer regimen is better than the 8-week regimen due to the reduction of the relapse rate without increasing risk of severe side effects12). In spite the increasing frequency of milder side effects such as cushingoid appearance and hypertrichosis, they concluded that the advantages of 12-week long regimen outweighed the risks and recommended this regimen for the initial treatment of MCNS13). Recent studies such as the 16-week regimen4), long treatment tapering5) and addition of cyclosporine6) have failed to demonstrate a better outcome than this treatment regimen, thus at present, the 12-week steroid regimen is the most popular steroid regimen for the first episode of primary NS in children1,2).
The question as to the main reason for the difference of outcome between 8- and 12-week regimen may arise. On the assumption that all patients of two steroid treatment regimens have same number of days from the onset of initial steroid therapy to remission in the first episode of NS, the 12-week regimen has an additional 4 weeks of treatment period, and in particular 2 weeks of daily prednisolone therapy after remission, compared to the 8-week regimen; we conclude that this difference is the main cause for significant improvement in remission and relapse rates. In other words, the longer duration of prednisolone therapy after remission during the first episode of NS is closely related to sustained remission and lower relapse rates.
The response to prednisone treatment is usually developed within 2 weeks after starting the steroid therapy in the first attack of NS10) and the rapidity of response correlates well with the relapse rate, especially in the patients without hematuria during the first year after the onset of NS7,8). This result also suggested that longer duration of prednisolone therapy continued after remission during the first episode of NS is closely related to lower relapse rate. However, other regimens longer than 12-week steroid regimen failed to produce any significant improvement of outcome4,5), so a longer length of steroid therapy always does not improved the outcome.
Therefore, we defined the patients with remission developed within the first week of steroid therapy as 'the early responders (ER)' and them after the first week as 'the late responders (LR)' in the patients receiving two regimens (12-week regimen vs. 8-week regimen). And then, we primarily compared the outcomes, including the persistence of remission and relapse rate between early and late responders (ER and LR) in same regimen, and secondarily, between same responders in two regimens (i.e., ER in patients in the 8-week regimen vs. ER in the 12-week regimen, and LR in the 8-week regimen versus LR in the 12-week regimen).
The patients in the 12-week regimen showed a longer interval to the first relapse and lower relapse rate than them in the 8-week regimen during 1 year of follow-up, but this result was limited to patients whose remission occurred after the first week of steroid therapy, so capable to daily prednisolone therapy for less than three weeks in the 8-week regimen group. Whereas, the patients whose remission occurred within the first week of steroid therapy in the 8-week regimen group did not show any difference in outcome compared to the 12-week regimen group. In other words, if the patient has daily prednisolone therapy for more than three weeks in the 8-week regimen, they can have similar outcome to the 12-week regimen group. Therefore, for the first episode of idiopathic NS, we suggest that the initial steroid regimen used can be either 12-week or 8-week regimen depending on the rapidity of response; i.e., a 12-week regimen for patients whose remission occurred after the first week of steroid therapy and 8-week regimen for those whose remission occurred within the first week of steroid therapy.
As our study has some limitations such as a retrospective study and small size of patients, we suggest a new prospective controlled study for steroid therapy regimens in the first episode of idiopathic NS based on our results. According to days to remission, there would be three steroid regimens that will provide more than three weeks of daily prednisolone therapy for all cases of remission within three weeks after steroid therapy, they are; (1) an 8-week regimen in patients whose remission occurred within the first week of initial steroid therapy, (2) a 10-week regimen in patients whose remission occurred from the end of first week to the second week of initial steroid therapy, and (3) a 12-week regimen in patients whose remission occurred from the end of second week to the third week of initial steroid therapy.
Conflicts of interest
Conflicts of interest:
No potential conflict of interest relevant to this article was reported.
References
1. Gipson DS, Massengill SF, Yao L, Nagaraj S, Smoyer WE, Mahan JD, et al. Management of childhood onset nephrotic syndrome. Pediatrics 2009;124:747–757.


2. Lombel RM, Gipson DS, Hodson EM. Kidney Disease: Improving Global Outcomes. Treatment of steroid-sensitive nephrotic syndrome: new guidelines from KDIGO. Pediatr Nephrol 2013;28:415–426.


3. Lande MB, Gullion C, Hogg RJ, Gauthier B, Shah B, Leonard MB, et al. Long versus standard initial steroid therapy for children with the nephrotic syndromeA report from the Southwest Pediatric Nephrology Study Group. Pediatr Nephrol 2003;18:342–346.


4. Bagga A, Hari P, Srivastava RN. Prolonged versus standard prednisolone therapy for initial episode of nephrotic syndrome. Pediatr Nephrol 1999;13:824–827.


5. Hiraoka M, Tsukahara H, Matsubara K, Tsurusawa M, Takeda N, Haruki S, et al. A randomized study of two long-course prednisolone regimens for nephrotic syndrome in children. Am J Kidney Dis 2003;41:1155–1162.


6. Hoyer PF, Brodeh J. Initial treatment of idiopathic nephrotic syndrome in children: prednisone versus prednisone plus cyclosporine A: a prospective, randomized trial. J Am Soc Nephrol 2006;17:1151–1157.


7. Constantinescu AR, Shah HB, Foote EF, Weiss LS. Predicting first-year relapses in children with nephrotic syndrome. Pediatrics 2000;105(3 Pt 1): 492–495.


8. Nakanishi K, Iijima K, Ishikura K, Hataya H, Nakazato H, Sasaki S, et al. Two-year outcome of the ISKDC regimen and frequent-relapsing risk in children with idiopathic nephrotic syndrome. Clin J Am Soc Nephrol 2013;8:756–762.



9. The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr 1981;98:561–564.


10. Short versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft für Pädiatrische Nephrologie. Lancet 1988;1:380–383.

11. Brodehl J, Krohn HP, Ehrich JH. The treatment of minimal change nephrotic syndrome (lipoid nephrosis): cooperative studies of the Arbeitsgemeinschaft für Pädiatrische Nephrologie (APN). Klin Padiatr 1982;194:162–165.


Fig. 1
Cumulative percentages of children with sustained remission after 2 initial steroid regimens (ST vs. LT). ST, short-term therapy; LT, long-term therapy.
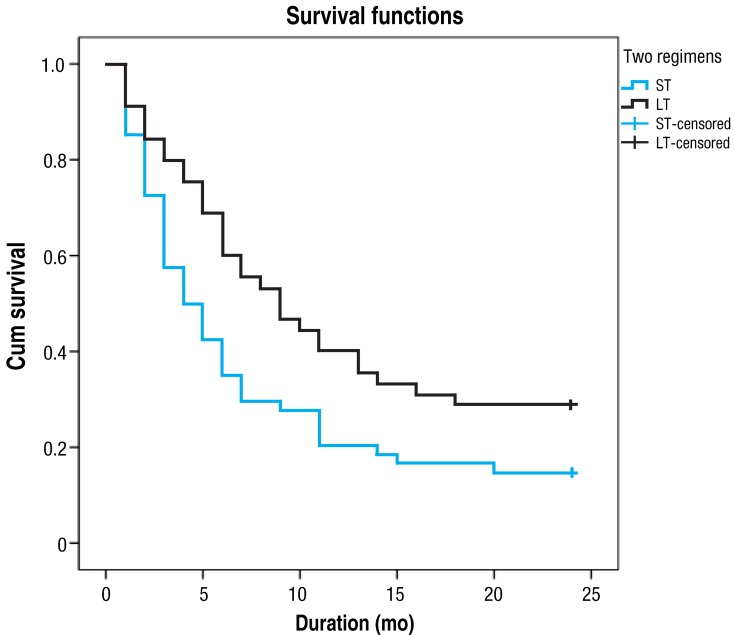
Fig. 2
Cumulative percentages of children with sustained remission based on the days to remission after two initial steroid regimens. ST, short-term therapy; ER, early responders; LR, late responders; LT, long-term therapy.

Table 1
Comparison of the baseline characteristics and frequency of relapse based on the initial steroid regimens
Table 2
Comparison of the baseline characteristics and frequency of relapse based on the initial steroid regimens and rapidity of remission
Table 3
Comparison of the relapse rates of nephrotic syndrome between the ST+ER and other subgroups by using the multivariate Cox proportional hazard regression model (adjusted for sex, age, and hemoglobin, blood urea nitrogen, creatinine, total protein, albumin, and total cholesterol levels)
| Subgroup | Hazard ratio (95% confidence Interval) | P value |
|---|---|---|
| ST+ER (reference) | ||
| ST+LR | 2.453 (1.146-5.251) | 0.021 |
| LT+ER | 0.911 (0.386-2.152) | 0.832 |
| LT+LR | 1.440 (0.631-3.286) | 0.386 |



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


