Article Contents
| Korean J Pediatr > Volume 60(3); 2017 |
|
Abstract
Purpose
The goal of nutritional support for very-low-birth-weight (VLBW) infants from birth to term is to match the in utero growth rates; however, this is rarely achieved.
Methods
We evaluated postdischarge growth patterns and growth failure in 81 Korean VLBW infants through a retrospective study. Weight and height were measured and calculated based on age percentile distribution every 3 months until age 24 months. Growth failure was defined as weight and height below the 10th percentile at 24 months. For the subgroup analysis, small-for-gestational age (SGA) and extremely low birth weight (ELBW) infants were evaluated. The growth patterns based on the Korean, World Health Organization (WHO), or Centers for Disease Control and Prevention (CDC) standard were serially compared over time.
Results
At postconception age (PCA) 40 weeks, 47 (58%) and 45 infants (55%) showed growth failure in terms of weight and height, respectively. At PCA 24 months, 20 infants (24%) showed growth failure for weight and 14 (18%) for height. Growth failure rates were higher for the SGA infants than for the appropriate-weight-for-gestational age infants at PCA 24 months (P=0.045 for weight and P=0.038 for height). Growth failure rates were higher for the ELBW infants than for the non-ELBW infants at PCA 24 months (P<0.001 for weight and P=0.003 for height). Significant differences were found among the WHO, CDC, and Korean standards (P<0.001).
The goal of nutritional support for very low birth weight (VLBW; <1,500 g) infants from birth to term is to match the in utero growth rates of normally growing fetuses1,2). Unfortunately, this goal is rarely achieved because of chronic undernutrition and poor growth3,4,5). Neonatal nutrition and the resulting postnatal growth are major determinants of short- and long-term outcomes for preterm infants6,7,8).
Among VLBW infants of 24–32 weeks' gestational age who were discharged at ≤40 weeks postconception age (PCA), the percentage of those with severe growth failure has decreased significantly, from 11.5% in 1995–2000 to 5.2% in 2006–2010, and mild growth failure declined from 40.1% to 9.8% during these periods; however, these improvements remain insufficient9).
In a previous study, among extremely low birth weight (ELBW; <1,000 g) infants assessed at 18–22 months' term-equivalent age, 50.5% and 31.7%, respectively, had weights and heights below the 10th percentile at follow-up10). In another study, among VLBW infants assessed at a corrected term-equivalent age of 24 months, 67.1% had achieved catch-up growth. Korean data from 2000 to 2001 show that 32.9% of VLBW infants have growth failure at a term-equivalent age of 24 months; however, there are no recent data11).
The Korean growth standard commonly used in Korean infants, including preterm infants, was revised in 200712). Internationally, the World Health Organization (WHO) chart13) and the Centers for Disease Control and Prevention (CDC) standards14) are used; however, variations in growth outcomes are frequently observed depending on the growth chart used. In addition, no study has yet compared those standards with each other.
In this study, we aimed to evaluate postdischarge growth patterns in Korean VLBW infants and to analyze the growth failure proportions in small for gestational age (SGA) and ELBW infants. Moreover, we aimed to compare the percentile distribution in weight and height between the Korean standard and the WHO and CDC standards.
This is a retrospective analysis of the medical records of VLBW infants admitted to the Severance Children's Hospital and Gangnam Severance Hospital neonatal intensive care unit from January 1, 2010 to December 31, 2011 and followed up at the outpatient clinic until PCA 24 months. Growth parameters, such as height and weight, were measured for all infants every 3 months. Growth standard curves were used to divide the growth parameters into 10 groups for statistical analysis (<3rd, 3rd–5th, 5th–10th, 10th-25th, 25th-50th, 50-75th, 75-90th, 90-95th, 95-97th, and >97th percentile). The growth curves used in this study were the 2007 Korean growth standard curves (http://www.cdc.go.kr)12), the US CDC growth charts (http://www.cdc.gov/growthcharts)14), and the WHO growth charts (http://www.cdc.gov/growthcharts)13). SGA was defined as birth weight below the 10th percentile for gestational age using fetal growth charts15). Growth failure was defined as below 10th percentile in weight of height at each period.
Statistical analysis was performed with IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Repeated-measures analyses of variance were used for comparisons among the growth standards, and P values of <0.05 were considered statistically significant.
The study protocol was reviewed and approved by Institutional Review Board of Gangnam Severance Hospital (approval number: 2016-0297-001). The requirement for informed consent was waived by the board due to the study's retrospective nature.
Total 139 VLBW infants were born and discharged from Severance Children's Hospital and Gangnam Severance Hospital neonatal intensive care unit from January 1, 2010 to December 31, 2011. Total 81 patients were enrolled and followed up at the outpatient clinic until PCA 24 months. 58 infants were lost for follow-up before 24 months of age.
Eighty-one VLBW infants (gestational age, 28.3±3.6 weeks; birth weight, 1,137±335 g) were enrolled. Of those infants, 38.9% were male. The mean Apgar score was 2.5±1.7 at 1 minute and 5.4±1.4 at 5 minutes. The mean hospital stay was 68.6±38.6 days (Table 1). The birth weights of 21% of infants were <10th percentile and none were >90th percentile (Table 2).
Among total group, the growth failure proportion at PCA 40 weeks was 58% and that at PCA 24 months was 24% according to the Korean standard; these infants achieved significant catch-up growth (P<0.001) (Fig. 1). Birth heights for 21% of infants were <10th percentile, and none were >90th percentile. The percentage of infants with heights <10th percentile was 55% at PCA 40 weeks and 18% at PCA 24 months by the Korean standard, indicating that they had achieved significant catch-up growth (P<0.001) (Fig. 2).
In the analysis of growth failure (<10th percentile) in SGA and appropriate weight for gestational age (AGA) infants over time with the Korean standard, 81% of SGA infants were at the <10th percentile weight reference at PCA 40 weeks, and 29% were at the <10th percentile weight reference at PCA 24 months. Of the AGA infants, 53% were at the <10th percentile weight reference at PCA 40 weeks, and 21% PCA 24 months. Growth failure in weight for the SGA infants were higher than AGA infants (29% vs. 21%, P=0.045). Of the SGA infants, 75% were at the <10th percentile height reference at PCA 40 weeks, and 37% at PCA 24 months. Of the AGA infants, 49% were at the <10th percentile height reference at PCA 40 weeks, and 13% at PCA 24 months. Growth failure in height, SGA infants were higher than AGA infants (37% vs. 13%, P=0.038) (Fig. 3).
In the analysis of growth failure proportions (<10th percentile) among ELBW and non-ELBW (1,000–1,500 g) infants over time using the Korean standard, 17% of ELBW infants showed weight growth failure at birth, 75% at PCA 40 weeks, and 42% at PCA 24 months. Among the non-ELBW infants, the rates were 25% at birth, 43% at PCA 40 weeks, and 10% at PCA 24 months. The rates of height growth failure of ELBW infants were 17% at birth, 72% at PCA 40 weeks, and 25% at PCA 24 months. For non-ELBW infants, the rates were 25% at birth, 30% at PCA 40 weeks, and 8% at PCA 24 months (Fig. 4). Growth failure rates were higher for ELBW than for non-ELBW infants at PCA 24 months (P<0.001 for weight, P=0.003 for height).
VLBW infants showed gradual catch-up growth in weight according to Korean, WHO, and CDC standard charts. With the Korean standard, the growth failure rate in infants whose weight was <10th percentile was 58.4% at PCA 40 weeks and 24.3% at PCA 24 months.
Single patient in a period can be either classified into growth failure or not using different growth chart. We compared each growth standard over time, and a significant difference (P<0.001) was found among the WHO, CDC, and Korean standards (Fig. 5). Both boys and girls showed significant catch-up growth in weight over time. For the boys, the mean weight was above the 25th percentile; however, for the girls, the mean weight was below the 25th percentile based on the Korean standard. Girls showed a trend toward lower rates of catch-up growth. The comparison of height percentiles between boys and girls showed no significant differences; both sexes showed a mean height above the 25th percentile.
Our study results showed growth failure in weight in 58.4% of VLBW infants and in height in 50.5% of infants at PCA 40 weeks. However, significant catch-up growth was observed at PCA 24 months. The rates of growth failure were 24.3% for weight and 18.1% for height at PCA 24 months.
The recommendation to allow preterm infants to grow at a rate comparable to the age-matched fetus in utero is traditionally clear1,2). Recently, there are other opinions about the adjustment of postnatal growth trajectories because all neonates including very preterm infants lose extracellular fluid after birth and tend to follow a lower percentile than their birth percentile16). However, extrauterine growth restriction commonly occurs in neonatal units17,18). Very preterm infants frequently experience cumulative energy and protein deficits despite attempts of aggressive nutritional support.
Achieving proper growth in preterm infants is important. Epidemiologic evidence shows that early nutrition and growth in preterm infants influence their development of diseases later in life, as well as their neurodevelopmental outcomes19,20,21). This study provides recent data on the postnatal growth of VLBW infants from birth to PCA 24 months in Korea.
The percentage of infants with severe growth failure has decreased significantly over time; however, the rate remains. In a study by Ofek Shlomai et al.9), among VLBW infants born at 24- to 32-week gestational age who were discharged home at ≤40 weeks postmenstrual age, the percentage of those with severe growth failure decreased significantly from 11.5% in 1995–2000 to 5.2% in 2006–2010, and those with mild growth failure declined from 40.1% to 9.8% during these periods (P<0.001). In a study by Cole et al.10), among ELBW infants assessed at 18–22 months of corrected gestational age, 50.5% and 31.7% had weights and heights <10th percentile at follow-up, respectively. In our study, growth failure in weight was noted 58.4% of infants at PCA 40 weeks, and growth failure in height was 50.5%. However, this study showed significant catch-up growth at PCA 24 months. Growth failure rate was 24.3% in weight and 18.1% in height at PCA 24 month.
In another study, among VLBW infants assessed at a corrected age of 24 months, 67.1% had achieved catch-up growth. In a study by Hack et al.22), which involved comparisons with control newborns, male and female VLBW children showed significantly lower mean weight Z scores at 8 years of age. At age 20 years, these differences persisted among men; however, they were no longer significant among women. Furthermore, VLBW boys had significantly lower mean height Z scores at both 8 and 20 years, whereas the girls did not differ significantly from controls at either 8 or 20 years.
A greater incidence of poor growth has been reported in SGA infants than in AGA infants. Sung et al.23) compared SGA infants with AGA infants matched for either gestational weight or birth weight up to the age of 3 years, and concluded that intrauterine growth restriction in VLBW infants has a significant long-term impact on growth. In another study, SGA infant showed 70.6% and 67.9% of growth failure (less than -2 standard deviation) at each 12 months and 24 months of age. On the other hand AGA infant showed 29.4% and 21.8% of growth failure at each 12 months and 24 months of age24). In our study, the growth failure (weight<10th percentile) rates of SGA infants based on the Korean standard were 71% at PCA 40 weeks and 29% at PCA 24 months. However, SGA infants showed more postnatal growth failure than did AGA infants. SGA infants achieved significant catch-up growth in both weight and height; however, the decrease in growth lag was better in weight than in height.
The ideal growth pattern in preterm infants remains undefined. Consequently, correct evaluation of the postnatal growth of these infants is of primary concern, although the definition of the optimal postnatal growth pattern is still controversial19).
To evaluate the postnatal growth of preterm infants, the 2007 revision of Korean standard is the most commonly used standard in Korea. In this standard, 142,945 children surveyed in 2005, were randomized and selected from the Korean population. The CDC's growth chart was released in 2000, and it excluded data for VLBW. A typical growth standard from birth to 5 years of age was released by the WHO, which was based on a multiethnic population of term, breast-fed infants without known health or environmental constraints to growth. In this standard, birth weight<1,500 g was excluded.
Currently, because of lack of an international longitudinal standard for evaluating postnatal growth in preterm infants25), confusion in the assessment of growth failure may occur when different charts are used. Thus, the assessment of growth failure at the same time points can produce different results if a different growth standard is used. In clinical practice, the best compromise is necessary to compare the different charts for the evaluation of growth of Korean VLBW infants. When the growth patterns were serially compared among the Korean, WHO, and CDC standards, significant differences were observed (P<0.001), and it is unclear which growth chart is ideal for evaluating growth in preterm infants. The INTERGROWTH study is expected to rectify this problem26,27). This study is limited by its small sample size, only two institution study, and retrospective design. Furthermore, the infants were followed-up only up to 2 years of age. Further longitudinal growth monitoring is needed to validate our findings.
In conclusion, with advancements in neonatal care, the catch up growth of VLBW infants was much improved, but remained inadequate. For SGA and ELBW infants, growth impairment was more severe. Careful observation and aggressive interventions, especially in SGA and ELBW infants, are needed.
Acknowledgment
This study was supported by a new faculty research seed money grant from Yonsei University College of Medicine for 2015 (2015-32-0020).
Notes
Conflict of interest:
No potential conflict of interest relevant to this article was reported.
References
1. American Academy of Pediatrics Committee on Nutrition: Nutritional needs of low-birth-weight infants. Pediatrics 1985;75:976–986.

2. Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 2006;117:1253–1261.


3. Worrell LA, Thorp JW, Tucker R, McKinley LT, Chen J, Chng YM, et al. The effects of the introduction of a high-nutrient transitional formula on growth and development of very-low-birth-weight infants. J Perinatol 2002;22:112–119.


4. Stefanescu BM, Gillam-Krakauer M, Stefanescu AR, Markham M, Kosinski JL. Very low birth weight infant care: adherence to a new nutrition protocol improves growth outcomes and reduces infectious risk. Early Hum Dev 2016;94:25–30.


5. Johnson MJ, Wootton SA, Leaf AA, Jackson AA. Preterm birth and body composition at term equivalent age: a systematic review and meta-analysis. Pediatrics 2012;130:e640–e649.


6. Corpeleijn WE, Kouwenhoven SM, van Goudoever JB. Optimal growth of preterm infants. World Rev Nutr Diet 2013;106:149–155.


7. Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, Davis PJ. Outcomes for extremely premature infants. Anesth Analg 2015;120:1337–1351.



8. Lucas A, Morley R, Cole TJ. Randomised trial of early diet in pre-term babies and later intelligence quotient. BMJ 1998;317:1481–1487.



9. Ofek Shlomai N, Reichman B, Lerner-Geva L, Boyko V, Bar-Oz B. Population-based study shows improved postnatal growth in preterm very-low-birthweight infants between 1995 and 2010. Acta Paediatr 2014;103:498–503.


10. Cole CR, Hansen NI, Higgins RD, Ziegler TR, Stoll BJ. Eunice Kennedy Shriver NICHD Neonatal Research Network. Very low birth weight preterm infants with surgical short bowel syndrome: incidence, morbidity and mortality, and growth outcomes at 18 to 22 months. Pediatrics 2008;122:e573–e582.



11. Ma TH, Kim KA, Ko SY, Lee YK, Shin SM. Catch-up growth and development of very low birth weight infants. Korean J Pediatr 2006;49:29–33.

12. Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr 2008;51:1–25.

13. Grummer-Strawn LM, Reinold C, Krebs NF. Centers for Disease Control and Prevention (CDC). Use of World Health Organization and CDC growth charts for children aged 0-59 months in the United States. MMWR Recomm Rep 2010;59(RR-9): 1–15.
14. Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002;(246): 1–190.
15. Lubchenco LO. Classification of high risk infants by birth weight and gestational age: an overview. Major Probl Clin Pediatr 1976;14:1–279.

16. Rochow N, Raja P, Liu K, Fenton T, Landau-Crangle E, Göttler S, et al. Physiological adjustment to postnatal growth trajectories in healthy preterm infants. Pediatr Res 2016;79:870–879.


17. Kim ES, Sohn JA, Lee EH, Choi EJ, Lee HJ, Lee JA, et al. Extrauterine growth restriction in very low birth weight infants. J Korean Soc Neonatol 2010;17:53–63.
18. Yu VY. Extrauterine growth restriction in preterm infants: importance of optimizing nutrition in neonatal intensive care units. Croat Med J 2005;46:737–743.

19. Bertino E, Di Nicola P, Giuliani F, Coscia A, Varalda A, Occhi L, et al. Evaluation of postnatal growth of preterm infants. J Matern Fetal Neonatal Med 2011;24(Suppl 2): 9–11.


20. Camelo JS Jr, Martinez FE. Nutritional dilemmas in extremely low birth weight infants and their effects on childhood, adolescence and adulthood. J Pediatr (Rio J) 2005;81(1 Suppl): S33–S42.


21. Ong KK, Kennedy K, Castañeda-Gutiérrez E, Forsyth S, Godfrey KM, Koletzko B, et al. Postnatal growth in preterm infants and later health outcomes: a systematic review. Acta Paediatr 2015;104:974–986.



22. Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, Borawski E. Growth of very low birth weight infants to age 20 years. Pediatrics 2003;112(1 Pt 1): e30–e38.


23. Sung IK, Vohr B, Oh W. Growth and neurodevelopmental outcome of very low birth weight infants with intrauterine growth retardation: comparison with control subjects matched by birth weight and gestational age. J Pediatr 1993;123:618–624.


24. Park HJ, Lee HY, Woo HK, Kim SN, Lee J, Yang HR, et al. The usefulness of birth weight Z-Score as a predictor of catch up growth in preterm infants. Neonatal Med 2015;22:142–149.

25. Bertino E, Boni L, Rossi C, Coscia A, Giuliani F, Spada E, et al. Evaluation of postnatal growth in very low birth weight infants: a neonatologist's dilemma. Pediatr Endocrinol Rev 2008;6:9–13.

Fig. 1
Percentile of weight from birth to postconception age (PCA) 24 months according to the Korean growth chart. P, percentile.
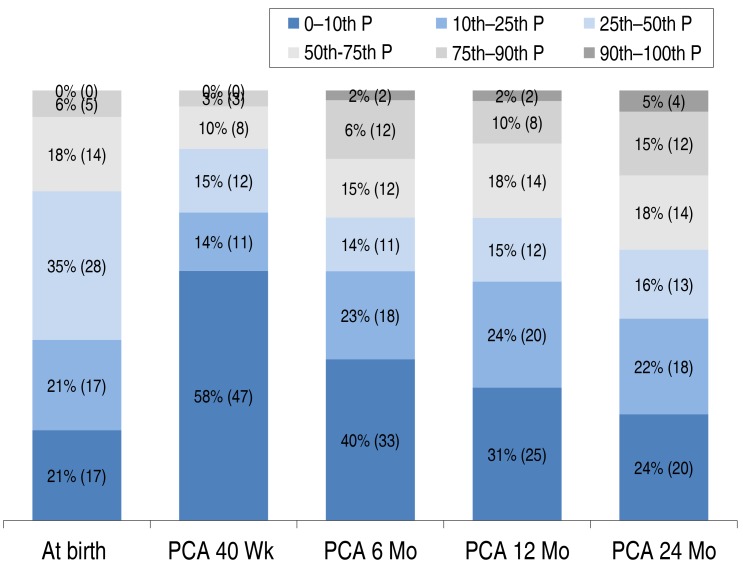
Fig. 2
Percentile of height from birth to postconception age (PCA) 24 months according to the Korean growth chart. P, percentile.

Fig. 3
Incidence of growth failure (<10th percentile) in the small-for-gestational age (SGA), appropriate-weight-for-gestational age (AGA), and very-low-birth-weight (VLBW) infants. PCA, postconception age.

Fig. 4
Incidence of growth failure(<10th percentile) in the extremely-low-birth-weight (ELBW) and non-ELBW infants with birth weights of 1,000 g–1,500 g. PCA, postconception age.
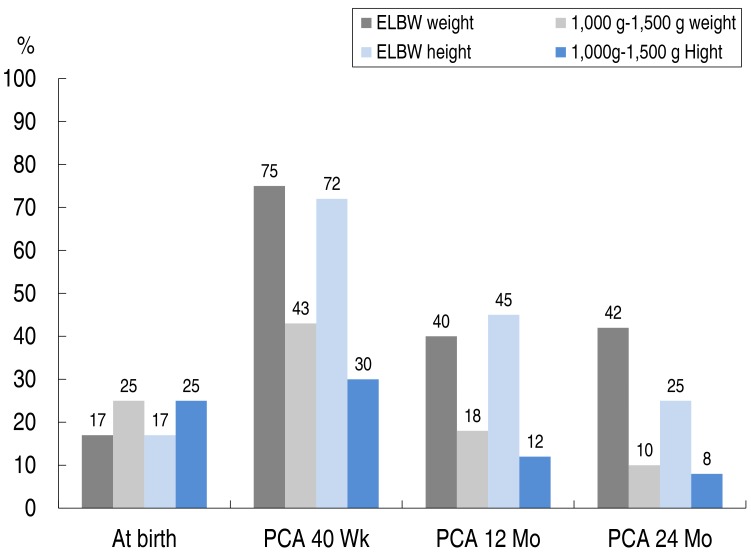
Fig. 5
Comparison of the weight (A) and height percentiles (B) by using the Korean, World Health Organization (WHO), and Centers for Disease Control and Prevention (CDC) standard charts. GA, gestational age.

Table 1
Patient characteristics (n=81)
| Characteristic | Value |
|---|---|
| Gestational age (wk) | 28.3±3.6 |
| Birth weight (g) | 1,137±335 |
| Male sex | 32 (38.9) |
| Apgar score | |
| 1 Minute | 2.5±1.7 |
| 5 Minutes | 5.4±1.4 |
| Hospital day (day) | 68.6±38.6 |



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


