Article Contents
| Clin Exp Pediatr > Volume 63(9); 2020 |
|
Abstract
Inflammatory bowel disease (IBD) is a chronic relapsing immune-mediated disease of the intestinal tract. Although its prevalence is reportedly lower in Asia than in Western countries, the rapid increase in the incidence of IBD has drawn attention to its etiology, including genetic susceptibility and environmental factors. Specifically, recent studies concerning dietary treatments and intestinal microbiota suggest that these factors may interact with the immune system, and the imbalance of this relationship may lead to immune dysregulation in IBD. Changes in diet or alterations in the composition of the intestinal microbiota may be associated with the increasing incidence of IBD in Asia. Here, we aim to review recent studies on the role of diet and intestinal microbiota in IBD pathogenesis and the results of the investigations performed to modulate these factors.
Inflammatory bowel disease (IBD), including Crohn disease (CD) and ulcerative colitis (UC), is an immune-mediated chronic relapsing inflammatory condition that mainly affects the gastrointestinal tract.
The incidence and prevalence of IBD is increasing globally. Although reportedly higher in Western countries, a similar trend is now being observed in Asia as well. The prevalences of CD and UC in Canada in 2008 were 255.2 per 100,000 (95% confidence interval [CI], 252.4–258.0) and 259.7 per 100,000 (95% CI, 256.9–262.5), respectively, while the prevalences of CD and UC in the commercially-insured in the commercially-insured adult population in United States during 2008–2009 were 241.3 (95% CI, 238.1–244.5) and 263.0 (95% CI, 259.7–266.4) per 100,000, respectively [1,2]. In European studies, prevalences as high as those in North America have been reported [3]. Unlike in Western countries, epidemiologic data for IBD in Asia are relatively lacking, but the prevalence of IBD in these areas is thought to be lower. In a Japanese study, the prevalences of CD and UC in 2005 were 21.2 (95% CI, 20.8–21.7) and 63.6 (95% CI, 62.8–64.4) per 100,000, respectively [4]. In South Korea, the adjusted prevalences of CD and UC per 100,000 in 2005 were 11.24 (95% CI, 9.29–13.18) and 30.87 (95% CI, 27.47–34.27), respectively [5]. However, according to Korean cohort studies, the mean annual incidence seems to have increased by more than 100-fold for both CD and UC in the past 20 years [5].
Increasing occurrences are also being seen in pediatric patients. From 1994 to 2009, the incidence of IBD in children increased from 9.4 per 100,000 (95% CI, 8.2–10.8) to 13.2 per 100,000 (95% CI, 11.9–14.6) (P<0.0001) [6].
Various factors seem to contribute to the increasing global incidence of IBD, including an increased awareness of the disease, more developed disease surveillance systems, improved accessibility to hospitals and health care providers, and lifestyle changes toward a Westernized environment [7]. Although genetic factors appear to play an important role in the pathogenesis of IBD as shown in Swedish cohort studies on identical twins, environmental changes over the past few decades have been among the important factors increasing the incidence of IBD in Asia [3,8,9]. This is supported by the higher incidence of illness among immigrants who migrate from countries with a low incidence to Western countries [10].
The environmental changes and subsequent alterations to the intestinal microbiota are considered important in the increased prevalence of IBD in Asia. Therapeutic approaches involving these factors demonstrating efficacy in recent studies also support this proposition [11-17]. In this review, we will discuss the environmental, nutritional, and microbial factors that contribute to the pathogenesis of IBD as well as therapeutic approaches to modulate these factors.
Dietary patterns and nutritional factors are considered important environmental factors in the etiology of IBD, and the Western diet has long been suspected of contributing to the development of IBD [10]. This diet is characterized by high levels of fats and refined sugars and low levels of fiber and vegetables. Several studies, although many were animal studies, have shown that the Western diet is associated with increased levels of proinflammatory cytokines, modulated intestinal permeability, and altered composition of the intestinal microbiota that promote chronic inflammation in the gut [18-21].
Sakamoto et al. [22] found a positive association between sugar consumption and CD risk (odds ratio [OR], 2.83; 95% CI, 1.38–5.83) and UC (OR, 2.86; 95% CI, 1.24–6.57). This supports views on the detrimental effects of refined carbohydrates and sweetened beverages in the Western diet on IBD. On the contrary, complex carbohydrates and fiber-rich vegetables and fruits are thought to be beneficial [23]. Haskey et al. showed that a high protein intake, especially from animal protein, resulted in a 3.3-time increased risk of IBD, suggesting that a diet high in animal protein was a major risk factor [23]. With respect to the intake of dietary fats, a high n-3 polyunsaturated fatty acid (PUFA) to n-6 PUFA ratio is reportedly inversely associated with the risk of IBD [23-25].
Several studies have shown the influence of certain components contained in food on epithelial cell permeability. For example, Söderholm et al. [26,27] found that sodium caprate, a medium-chain fatty acid in dairy products, increased the intestinal per me ability in the ilea of rats and humans, more noticeably in those with CD. Lammers et al. [28] proved that gliadin, the toxic component of gluten that initiates the inflammatory response in celiac disease binds to C-X-C motif chemokine receptor 3 in the small intestine epithelium to increase zonulin release in a myeloid-differentiating primary-response 88-dependent manner and subsequently increases intestinal permeability. Increased intestinal perme ability is associated with a defective mucosal barrier, which exposes the luminal bacteria and their products to the mucosa. An influx of the luminal contents to the intestinal mucosa triggers immune cell activation and cytokine production and secretion [29].
Aside from the nutritional food components, food additives such as detergents and emulsifiers may be associated with defective barrier function [30]. Chassaing et al. [31] documented in an animal study that chronic exposure to carboxymethylcellulose, a widely used cellulose derivative used as a viscosity modifier in a variety of dairy products, sauces, and sausages, increased bacterial adherence to the intestinal epithelium, particularly proinflammatory microbiota. Another food emulsifier common ly used in processed food, polysorbate-80, increased the translocation of Escherichia coli across M cells and Peyer’s patches in patients with CD [32].
The human microbiota consists of about 1,014 diverse microbes, primarily in the colon [33]. The gut microbiota affects human health by performing many roles in metabolite synthe sis, barrier function, and immune responses [34]. There is an interaction between the gut microbiota and the host immune system; when this balanced relationship is disrupted, gut microbial composition changes occur that consequently aggravate permeability dysfunction [35]. This, in turn, further aggravates alteration of the microbial composition, i.e., dysbiosis, to which a chronic inflammatory response occurs in the host immune system.
The intestinal microbiota is also known to have an important role in the pathogenesis of IBD [36]. Many studies have shown lower microbial diversity and a higher microbial dysbiosis index in IBD patients compared to healthy controls. Moreover, a long-term follow-up study of fecal microbiota in patients with IBD showed that the microbial profiles of IBD patients are different from those of healthy controls, and high volatility was observed in IBD patients [37].
Some specific changes in the intestinal microbiota of IBD patients have been identified, such as decreases in Roseburia hominis and Faecalibacterium prausnitzii, butyrate-producing species [38]. There are reports of an increased amount of Enterobacteriaceae and a reduced number of Clostridium clusters IV and XVIa during disease-associated inflammation in newly diagnosed CD patients [39]. Increases in Escherichia coli, Fusobacterium, and Proteus as well as decreases in Firmicutes such as Faecalibacterium prausnitzii have also been reported [3].
In newly diagnosed pediatric IBD patients, an increased amount of Proteobacteria and a decrease in Faecalibacterium prausnitzii in the intestinal microbiota seem to be associated with complicated disease phenotypes and a subsequent need for biologic therapy or surgery [40].
Colonization of the gut begins at birth, and the gut microbiota become more stable and develop adult-like complexity during the first year of life [41]. Various environmental factors, such as diet, are known to contribute to this phenomenon, which begins very early in life. A higher proportion of Bifidobacteria was found in breastfed than formula-fed infants [42]. As previously mentioned, dietary patterns are associated with the pathogenesis of IBD and are related to the intestinal microbiota. In a mouse model, mice fed a high-fat diet demonstrated dysbiosis characterized by an increase in Proteobacteria and decrease in Firmicutes, similar to that observed in CD [43]. A high-fat diet results in the accumulation of secondary bile acids, which in turn can inhibit the growth of the Bacteroidetes and Firmicutes phyla, a common dysbiotic feature found in CD [44].
These varied evidences suggest that the dietary pattern influences the composition of the intestinal microbiota; through this indirect mechanism, diet can determine subsequent intestinal inflammation (Fig. 1).
Exclusive enteral nutrition (EEN) is the only evidence-based dietary treatment for IBD. EEN involves a completely liquid diet without any normal dietary components for a certain duration. It is used as a therapeutic method to induce remission in pediatric patients with active CD [45].
According to a meta-analysis, EEN is as effective as corticosteroids at inducing remission in pediatric CD patients. This is true for newly diagnosed CD and relapsed cases (OR, 0.76; 95% CI, 0.29–1.98). Furthermore, EEN was more effective than corticosteroids with respect to mucosal healing (OR, 4.5; 95% CI, 1.64–12.32) [46]. Based on these results, the European Crohn’s and Colitis Organization and the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) consensus guidelines on the medical management of pediatric CD recommended EEN as the first-line therapy to induce remission in children with active luminal CD [47]. Although its mechanisms are not yet fully understood, there is some evidence that EEN reinforces the epithelial barrier; accordingly, bacterial invasion into the mucosa is prevented. Moreover, strengthening the barrier can restore intestinal microbial dysbiosis and affect the dysregulated immune system by decreasing pro-inflammatory cytokines as well as the local action of anti-inflammatory cytokines. In this way, EEN is thought to improve inflammation in CD [48].
Despite the safety and efficacy of EEN for inducing remission in pediatric CD patients, intolerance of or poor adherence to is the main hindrance to implementing this therapeutic method [49]. A recent randomized clinical trial by Levine et al. [11] showed that the combination of the Crohn disease exclusion diet (CDED) and partial enteral nutrition (PEN) induced sustained remission at week 12 compared to EEN (75.6% and 45.1%, respectively, P=0.01). Moreover, significantly higher tolerance was noted in patients who received CDED with PEN than those treated with EEN (97.5% and 73.7% respectively, P=0.002).
Table 1 shows various attempts to develop a new dietary treatment method for IBD to target the modulation of intestinal microbiota or the immune system itself [11,50-60]. However, there is insufficient evidence to propose a recommendation. A recent position paper on behalf of the Porto Inflammatory Bowel Disease Group of the ESPGHAN also stated that “elimination or restrictive diet in children/adolescents with IBD should not be recommended unless potential benefits outweigh potential risks of the diet [61].”
Ever since intestinal microorganisms were known to attribute to the pathogenesis of IBD, efforts have been made to restore the altered microbial composition. The administration of probiotics and prebiotics as IBD treatment has obtained inconsistent results [21].
Probiotics are defined as live microorganisms that are beneficial to the host’s health when ingested in adequate amounts. Derived from commensal microbiota, they mimic the homeostatic effect of intestinal microbiota in the healthy condition. They affect the mucosal immune system by balancing pro- and anti-inflammatory components, alter the microbial composition by inhibiting pathogenic bacteria, and enhance barrier function [62-65].
Although many probiotics demonstrated limited efficacy in UC, the probiotic cocktail VSL#3 and Escherichia coli Nissle 1917 reduced active inflammation in many studies [66-69]. They were associated with increased mucosal regulatory T cells, reduced pro-inflammatory cytokines, increased microbial diversity, and restored barrier integrity. However, they showed no statistically significant impact for treating CD [70,71]. In addition, several microbes such as Faecalibacterium prausnitzii and Bacteroides fragilis have been studied for their therapeutic poten tial as they seem to reduce colitis severity in many mouse models [72-74].
As shown above, some taxa seem to be associated with the disease course of IBD by interacting with the immune system [38-40]. However, the changes of specific microbiota that increase the risk of IBD are not completely clear. Therefore, it is important to manipulate specific microbiota and enhance the overall environment of beneficial microorganisms. Moreover, the fact that dietary modification affects the disease course of IBD also suggests the significance of prebiotics as a nutrient source for the microbiota.
Prebiotics are nondigestible food components fermented by microbiota that benefit the host. By providing essential food to the microbiota, prebiotics can modify the gut microbial com position and subsequent metabolites. For instance, oligosaccharides and fibers induce the proliferation of short-chain fatty acid-producing bacteria, such as the Bacteroides genus, to improve colitis severity in IBD [75,76]. Many in vitro and animal studies also confirmed that prebiotics helped alleviate colitis severity by altering the microbial composition, production of short-chain fatty acids such as butyrate, and balances in pro- and anti-inflammatory cytokines [77-80].
Several human studies have confirmed the efficacy of prebiotics in IBD patients, but the results are controversial. Lindsay et al. showed a reduced disease activity index and increased mucosal Bifidobacteria when CD patients were provided with 15 g of fructooligosaccharides (FOS) [81]. However, a randomized trial conducted by Benjamin et al. [82] showed no significant improvement in disease activity in a population that received FOS, although it demonstrated an increase in interleukin (IL)-10-producing dendritic cells (DCs) and decrease in IL-6-producing DCs. Other than FOS, germinated barley foodstuff, Ispaghula husk, and a combination of oligofructose and inulin demonstrated the potential to induce remission or reduce in flammation in UC patients, while inulin showed its efficacy in pouchitis patients as well [83-86].
As describe above, probiotics and prebiotics are thought to play distinct roles in immune system regulation. Although they are considered feasible armamentaria in the modulation of intestinal microbiota and possible treatment options for IBD, many clinical trials on this subject are tremendously heterogeneous in study design, mode of administration, and used probiotics or prebiotics to lead to a firm conclusion. Therefore, further well-designed studies of larger populations are needed to determine which probiotics or prebiotics effectively treat IBD.
Fecal microbiota transplantation (FMT) is another approach to modulating the intestinal microbiota. FMT is considered the most direct method to manipulate the intestinal microbiota profile, and there is much ongoing research regarding FMT as a potential treatment for IBD.
As the first case of FMT in pseudomembranous colitis was reported several decades ago, FMT has been well studied and proven as an effective and safe treatment for refractory or recurrent Clostridium difficile infection [87]. This has stimulated research in FMT for other diseases related to dysbiosis, including IBD.
Although there are no available randomized controlled trials (RCTs) of CD patients, 6 uncontrolled cohort studies were reported with controversial results [12]. Vermeire et al. [13] reported a 0% remission rate among patients with moderate to severe CD, whereas Cui et al. [14] reported a 76.7% clinical remission rate after 4 weeks of FMT. Although a meta-analysis of the 6 pooled cohort studies showed a clinical remission rate of 52%, RCTs with a larger number of patients are needed to ensure the efficacy of FMT in CD patients [88].
In contrast to CD, larger RCTs have been performed in UC patients. A clinical remission rate of 24%–50% was reported in an FMT group; in 3 of 4 studies, remission rates were significantly higher in the FMT group than in the control group [15-17,88]. A meta-analysis of 4 RCTs also showed a significant benefit in clinical remission (pooled OR, 2.89; 95% CI, 1.36–6.13; P=0.006) [88]. Subsequently, the American Gastroenterological Association stated the efficacy of FMT for inducing remission in mild to moderate UC [89].
In pediatric patients, there are no published RCTs, but 6 cohort studies assessing 34 UC patients and 2 cohort studies assessing 13 CD patients showed a pooled estimated clinical remission rate of 23% (95% CI, 7%–51%) in UC and 54% (95% CI, 28%–78%) in CD patients [88]. The clinical trials and their results of FMT in pediatric IBD patients are summarized in Table 2 [90-100].
When there was a thorough investigation of donor fecal material, FMT has been considered a relatively safe treatment modality with a low rate of adverse events. Any reported side effects were mild and self-limiting [101]. Although serious adverse events (SAEs) such as flares were reported in several studies, a recent meta-analysis showed no significant difference between the FMT and the control groups with respect to SAEs. The pooled rate of SAEs was 7.1% in the FMT group versus 5.1% in the control group with no significant difference (risk ratio adverse events, 1.40; 95% CI, 0.55–3.58; P=0.49) [102].
FMT can be considered a relatively safe and effective treatment option for IBD that modulates the intestinal microbiota. However, several factors affecting FMT outcome and efficacy remain to be determined, including pretreatment, dosage and frequency, preparation of donor stools, and routes of administration. Further studies are needed to increase our understanding of and optimize FMT in IBD [12].
Numerous environmental factors can contribute to the increasing incidence of IBD. Of them, dietary and nutritional factors play an important role in the pathophysiology directly or through changes to the intestinal microbiota. In this “biologic era” in which a variety of new potent medications is being used, modifying causative environmental factors is still expected to play a more fundamental role in treating and preventing IBD. To increase our understanding of IBD, it is necessary to focus on the medical management and elucidate the environmental factors such as dietary treatment and FMT.
Fig. 1.
Relationship between diet, intestinal microbiota, and inflammatory bowel disease (IBD). Genetic susceptibility, diet, and microbial composition contribute to the incidence of inflammatory bowel disease. Inflammatory bowel disease itself and its severity are responsible for the microbial composition; conversely, dysbiosis is also thought to affect inflammatory bowel disease.
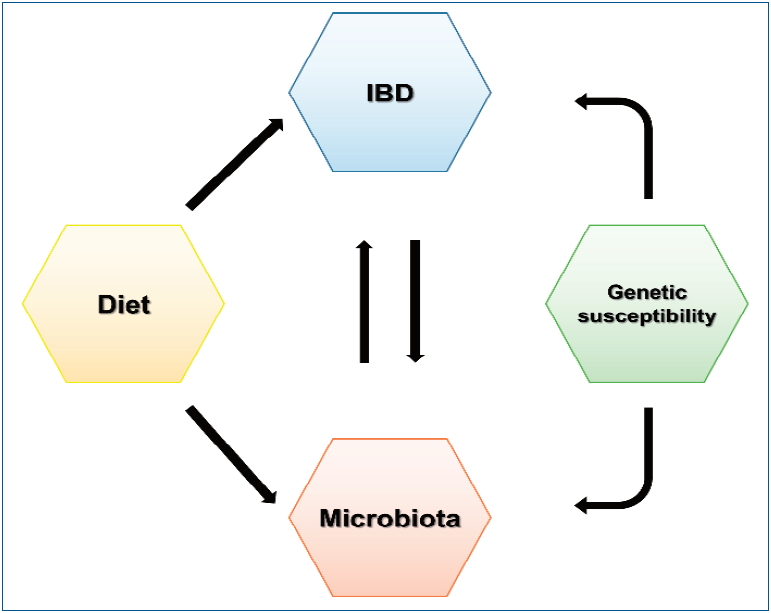
Table 1.
Summary of the various dietary treatments for IBD other than EEN
Table 2.
Clinical trials of fecal microbiota transplantation in pediatric IBD
| Heading | Author | No. of patients | Severity | Route | Donor | Fresh/frozen | Frequency | Clinical remission | Clinical response | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| UC | Kunde et al., 2013 [90] | 10 | Mild-Moderate (PUCAI 15–65) | Enema | Related and unrelated | Fresh | 5 Consecutive days | Week 1: 3/9 (33%) | Week 1: 7/9 (78%) | 4 Weeks |
| Week 4: 3/9 (33%) | Week 4: 6/9 (67%) | |||||||||
| Kellermayer et al., 2015 [91] | 3 | Immunotherapy dependent but controlled (Mayo 0–1) | Colonoscopy followed by enemas | Unrelated | Frozen | 22–30 (daily for fortnight, thrice weekly for fortnight, then weekly for 6–12 weeks) | 3/3 (100%) | - | 3 Months | |
| Vandenplas et al., 2015 [92] | 1 | Severe (PUCAI 60–75) | Colonoscopy first 2 infusions | Related | Fresh | 7 times (interval not shown) | 1 | - | 6 Months | |
| Nasoduodenal tube next 5 infusions | ||||||||||
| Suskind et al., 2015 [94] | 4 | Mild–moderate (PUCAI 20–55) | Nasogastrtuc tube | NR | Fresh | Single | 0 | 0 | 12 Weeks | |
| Shimizu et al., 2016 [96] | 1 | Severe, steroid dependent UC | Colonoscopy first 1 infusion | Related | Fresh | 16 Times for 10 months | 1 | 0 | 10 Months | |
| Enema next 4 infusions (5–day course), then 11 infusions for 10 months/ | ||||||||||
| Pai et al., 2016 [95] | 2 | Active | Unrelated | Enemas | Frozen | 12 Times (biweekly for 6 weeks) | 0 | 0 | NR | |
| Kumagai et al., 2016 [96] | 1 | Severe (PUCAI 85) | Enema first 2 infusions, Nasoduodenal tube next 4 infusions | Related | Fresh | 6 Times within 10 days | 0 (Required colectomy) | 0 | 3 Months | |
| Karolewska Bochenek et al., 2018 [97] | 8 | Moderate-Severe (PUCAI 15–70) | Gastroscopy or Nasoduodenal tube | Unrelated | NR | 5 Consecutive days | 3/8 (37.5%) | 7/8 (87.5%) | 4 Weeks | |
| 3 Days alternatively | ||||||||||
| Goyal et al., 2018 [98] | 12 | Mild-moderate (PUCAI <65) | Both gastroscopy (20–30 mL) and colonoscopy (200–250 mL) | Related and unrelated | Fresh | Single | 6 Months: 0/14 (0%) | 1 Month: 7/14 (50 %) | 6 Months | |
| 6 Months: 3/14 (21.4 %) | ||||||||||
| Yodoshi et al., 2018 [99] | 2 | Severe refractory UC | Colonoscopy for one patient, and Nasoduodenal tube for another (As desired) | Related | Fresh | 5 Consecutive days | Week 3: 2/2 | - | 2 Years | |
| Week 4: 1/2 (1 had undergone colectomy) | ||||||||||
| CD | Suskind et al., 2015 [100] | 9 | Mild-moderate (PCDAI 10–29) | Nasogastrtuc tube | Related | Fresh | Single | Week 2: 7/9 (78%) | NR | 12 Weeks |
| Week 6&12: 5/9 (56%) | ||||||||||
| Karolewska Bochenek et al., 2018 [97] | 2 | Moderatesevere (PCDAI 15–37.5) | Gastroscopy or nasoduodenal tube | Unrelated | NR | 5 Consecutive days | 2/2 (100%) | 2/2 (100%) | 4 Weeks | |
| 3 Days alternatively | ||||||||||
| Goyal et al., 2018 [98] | 4 | Mild-moderate (PCDAI<40) | Both gastroscopy (20–30 mL) and colonoscopy (200–250 mL) | Related and unrelated | Fresh | Single | 6 Months: 2/7 (28.6 %) | 1 Month: 5/7 (71%) | 6 Months | |
| 6 Months: 3/7 (43 %) |
References
1. Benchimol EI, Manuel DG, Guttmann A, Nguyen GC, Mojaverian N, Quach P, et al. Changing age demographics of inflammatory bowel disease in Ontario, Canada: a population-based cohort study of epidemiology trends. Inflamm Bowel Dis 2014;20:1761–9.


2. Kappelman MD, Moore KR, Allen JK, Cook SF. Recent trends in the prevalence of Crohn's disease and ulcerative colitis in a commercially insured US population. Dig Dis Sci 2013;58:519–25.


3. Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology 2017;152:313–21. e2.


4. Asakura K, Nishiwaki Y, Inoue N, Hibi T, Watanabe M, Takebayashi T. Prevalence of ulcerative colitis and Crohn's disease in Japan. J Gastroenterol 2009;44:659–65.



5. Yang SK, Yun S, Kim JH, Park JY, Kim HY, Kim YH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis 2008;14:542–9.


6. Benchimol EI, Mack DR, Nguyen GC, Snapper SB, Li W, Mojaverian N, et al. Incidence, outcomes, and health services burden of very early onset inflammatory bowel disease. Gastroenterology 2014;147:803–13. e7; quiz e14-5.


7. Sartor RB. Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol 2006;3:390–407.



8. Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol 2015;12:720–7.



9. Halfvarson J, Bodin L, Tysk C, Lindberg E, Järnerot G. Inflammatory bowel disease in a Swedish twin cohort: a long-term follow-up of concordance and clinical characteristics. Gastroenterology 2003;124:1767–73.


10. Legaki E, Gazouli M. Influence of environmental factors in the development of inflammatory bowel diseases. World J Gastrointest Pharmacol Ther 2016;6(7): 112–25.

11. Levine A, Wine E, Assa A, Sigall Boneh R, Shaoul R, Kori M, et al. Crohn's disease exclusion diet plus partial enteral nutrition induces sus tained remission in a randomized controlled trial. Gastroenterology 2019;157:440–50. e8.


12. Jeon SR, Chai J, Kim C, Lee CH. Current evidence for the management of inflammatory bowel diseases using fecal microbiota transplantation. Curr Infect Dis Rep 2018;20:21



13. Vermeire S, Joossens M, Verbeke K, Wang J, Machiels K, Sabino J, et al. Donor species richness determines faecal microbiota transplantation success in inflammatory bowel disease. J Crohns Colitis 2016;10:387–94.



14. Cui B, Feng Q, Wang H, Wang M, Peng Z, Li P, et al. Fecal microbiota transplantation through mid-gut for refractory Crohn's disease: safety, feasibility, and efficacy trial results. J Gastroenterol Hepatol 2015;30:51–8.


15. Paramsothy S, Kamm MA, Kaakoush NO, Walsh AJ, van den Bogaerde J, Samuel D, et al. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet 2017;389:1218–28.


16. Moayyedi P, Surette MG, Kim PT, Libertucci J, Wolfe M, Onischi C, et al. Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology 2015;149:102–9. e6.


17. Rossen NG, Fuentes S, van der Spek MJ, Tijssen JG, Hartman JH, Duflou A, et al. Findings from a randomized controlled trial of fecal transplantation for patients with ulcerative colitis. Gastroenterology 2015;149:1108e4.

18. Huang EY, Devkota S, Moscoso D, Chang EB, Leone VA. The role of diet in triggering human inflammatory disorders in the modern age. Microbes Infect 2013;15:765–74.


19. Agus A, Denizot J, Thévenot J, Martinez-Medina M, Massier S, Sauvanet P, et al. Western diet induces a shift in microbiota composition enhancing susceptibility to Adherent-Invasive E. coli infection and intestinal inflammation. Sci Rep 2016;6:19032



20. Statovci D, Aguilera M, MacSharry J, Melgar S. The impact of western diet and nutrients on the microbiota and immune response at mucosal interfaces. Front Immunol 2017;8:838



21. Zuo T, Ng SC. The gut microbiota in the pathogenesis and therapeutics of inflammatory bowel disease. Front Microbiol 2018;9:2247



22. Sakamoto N, Kono S, Wakai K, Fukuda Y, Satomi M, Shimoyama T, et al. Dietary risk factors for inflammatory bowel disease: a multicenter case-control study in Japan. Inflamm Bowel Dis 2005;11:154–63.


23. Haskey N, Gibson DL. An Examination of diet for the maintenance of remission in inflammatory bowel disease. Nutrients 2017;9:259



24. Hou JK, Abraham B, El-Serag H. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol 2011;106:563–73.



25. John S, Luben R, Shrestha SS, Welch A, Khaw KT, Hart AR. Dietary n-3 polyunsaturated fatty acids and the aetiology of ulcerative colitis: a UK prospective cohort study. Eur J Gastroenterol Hepatol 2010;22:602–6.


26. Söderholm JD, Oman H, Blomquist L, Veen J, Lindmark T, Olaison G. Reversible increase in tight junction permeability to macromolecules in rat ileal mucosa in vitro by sodium caprate, a constituent of milk fat. Dig Dis Sci 1998;43:1547–52.


27. Söderholm JD, Olaison G, Peterson KH, Franzén LE, Lindmark T, Wirén M, et al. Augmented increase in tight junction permeability by luminal stimuli in the non-inflamed ileum of Crohn's disease. Gut 2002;50:307–13.



28. Lammers KM, Lu R, Brownley J, Lu B, Gerard C, Thomas K, et al. Gliadin induces an increase in intestinal permeability and zonulin release by binding to the chemokine receptor CXCR3. Gastroenterology 2008;135:194–204. e3.



30. Swidsinski A, Ung V, Sydora BC, Loening-Baucke V, Doerffel Y, Verstraelen H, et al. Bacterial overgrowth and inflammation of small intestine after carboxymethylcellulose ingestion in genetically susceptible mice. Inflamm Bowel Dis 2009;15:359–64.


31. Chassaing B, Koren O, Goodrich JK, Poole AC, Srinivasan S, Ley RE, et al. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 2015;519:92–6.




32. Roberts CL, Keita AV, Duncan SH, O'Kennedy N, Söderholm JD, Rhodes JM, et al. Translocation of Crohn's disease Escherichia coli across M-cells: contrasting effects of soluble plant fibres and emulsifiers. Gut 2010;59:1331–9.



33. Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010;464:59–65.




34. Prakash S, Rodes L, Coussa-Charley M, Tomaro-Duchesneau C. Gut microbiota: next frontier in understanding human health and development of biotherapeutics. Biologics 2011;5:71–86.



35. Kamada N, Seo SU, Chen GY, Núñez G. Role of the gut microbiota in immunity and inflammatory disease. Nat Rev Immunol 2013;13:321–35.



36. De Cruz P, Prideaux L, Wagner J, Ng SC, McSweeney C, Kirkwood C, et al. Characterization of the gastrointestinal microbiota in health and inflammatory bowel disease. Inflamm Bowel Dis 2012;18:372–90.


37. Halfvarson J, Brislawn CJ, Lamendella R, Vázquez-Baeza Y, Walters WA, Bramer LM, et al. Dynamics of the human gut microbiome in inflammatory bowel disease. Nat Microbiol 2017;2:17004




38. Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology 2014;146:1489–99.



39. Gevers D, Kugathasan S, Denson LA, Vázquez-Baeza Y, Van Treuren W, Ren B, et al. The treatment-naive microbiome in new-onset Crohn's disease. Cell Host Microbe 2014;15:382–92.



40. Olbjørn C, Cvancarova Småstuen M, Thiis-Evensen E, Nakstad B, Vatn MH, Jahnsen J, et al. Fecal microbiota profiles in treatment-naïve pediatric inflammatory bowel disease - associations with disease phenotype, treatment, and outcome. Clin Exp Gastroenterol 2019;12:37–49.



41. Palmer C, Bik EM, DiGiulio DB, Relman DA, Brown PO. Development of the human infant intestinal microbiota. Version 2. PLoS Biol 2007;5:e177.



43. Lai KP, Chung YT, Li R, Wan HT, Wong CK. Bisphenol A alters gut microbiome: Comparative metagenomics analysis. Environ Pollut 2016;218:923–30.


44. Islam KB, Fukiya S, Hagio M, Fujii N, Ishizuka S, Ooka T, et al. Bile acid is a host factor that regulates the composition of the cecal microbiota in rats. Gastroenterology 2011;141:1773–81.


45. Day AS, Lopez RN. Exclusive enteral nutrition in children with Crohn's disease. World J Gastroenterol 2015;21:6809–16.



46. Swaminath A, Feathers A, Ananthakrishnan AN, Falzon L, Li Ferry S. Systematic review with meta-analysis: enteral nutrition therapy for the induction of remission in paediatric Crohn's disease. Aliment Pharmacol Ther 2017;46:645–56.



47. Ruemmele FM, Veres G, Kolho KL, Griffiths A, Levine A, Escher JC, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn's disease. J Crohns Colitis 2014;8:1179–207.



48. Ashton JJ, Gavin J, Beattie RM. Exclusive enteral nutrition in Crohn's disease: Evidence and practicalities. Clin Nutr 2019;38:80–9.


49. de Bie C, Kindermann A, Escher J. Use of exclusive enteral nutrition in paediatric Crohn's disease in The Netherlands. J Crohns Colitis 2013;7:263–70.



50. Damas OM, Garces L, Abreu MT. Diet as adjunctive treatment for inflammatory bowel disease: review and update of the latest literature. Curr Treat Options Gastroenterol 2019;17:313–25.




51. Gunasekeera V, Mendall MA, Chan D, Kumar D. Treatment of Crohn's disease with an IgG4-guided exclusion diet: a randomized controlled trial. Dig Dis Sci 2016;61:1148–57.



52. Olendzki BC, Silverstein TD, Persuitte GM, Ma Y, Baldwin KR, Cave D. An anti-inflammatory diet as treatment for inflammatory bowel disease: a case series report. Nutr J 2014;13:5




53. Sigall-Boneh R, Pfeffer-Gik T, Segal I, Zangen T, Boaz M, Levine A. Partial enteral nutrition with a Crohn's disease exclusion diet is effective for induction of remission in children and young adults with Crohn's disease. Inflamm Bowel Dis 2014;20:1353–60.


54. Svolos V, Hansen R, Nichols B, Quince C, Ijaz UZ, Papadopoulou RT, et al. Treatment of active Crohn's disease with an ordinary food-based diet that replicates exclusive enteral nutrition. Gastroenterology 2019;156:1354–67. e6.


55. Obih C, Wahbeh G, Lee D, Braly K, Giefer M, Shaffer ML, et al. Specific carbohydrate diet for pediatric inflammatory bowel disease in clinical practice within an academic IBD center. Nutrition 2016;32:418–25.


56. Cohen SA, Gold BD, Oliva S, Lewis J, Stallworth A, Koch B, et al. Clinical and mucosal improvement with specific carbohydrate diet in pediatric Crohn disease. J Pediatr Gastroenterol Nutr 2014;59:516–21.


57. Suskind DL, Wahbeh G, Cohen SA, Damman CJ, Klein J, Braly K, et al. Patients perceive clinical benefit with the specific carbohydrate diet for inflammatory bowel disease. Dig Dis Sci 2016;61:3255–60.



58. Suskind DL, Wahbeh G, Gregory N, Vendettuoli H, Christie D. Nutritional therapy in pediatric Crohn disease: the specific carbohydrate diet. J Pediatr Gastroenterol Nutr 2014;58:87–91.


59. Rajendran N, Kumar D. Food-specific IgG4-guided exclusion diets improve symptoms in Crohn's disease: a pilot study. Colorectal Dis 2011;13:1009–13.


60. Zhan YL, Zhan YA, Dai SX. Is a low FODMAP diet beneficial for patients with inflammatory bowel disease? A meta-analysis and systematic review. Clin Nutr 2018;37:123–9.


61. Miele E, Shamir R, Aloi M, Assa A, Braegger C, Bronsky J, et al. Nutrition in pediatric inflammatory bowel disease: a position paper on behalf of the porto inflammatory bowel disease group of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2018;66:687–708.


62. Petrof EO, Kojima K, Ropeleski MJ, Musch MW, Tao Y, De Simone C, et al. Probiotics inhibit nuclear factor-kappaB and induce heat shock proteins in colonic epithelial cells through proteasome inhibition. Gastroenterology 2004;127:1474–87.


63. McCarthy J, O'Mahony L, O'Callaghan L, Sheil B, Vaughan EE, Fitzsimons N, et al. Double blind, placebo controlled trial of two probiotic strains in interleukin 10 knockout mice and mechanistic link with cytokine balance. Gut 2003;52:975–80.



64. O'Mahony C, Scully P, O'Mahony D, Murphy S, O'Brien F, Lyons A, et al. Commensal-induced regulatory T cells mediate protection against pathogen-stimulated NF-kappaB activation. PLoS Pathog 2008;4:e1000112.



65. Vindigni SM, Zisman TL, Suskind DL, Damman CJ. The intestinal microbiome, barrier function, and immune system in inflammatory bowel disease: a tripartite pathophysiological circuit with implications for new therapeutic directions. Therap Adv Gastroenterol 2016;9:606–25.



66. Miele E, Pascarella F, Giannetti E, Quaglietta L, Baldassano RN, Staiano A. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am J Gastroenterol 2009;104:437–43.


67. Tursi A, Brandimarte G, Papa A, Giglio A, Elisei W, Giorgetti GM, et al. Treatment of relapsing mild-to-moderate ulcerative colitis with the probiotic VSL#3 as adjunctive to a standard pharmaceutical treatment: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol 2010;105:2218–27.




68. Wehkamp J, Harder J, Wehkamp K, Wehkamp-von Meissner B, Schlee M, Enders C, et al. NF-kappaB- and AP-1-mediated induction of human beta defensin-2 in intestinal epithelial cells by Escherichia coli Nissle 1917: a novel effect of a probiotic bacterium. Infect Immun 2004;72:5750–8.



69. Schultz M. Clinical use of E. coli Nissle 1917 in inflammatory bowel disease. Inflamm Bowel Dis 2008;14:1012–8.


70. Malchow HA. Crohn's disease and Escherichia coli. A new approach in therapy to maintain remission of colonic Crohn's disease? J Clin Gastroenterol 1997;25:653–8.


71. Derwa Y, Gracie DJ, Hamlin PJ, Ford AC. Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease. Aliment Pharmacol Ther 2017;46:389–400.


72. Martín R, Miquel S, Chain F, Natividad JM, Jury J, Lu J, et al. Faecalibacterium prausnitzii prevents physiological damages in a chronic low-grade inflammation murine model. BMC Microbiol 2015;15:67




73. Round JL, Lee SM, Li J, Tran G, Jabri B, Chatila TA, et al. The Toll-like receptor 2 pathway establishes colonization by a commensal of the human microbiota. Science 2011;332:974–7.




74. Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux JJ, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci U S A 2008;105:16731–6.



75. Walker AW, Duncan SH, McWilliam Leitch EC, Child MW, Flint HJ. pH and peptide supply can radically alter bacterial populations and short-chain fatty acid ratios within microbial communities from the human colon. Appl Environ Microbiol 2005;71:3692–700.



76. Rasmussen HE, Hamaker BR. Prebiotics and Inflammatory Bowel Disease. Gastroenterol Clin North Am 2017;46:783–795.


77. Videla S, Vilaseca J, Antolín M, García-Lafuente A, Guarner F, Crespo E, et al. Dietary inulin improves distal colitis induced by dextran sodium sulfate in the rat. Am J Gastroenterol 2001;96:1486–93.


78. Lara-Villoslada F, Debras E, Nieto A, Concha A, Gálvez J, López-Huertas E, et al. Oligosaccharides isolated from goat milk reduce intestinal inflammation in a rat model of dextran sodium sulfate-induced colitis. Clin Nutr 2006;25:477–88.


79. Daddaoua A, Puerta V, Requena P, Martínez-Férez A, Guadix E, de Medina FS, et al. Goat milk oligosaccharides are anti-inflammatory in rats with hapten-induced colitis. J Nutr 2006;136:672–6.



80. Hoentjen F, Welling GW, Harmsen HJ, Zhang X, Snart J, Tannock GW, et al. Reduction of colitis by prebiotics in HLA-B27 transgenic rats is associated with microflora changes and immunomodulation. Inflamm Bowel Dis 2005;11:977–85.


81. Lindsay JO, Whelan K, Stagg AJ, Gobin P, Al-Hassi HO, Rayment N, et al. Clinical, microbiological, and immunological effects of fructooligosaccharide in patients with Crohn's disease. Gut 2006;55:348–55.



82. Benjamin JL, Hedin CR, Koutsoumpas A, Ng SC, McCarthy NE, Hart AL, et al. Randomised, double-blind, placebo-controlled trial of fructooligosaccharides in active Crohn's disease. Gut 2011;60:923–9.


83. Kanauchi O, Mitsuyama K, Homma T, Takahama K, Fujiyama Y, Andoh A, et al. Treatment of ulcerative colitis patients by long-term administration of germinated barley foodstuff: multi-center open trial. Int J Mol Med 2003;12:701–4.


84. Hallert C, Kaldma M, Petersson BG. Ispaghula husk may relieve gastro intestinal symptoms in ulcerative colitis in remission. Scand J Gastroenterol 1991;26:747–50.


85. Furrie E, Macfarlane S, Kennedy A, Cummings JH, Walsh SV, O'neil DA, et al. Synbiotic therapy (Bifidobacterium longum/Synergy 1) initiates resolution of inflammation in patients with active ulcerative colitis: a randomised controlled pilot trial. Gut 2005;54:242–9.



86. Welters CF, Heineman E, Thunnissen FB, van den Bogaard AE, Soeters PB, Baeten CG. Effect of dietary inulin supplementation on inflammation of pouch mucosa in patients with an ileal pouch-anal anastomosis. Dis Colon Rectum 2002;45:621–7.


87. Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery 1958;44:8549–9.
88. Paramsothy S, Paramsothy R, Rubin DT, Kamm MA, Kaakoush NO, Mitchell HM, et al. Faecal microbiota transplantation for inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis 2017;11:1180–99.



89. Singh S, Feuerstein JD, Binion DG, Tremaine WJ. AGA technical review on the management of mild-to-moderate ulcerative colitis. Gastroenterology 2019;156:769–808. e29.


90. Kunde S, Pham A, Bonczyk S, Crumb T, Duba M, Conrad H Jr, et al. Safety, tolerability, and clinical response after fecal transplantation in children and young adults with ulcerative colitis. J Pediatr Gastroenterol Nutr 2013;56:597–601.


91. Kellermayer R, Nagy-Szakal D, Harris RA, Luna RA, Pitashny M, Schady D, et al. Serial fecal microbiota transplantation alters mucosal gene expression in pediatric ulcerative colitis. Am J Gastroenterol 2015;110:604–6.




92. Vandenplas Y, Veereman G, van der Werff Ten Bosch J, Goossens A, Pierard D, Samsom JN, et al. Fecal microbial transplantation in early-onset colitis: caution advised. J Pediatr Gastroenterol Nutr 2015;61:e12–4.


93. Suskind DL, Singh N, Nielson H, Wahbeh G. Fecal microbial transplant via nasogastric tube for active pediatric ulcerative colitis. J Pediatr Gastroenterol Nutr 2015;60:27–9.


94. Shimizu H, Arai K, Abe J, Nakabayashi K, Yoshioka T, Hosoi K, et al. Repeated fecal microbiota transplantation in a child with ulcerative colitis. Pediatr Int 2016;58:781–5.


95. Pai N PJ, Lee C. A randomized, placebo-controlled trial of fecal microbial transplantation for pediatric ulcerative colitis [Pedifetch Trial]. J Pediatr Gastroenterol Nutr 2016;63:S79–80.
96. Kumagai H, Yokoyama K, Imagawa T, Inoue S, Tulyeu J, Tanaka M, et al. Failure of fecal microbiota transplantation in a three-year-old child with severe refractory ulcerative colitis. Pediatr Gastroenterol Hepatol Nutr 2016;19:214–20.



97. Karolewska-Bochenek K, Grzesiowski P, Banaszkiewicz A, Gawronska A, Kotowska M, Dziekiewicz M, et al. A two-week fecal microbiota transplantation course in pediatric patients with inflammatory bowel disease. Adv Exp Med Biol 2018;1047:81–7.


98. Goyal A, Yeh A, Bush BR, Firek BA, Siebold LM, Rogers MB, et al. Safety, Clinical Response, and Microbiome Findings Following Fecal Microbiota Transplant in Children With Inflammatory Bowel Disease. Inflamm Bowel Dis 2018;24:410–21.



99. Yodoshi T, Hurt TL. Fecal microbiota transplantation to patients with refractory very early onset ulcerative colitis. Pediatr Gastroenterol Hepatol Nutr 2018;21:355–60.



100. Suskind DL, Brittnacher MJ, Wahbeh G, Shaffer ML, Hayden HS, Qin X, et al. Fecal microbial transplant effect on clinical outcomes and fecal microbiome in active Crohn's disease. Inflamm Bowel Dis 2015;21:556–63.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


