Article Contents
| Clin Exp Pediatr > Volume 64(9); 2021 |
|
Abstract
Background
Purpose
Methods
Results
Acknowledgments
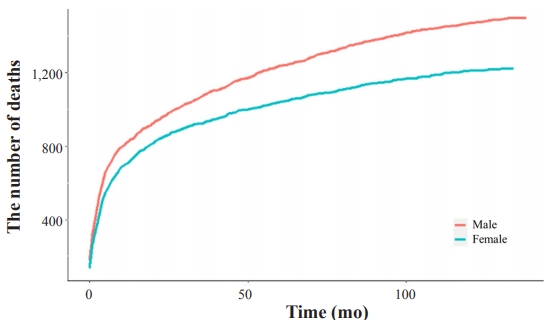
Fig. 2.

Table 1.
| Screening session | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| General health questionnaire | |||||||
| Safety accident prevention | √ | √ | √ | √ | √ | √ | √ |
| Prevention of SIDS | √ | ||||||
| Nutrition | √ | √ | √ | √ | √ | √ | √ |
| Sleep | √ | ||||||
| Vision | √ | √ | √ | √ | √ | √ | √ |
| Hearing | √ | √ | √ | √ | √ | √ | √ |
| Oral health guidance | √ | ||||||
| Toilet training | √ | ||||||
| Emotion | √ | ||||||
| Hygiene | √ | ||||||
| Preschool education | √ | ||||||
| Passive smoking | √ | ||||||
| Infection | √ | ||||||
| Developmental screeninga) | √ | √ | √ | √ | √ | √ | |
| Oral health questionnaire | √ | √ | √ | ||||
| Oral examination and guidance | √ | √ | √ | ||||
| Anthropometric exam | |||||||
| Height | √ | √ | √ | √ | √ | √ | √ |
| Weight | √ | √ | √ | √ | √ | √ | √ |
| Head circumference | √ | √ | √ | √ | √ | √ | √ |
| Vision acuity | √ | √ | √ | √ | |||
| Physical examination | √ | √ | √ | √ | √ | √ | √ |
| Anticipatory guidance | |||||||
| Accidents and poisoning | √ | √ | √ | √ | √ | √ | √ |
| Nutrition | √ | √ | √ | √ | √ | √ | √ |
| Sleep | √ | ||||||
| Oral health | √ | ||||||
| Toilet training | √ | ||||||
| Hygiene | √ | ||||||
| Passive smoking | √ |
Table 2.
Table 3.
| Characteristic | Birth in 2008 (n=469,248) | Birth in 2009 (n=448,459) |
|---|---|---|
| Sex | ||
| Boys | 241,752 (51.5) | 231,133 (51.5) |
| Girls | 227,496 (48.5) | 217,326 (48.5) |
| Birth weight (kg)a) | 3.19±0.46 | 3.18±0.46 |
| 500–999 g | 367 (0.09) | 456 (0.11) |
| 1,000–1,499 g | 1,644 (0.39) | 1,533 (0.36) |
| 1,500–2,499 g | 18,671 (4.38) | 18,495 (4.40) |
| 2,500–4,000 g | 388,902 (91.26) | 384,179 (91.44) |
| >4,000 g | 16,551 (3.88) | 15,465 (3.68) |
| Prematurityb) | 23,404 (5.5) | 23,368 (5.6) |
| Death, total | 1,424 (0.3) | 1,294 (0.28) |
| Birth–3 months | 441 (0.09) | 432 (0.09) |
| 4–9 Months | 286 (0.06) | 258 (0.05) |
| 10–21 Months | 179 (0.04) | 162 (0.03) |
| 22–33 Months | 95 (0.02) | 106 (0.02) |
| 34–45 Months | 84 (0.02) | 74 (0.02) |
| 46–57 Months | 63 (0.01) | 64 (0.01) |
| 58–69 Month | 60 (0.01) | 38 (0.01) |
| >70 Months | 216 (0.05) | 160 (0.03) |
| Birth placec) | ||
| Seoul | 147,843 (31.51) | 90,496 (19.29) |
| Metropolis | 96,887 (20.65) | 106,079 (22.61) |
| Urban area | 167,357 (35.66) | 187,027 (39.86) |
| Rural area | 52,107 (11.10) | 59,965 (12.78) |
| Economic statusd) | ||
| 1st quintile (lowest income) | 38,222 (8.4) | 35,554 (8.3) |
| 2nd quintile | 69,678 (15.3) | 61.812 (14.4) |
| 3rd quintile (middle income) | 120,839 (26.6) | 112,885 (26.3) |
| 4th quintile | 144,949 (31.9) | 138,720 (32.3) |
| 5th quintile (highest income) | 80,827 (17.8) | 81,052 (18.9) |
a) Birth weight data were obtained from parental responses in the National Health Screening Program for Infants and Children (NHSPIC) database. Missing data: 43,000 (2008) and 28,331 (2009).
b) Prematurity status was from parental responses to the general questionnaire of the NHSPIC and defined as birth prior to 36-week gestation. Missing data: 43,444 (2008) and 29,406 (2009).
Table 4.
| Session No. (age) | Birth in 2008 (n=469,248) | Birth in 2009 (n=448,459) | Total |
|---|---|---|---|
| 1 (4–6 months) | 229,389 (48.88) | 238,491 (53.18) | 467,880 |
| 2 (9–12 months) | 204,845 (43.65) | 224,789 (50.12) | 429,634 |
| 3 (18–24 months) | 239,872 (51.12) | 262,218 (58.47) | 502,090 |
| 4 (30–36 months) | 256,085 (54.57) | 278,571 (62.12) | 534,656 |
| 5 (42–48 months) | 240,873 (51.33) | 280,319 (62.51) | 521,191 |
| 6 (54–60 months) | 239,197 (50.97) | 267,304 (59.61) | 506,501 |
| 7 (66–71 months) | 230,400 (49.1) | 233,139 (51.99) | 463,539 |
| All sessionsa) | 40,360 (8.6) | 55,686 (12.42) | 96,046 |
Table 5.
Table 6.
| Session No. (age) | Participating children (n) | Appropriate development, n (%) | Need for follow-up, n (%) | Recommendation for further evaluation, n (%) | Need for consistent management, n (%) |
|---|---|---|---|---|---|
| 2 (9–12 months) | 428,798 | 407,804 (95.1) | 17,520 (4.1) | 3,474 (0.8) | - |
| 3 (18–24 months) | 501,881 | 482,346 (96.1) | 15,230 (3.0) | 4,303 (0.9) | 2 (0.0) |
| 4 (30–36 months) | 534,478 | 513,870 (96.1) | 13,706 (2.6) | 6,293 (1.2) | 609 (0.1) |
| 5 (42–48 months) | 521,053 | 505,563 (97.0) | 9,238 (1.8) | 4,639 (0.9) | 1,613 (0.3) |
| 6 (54–60 months)a) | 506,427 | 495,245 (97.8) | 6,140 (1.2) | 3,310 (0.7) | 1,775 (0.4) |
| 7 (66–71 months)a) | 436,538 | 443,365 (95.7)a) | 15,082 (3.3) | 3,643 (0.8) | 1,448 (0.3) |
The developmental screening sessions 2, 3, 4, and 5 used the Korean Age and Stages Questionnaire (K-ASQ) in all participating children. Missing data: 836 (session 2), 209 (session 3), 178 (session 4), 138 (session 5), 31 (session 6), and 1 (session 7).
a) During session 6, 502,975 children were screened using the K-ASQ and 3,452 children using the Korean Developmental Screening Test for Infants and Children (K-DST). During session 7, 277,479 children were screened using the K-ASQ and 186,059 children using the K-DST. For K-DST, results of “advanced development” and “age appropriate” were defined as “appropriate.”





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


