Article Contents
| Clin Exp Pediatr > Volume 65(4); 2022 |
|
Abstract
Background
According to the National Family Health Survey–4, in India, 78.9% of deliveries occur in institutions, although only 42.6% of new mothers initiate breastfeeding within 1 hour of delivery.
Purpose
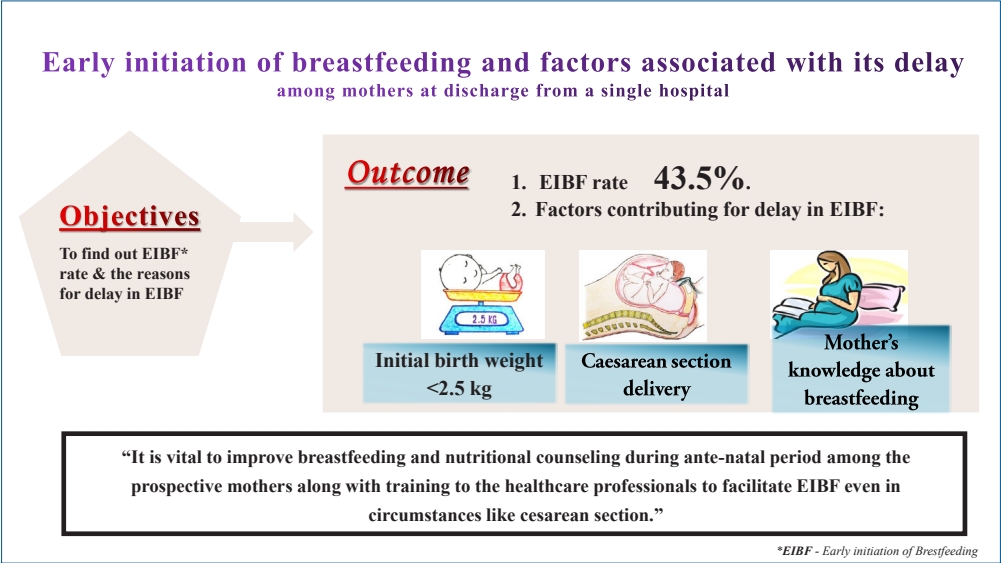
To estimate the proportion of early initiation of breastfeeding (EIBF) among new mothers at discharge from a tertiary care hospital and identify the determinants of delayed initiation of breastfeeding among them.
Methods
This was a hospital-based analytical cross-sectional study of 108 new mothers. After obtaining Institutional Review Board approval and informed consent, we interviewed the new mothers on the day of discharge. Multivariate logistic regression was performed using IBM SPSS Statistics ver. 24.
Results
The median breastfeeding initiation time was 90 minutes (interquartile range, 30–180 minutes). Overall, 43.5% of the mothers practiced EIBF, 77.4% practiced exclusive breastfeeding, and 43.5% were rooming in at discharge. Reasons for breastfeeding delays included extended recovery time from spinal anesthesia, maternal lassitude, and uncomfortable breastfeeding position due to post-cesarean pain. In the multivariate analysis, a birth weight less than 2,500 g (adjusted odds ratio [aOR], 4.33; 95% confidence interval [CI], 1.12–16.82; P=0.03), cesarean section delivery (aOR, 4.68; 95% CI, 1.57–13.92; P=0.005), and mother’s poor knowledge of breastfeeding (aOR, 4.61; 95% CI, 1.44–14.72; P=0.010) were more likely to delay the initiation of breastfeeding.
Conclusion
EIBF was practiced by less than half of the new mothers as determined by the cesarean section, baby’s birth weight, and mothers’ awareness of breastfeeding. Thus, it is vital to improve breastfeeding and nutritional counseling among mothers during the antenatal period and improve healthcare professionals’ training to facilitate EIBF, even in circumstances such as cesarean section.
Graphical abstract
Early initiation of breastfeeding (EIBF) is defined as ‘provision of mothers’ breast milk to infants within the first hour of birth and ensures that the newborn receives colostrum[1]. EIBF is crucial as it ensures that the baby receives a colostrum, a yellow liquid contains crucial nutrients and antibodies to newborn acts as a first feed and first immunization [1]. EIBF provides a unique opportunity for the infants to obtain balanced nutrition and energy required for their growth and development at the earliest. Similarly, it creates the bonding between the infant and the mother, which enhances the cognitive development. It also reduces the risk of developing noncommunicable disease and obesity in prime of life [1,2].
Not only that, EIBF also protects the infants during their critical window period from diseases like diarrhea, neonatal sepsis, and pneumonia and at the same time improves maternal-infant bonding [2-4]. It is evident from the previous studies that EIBF not only plays a crucial role in reducing neonatal mortality and also increases the chances of continuing exclusive breastfeeding at later months [3,4].
It is expected that delivery conducted in a health institution escalates the chances that a newborn will be initiated on early breastfeeding [2,5,6]. But unexpectedly, though 7.9% of the babies were institutionally delivered in India, only 42.6% of them were breastfed within one hour of birth [7]. Subsequently, various maternal and facility-level factors have proven to have impact on EIBF [6,8]. Our hospital is planning to move towards the baby-friendly hospital initiative (BFHI) policy, in which one of the key components is “to facilitate immediate and uninterrupted skin-to-skin contact and support mothers to initiate breastfeeding as soon as possible after birth.” [9] Identifying these factors and intervening at an early stage will help to accentuate EIBF at the facility level [5]. Hence, the current study was planned with the following objectives: (1) to estimate the proportion of EIBF among postnatal mothers at the point of discharge in a tertiary care hospital in Puducherry and (2) to find out the determinants of delayed initiation of breastfeeding among postnatal mothers.
The study was conducted in the postnatal ward by the Department of Community Medicine in collaboration with the Paediatrics Department in a tertiary care teaching hospital in Puducherry, India. This tertiary care institute is equipped with state-of-the-art equipment conducive to proficient stalwarts in conducting normal vaginal delivery and cesarean sections, followed by unmitigated postnatal care for both the mother and the newborn. The annual breastfeeding week celebration is organized by both departments, which has a beneficial response in elevating the breastfeeding habits in this hospital. It was a hospital-based analytical cross-sectional study. Data collection was done for 3 months. All postnatal mothers who delivered in the hospital (vaginal & cesarean delivery) during the study period were included in the study. Considering the prevalence of EIBF to be 14% [10] with 6.5% absolute precision and 10% nonresponse rate, the sample size was 108 (calculated using OpenEpi software ver. 3.01; Open Source Epidemiologic Statistics for Public Health). Consecutive sampling technique was used to include all the postnatal mothers for the study until the desired sample size was achieved.
After obtaining informed consent, data were collected using a pretested structured questionnaire. The questionnaire included demographic details, baby details, obstetric history, breastfeeding history, infant feeding practices, and rooming-in. Besides, open-ended questions were used to find out the reasons for delayed initiation of breastfeeding and rooming-in. A trained Community Medicine postgraduate paid visit to the postnatal mothers in the ward and conducted a face-to-face interview on the day before discharge. Confidentiality, anonymity, and privacy of the participants were guaranteed throughout the study.
The collected data were entered in Epi_Info (ver. 7.2.2.6; Centers for Disease Control and Prevention, Atlanta, GA, USA, and World Health Organization) software and analysed using IBM SPSS Statistics ver. 24.0 (IBM Co., Armonk, NY, USA). Bivariate and multivariate analyses were done to find out the determinants of delay in EIBF. In the first stage, an association between the delayed initiation of breastfeeding (dependent variable) and 15 independent variables such as baby age, baby’s sex, birth weight of the baby, mother’s age, area of the respondent, mother’s occupation, mother’s education, family type, socioeconomic status, religion, birth order, delivery type, prelacteal feeds, rooming-in and breastfeeding knowledge in mothers were done using bivariate analysis. In the next stage, 11 variables, (4 variables with higher odds ratio and 7 significant variables) obtained from bivariate analysis were included for multivariate logistic regression. The level of significance was set at 5% (P<0.05). The multiple coefficient of determinance (R2) was used as a goodness-of-fit statistic for the model.
Ethical clearance was obtained from the Institutional Ethics Committee (IEC) of Sri Mankula Vinayagar Medical College and Hospital, Puducherry (IEC Code no: 37/2019).
To ensure the present hospital-based cross-sectional study’s systemic reporting, STROBE (Strengthening The Reporting of an OBservational study in Epidemiology) guideline was followed [11].
The sociodemographic details of the baby and the mothers were given in Table 1. The mean±standard deviation age of the postnatal mothers was 26.16±4.22 years.
The median breastfeeding initiation time was 90 minutes (interquartile range [IQR], 30–180 minutes) among the participants. Out of 108 respondents, about 47 mothers (43.5%) initiated breastfeeding within one hour of the delivery (vaginal and cesarean delivery). Nearly 107 of infants (99.1%) were breastfed. Of the infants, 84 (77.4%) were exclusively breast milk-fed (breast milk+expressed breast milk), and more than half 73 (67.6%) were exclusively breastfed by natural mothers from the day of birth until discharge. Only 1 of infants (0.9%) received bottled feed as the mother was on antiarrhythmia drug. Of 108 mother-baby pairs, only 47 (43.5%) practiced rooming-in, and the reasons stated for low rooming-in practice were cesarean section and the requirement of neonatal intensive care unit (NICU) admission for babies for their medical illness.
Among 61 mothers who delayed initiation of breastfeeding, majority of them 95 (88.0%) stated that inadequate breast milk was the reasons for the delay. Other reasons stated by the mothers include that, about 86 mothers (79.6%) were exhausted after delivery, 37 participants (34.3%) said extended recovery time from anesthesia (late wearing of anaesthetic effect), 15 mothers (13.8%) explained the uncomfortable breastfeeding position after cesarean section and 10 mothers (9.3%) stated that delayed in episiotomy suture. Added to that, 85 of mothers (78.7%) quoted that their baby was in NICU observation after delivery and 61 mothers (56.5%) said there was an increased time for the transfer of baby form NICU after observation to ward or transfer of mother from operational theater to ward delayed the breastfeeding initiation (Fig. 1).
In multivariate analysis, 3 variables emerged as significant predictors for the delay in EIBF. Mothers who had babies with a birth weight of less than 2,500 g had 4.33 times higher odds (95% confidence interval [CI], 1.12–16.82; P=0.034) in delayed initiation of breastfeeding when compared to babies with birth weight more than or equal to 2,500 g. Mothers who had a cesarean section (95% CI, 1.57–13.92; P=0.005) had 4.68 times higher odds of not initiating breastfeeding earlier than mothers who had a vaginal delivery. Similarly, the odds of delay in EIBF among mothers who had poor knowledge about breastfeeding was 4.61 times (95% CI, 1.44–14.72; P=0.010) higher when compared to the mothers with breastfeeding knowledge. The Nagelkerke pseudo-R2 value for the final model was 36.7 percentages (Table 2). The EIBF rates and associated factors from other studies were summarized in Table 3.
The present study showed that, out of 108 postnatal mothers, 47 (43.5%) initiated breastfeeding within 1 hour after delivery. The median breastfeeding initiation time was about 90 minutes (IQR, 30–180 minutes). Approximately 73 infants (67.6%) were breastfed exclusively by their mothers, but the rooming-in rate was 47 (43.5%) only. Babies with birth weight less than 2,500 g; mothers who had cesarean section delivery and reduced awareness and knowledge about breastfeeding were found to be significant factors for delayed initiation of breastfeeding.
In the present study, EIBF rate was found to be 43.5%, despite the breastfeeding rate of 99.1%, which was similar to the EIBF rate at the national level (42.6%); however, it was found to be lower than the Puducherry state-level report (64.6%) [7,12]. Besides, the prevalence of EIBF observed in our study was lower than that observed in studies done in other states such as Maharashtra (45.2%), Andhra Pradesh (75.6%), and Tamil Nadu (97.5%) but higher than Madhya Pradesh (38.6%), Nagpur and Odisha (36.4%), and Bihar (24.86 percentage) [13-19]. This deviations of the rate within nation might be owing to study setting, sampling procedures in other studies, and possible effects from cultural factors. Similar cross-sectional studies done outside India, in Africa, Central America, Nepal, and Bangladesh showed higher prevalence of EIBF ranging from 47.3% to 80% while results from Uganda, Nigeria, and Northwest Romania showed lower EIBF rate (range, 19.7%–34.7%) than our study findings [2,6,20-27]. (Table 3). The wide variation in EIBF rates may be due to disparities in social, cultural, and ethnographic factors, in breastfeeding practice.
Mothers who had delivered their baby by cesarean section were found to be associated with delay in initiation of breastfeeding (aOR, 4.68; 95% CI, 1.57–14.72; P=0.005) as compared to those who had a vaginal delivery. This association has also been observed with the studies from India and other countries globally [2,6,13,15,18,20-23,26-28]. Maternal factors, such as maternal lassitude, inconvenient breastfeeding position due to post-cesarean pain, and insufficient breastmilk (due to reduced oxytocin release followed by anesthesia) [29] might have hampered the immediate direct skin-to-skin contact, was observed in this study also contributed for the delay [2,6,8,13,18,20-23,27,30]. This can be overcome by providing physical and psychological support to these mothers by their family members and healthcare providers immediately after ceserean section might improve the EIBF.
Institutional factors for EIBF among ceserean section mothers such as extended recovery time from spinal anesthesia and reduced rooming-in rate which were also found in our study might have contributed to this delay [2,6,8,13,18,20-23,27,30]. This reduced practice of EIBF in postoperative room immediately after C-section by healthcare professionals who assist in mother’s recovery rather than initiating breastfeeding might lend to this factor [23]. This can be overcome by initiating maternal-infant skin-to-skin contact at the earliest through practices like breast-crawl that proven to have a major impact on EIBF even in cesarean deliveries [31,32]. Thus, healthcare providers and nursing staff need to be sensitized about these bottlenecks in initiating EIBF and need to be trained about the different breastfeeding positions, and practice of breast-crawl in cesarean sections. This also requires, appropriate guidelines and policy regarding the cesarean delivery at the healthcare center to improve the EIBF.
Baby’s birth weight of less than 2,500 g was a significant factor for delayed breastfeeding initiation (aOR, 4.33; 95% CI, 1.12–16.82; P=0.034) found in the study. Our findings were similar to the studies done in inside and outside India [2,13,15,20]. The possible explanation of the delay in EIBF could be due to poor suckling capacity, swallowing difficulty and poor co-ordination of a premature baby and requirement of admission in a NICU due to medical conditions like respiratory distress, jaundice, meconium aspirations, and again low birth weight [5,6,13,20] were also asserted in our study. These barriers can be addressed by providing early skin-to-skin contact and initiating breastfeeding immediately after delivery to improve their suckling reflex and giving expressed breast milk to the babies admitted in NICU to improve their nutrition and well-being. This explicates the want of practice and training to healthcare providers in handling low birth weight babies and counseling to the prospective mothers during the antenatal care (ANC) clinic to achieve the early initiation and continuation of breast milk feeding in low birth weight babies.
The current study showed that mothers who had poor knowledge about breastfeeding had 4.61 times higher odds to delay initiation of breastfeeding than mothers with knowledge about breastfeeding (95% CI, 1.44–14.72; P=0.010). This was consistent with the findings of the studies done previously [13,26,28]. ANC visit or appointments acts as a bridgehead of the mothers to have contact with the healthcare professionals [33]. Multiple researches have revealed that approaches like health promotion and breastfeeding counseling during the ANC visit can enhance the rate of timely initiation of breastfeeding [5,9,22,24,27,34,35]. Thus, scaling up of intervention programs among antenatal mothers at the institutional level helps the mothers to be more receptive and provide them good opportunity to acquire knowledge about it to prepare them for timely initiation of breastfeeding [5,34]. In addition to that, healthcare professionals need to be trained on skills requires for efficient initiation of breastfeeding for its promotion and support along with nutritional education. Furthermore, this explains the paramount importance of implementing the baby-friendly initiatives at the institution level.
The major strengths of the study are the use of pretested structured questionnaire and data collection by a single investigator throughout the study. Collection of data at the point of discharge helps to minimize the maternal recall bias. However, being a cross-sectional study, temporality of association could not be assessed. Also, this was a hospital-based single centric study, in which the results cannot be extrapolated to the general population.
EIBF was practiced by less than half of the postnatal mothers, determined by birth by cesarean section, the baby’s birth weight and mothers’ awareness about breastfeeding. We recommend that additional support, training, and education need to be provided to the healthcare practitioners to increase breastfeeding initiation to the mothers predominantly who had cesarean sections to enable early skin-to-skin contact. Overall, this study also implies that comprehensive breastfeeding education programs and counseling targeting antenatal mothers need to be scaled up at the institution level. Added to these, there is an imperative need to focus on full implementation of the BFHI and infant young child feeding policies at the institutional level to intensify the EIBF and child’s well-being.
Acknowledgments
We thank all the staff, physicians, medical interns, and nurses in the Department of Paediatrics and Obstetrics for their generous assistance and support; we were also very thankful to all the postnatal mothers who participated in this study. I also extend my gratitude to the judges of poster presentation of AIIMS conference 2020, Mangalagiri, for their comments in improving the draft.
Fig. 1.
Reasons for delay of early initiation of breastfeeding (n=61). Values are presented with percentages (%). OT, operating theater; NICU, neonatal intensive care unit.
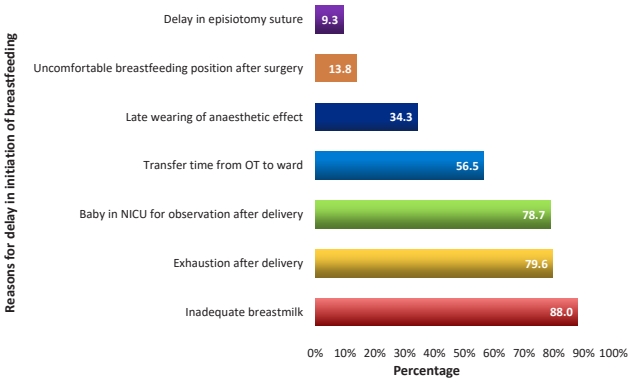
Table 1.
Sociodemographic details of postnatal mothers and infants before discharge (n=108)
Table 2.
Bivariate and multivariate analyses of determinants of delayed initiation of breastfeeding among postnatal mothers at discharge (n=108)
| Variable | No. (%) | Delay in EIBF, n (%) |
OR (95% CI) |
|
|---|---|---|---|---|
| Unadjusted | Adjusted | |||
| Sex of the baby | ||||
| Male | 59 (54.6) | 34 (57.6) | 1.10 (0.51–2.37) | |
| Female | 49 (45.4) | 27 (55.1) | 1 | |
| Birth weight of the baby (g) | ||||
| <2,500 | 21 (19.5) | 16 (76.2) | 2.98 (1.00–8.87) | 4.33 (1.12–16.82) |
| ≥2,500 | 87 (80.5) | 45 (51.7) | 1 | 1 |
| Age of the mother (yr) | ||||
| 10–19 | 6 (5.6) | 2 (33.3) | 5.25 (0.56–48.95) | |
| 20–29 | 79 (73.1) | 21 (26.6) | 3.80 (0.82–17.62) | |
| ≥30 | 23 (21.3) | 2 (8.7) | 1 | |
| Area of the respondent | ||||
| Urban | 55 (50.9) | 10 (18.2) | 1.77 (0.71–4.40) | |
| Rural | 53 (49.1) | 15 (28.3) | 1 | |
| Mothers’ occupation | ||||
| Housewife | 101 (93.5) | 22 (21.8) | 1 | |
| Working mothers | 7 (6.5) | 3 (42.9) | 2.69 (0.56–12.94) | |
| Mother’s education | ||||
| Primary | 11 (10.2) | 6 (54.5) | 0.61 (0.16–2.26) | |
| Secondary | 38 (35.2) | 16 (42.1) | 0.37 (0.16–0.86) | |
| Graduate & professional | 59 (54.6) | 39 (66.1) | 1 | |
| Socioeconomic status of the family (BG Prasad scale 2019) | ||||
| Upper class | 16 (14.8) | 10 (62.5) | 5 (0.95–26.1) | |
| Middle classa) | 80 (74.1) | 47 (58.8) | 4.27 (1.07–16.99) | |
| Lower class | 12 (11.1) | 3 (25.0) | 1 | |
| Order of birth | ||||
| First child | 48 (44.4) | 31 (64.6) | 1 | |
| Second child | 47(43.5) | 26 (55.3) | 0.67 (0.29–1.54) | |
| Three or more children | 13 (12.1) | 4 (30.8) | 0.24 (0.06–0.91) | |
| Type of delivery | ||||
| Cesarean section | 77 (71.3) | 50 (64.9) | 3.36 (1.40–8.05) | 4.68 (1.57–13.92) |
| Vaginal delivery | 31 (28.7) | 11 (35.5) | 1 | 1 |
| Prelacteal feeding | ||||
| Yes | 24 (22.2) | 18 (75.0) | 3 (1.08–8.30) | |
| No | 84 (77.8) | 42 (50.0) | 1 | |
| Knowledge about breastfeeding | ||||
| Yes | 77 (71.3) | 37 (48.1) | 1 | 1 |
| No | 31 (28.7) | 24 (77.4) | 3.70 (1.42–9.61) | 4.61 (1.44–14.72) |
Table 3.
Summary of rate of early initiation of breastfeeding and factors associated with its delay
| Regions and year | Author | Type of study | EIBF | Factors associated with delayed initiation of breastfeeding | |
|---|---|---|---|---|---|
| Studies with increased EIBF rate than our study prevalence of 43.5% | |||||
| International | |||||
| Ethiopia; 2016 | Tewabe [22] | Cross-sectional study | 78.8% | Delivery at home, cesarean section, given prelacteal feeds | |
| Guatemala; 2017 | Atyeo et al. [24] | Mixed method study | 76% | Source of breastfeeding information from mother or relative, complementary food introduction, living area | |
| Bahir Dar City, Ethiopia; 2019 | Belachew [23] | Cross-sectional study | 75.4% | Delivery at home, cesarean section, no breastfeeding counseling during ANC visits | |
| Bangladesh; 2019 | Karim et al. [6] | Secondary data analysis | 51% | Cesarean section, mother who have not received PNC visit with babies | |
| Northern Uganda; 2017 | Mukunya et al. [21] | National survey | 48.2% | Cesarean delivery, discarding initial breast milk, delivery at home, education status of mother | |
| Kathmandu; 2019 | Acharya et al. [20] | Cross-sectional study | 47.3% | Cesarean delivery, low birth weight babies | |
| Saudi Arabia; 2019 | Ahmed and Salih [28] | Cross-sectional study | 43.6% | Cesarean section, reduced knowledge about breast- feeding, mother’s educational status, do not know how to initiate breastfeeding | |
| National | |||||
| Tamil Nadu; 2012 | Jennifer and Muthukumar [19] | Cross-sectional study | 97.5% | - | |
| Andhra Pradesh, 2019 | Uppiretla et al. [16] | Cross-sectional study | 75.6% | - | |
| Maharashtra, 2020 | Jeyakumar et al. [15] | Cross-sectional study | 45.2% | Delivery at home, cesarean section, very low birth weight | |
| Studies with reduced EIBF rate than our study prevalence of 43.5% | |||||
| International | |||||
| Nigeria; 2016 | Berde and Yalcin [2] | Cross - sectional study | 34.7% | Delivery at home, cesarean section, first birth order, size of the baby at birth, mother’s occupation, wealth index, residency type | |
| Uganda; 2015 | Kalisa et al. [27] | Cross-sectional study | 31.4% | Maternal HIV positive status, inadequate prenatal guidance, inadequate professional assistance to initiate breastfeeding, cesarean section, other reasons were perceived lack of breast milk, need of rest for both mother and baby after labor, and negative cultural beliefs. | |
| Northwestern Romania; 2019 | Cozma-Petruţ et al. [26] | Cross-sectional study | 24.30% | Public hospital delivery, Cesarean delivery, no mother–newborn skin-to-skin contact for one hour or more, no counseling during ANC visit | |
| National | |||||
| Madhya Pradesh; 2015 | Sharma et al. [14] | Cross-sectional study | 38.60% | Mother’s education and occupation, reduced counseling of mother during ANC visits, home delivery, delivery conducted by untrained person, no postnatal advice received | |
| Nagpur; 2013 | Patel et al. [13] | Cross-sectional study | 36.4% | Education status of the mother, no counseling during ANC clinic visit, cesarean section, mothers with obstetric problems, gestational week | |
| Odisha; 2021 | Kuchi et al. [18] | Observational study | 36.4% | Cesarean sections, rooming-in, multiparous homema- kers, nuclear families | |
| Puducherry; 2018 | Babu et al. [30] | Mixed method study | 1.39% | Time of rooming-in, mother’s knowledge on importance of EIBF | |
| Haryana; 2016 | Majra and Silan [8] | Qualitative study - FGD | - | Lack of awareness regarding proper technique of breastfeeding and benefits of colostrum, breast abnormality like inverted/retracted nipples, obstetric/neonatal complications requiring specialized care, cultural practices like giving prelacteal, gender discrimination | |
References
1. World Health Organization (WHO). Breastfeeding [Internet]. Geneva (Switzerland), WHO. [cited 2019 Feb 26]; Available from: https://www.who.int/health-topics/breastfeeding#tab=tab_2.
2. Berde AS, Yalcin SS. Determinants of early initiation of breastfeeding in Nigeria: a population-based study using the 2013 demographic and health survey data. BMC Pregnancy Childbirth 2016;16:32.


4. Debes AK, Kohli A, Walker N, Edmond K, Mullany LC. Time of initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health 2013;13:S19.


5. Forster DA, McLachlan HL. Breastfeeding initiation and birth setting practices: a review of the literature. J Midwifery Womens Health 2007;52:273–80.


6. Karim F, Billah SM, Chowdhury MAK, Zaka N, Manu A, Arifeen SE, et al. Initiation of breastfeeding within one hour of birth and its determinants among normal vaginal deliveries at primary and secondary health facilities in Bangladesh: a case-observation study. PLoS One 2018;13:e0202508.



7. United Nations Children’s Fund (UNICEF). India (IND)–Demographics, Health and Infant Mortality–UNICEF DATA [Internet]. New York: UNICEF; 2019 [cited 2020 Mar 23]. Available from: https://data.unicef.org/country/ind/.
8. Majra JP, Silan VK. Barriers to early initiation and continuation of breastfeeding in a tertiary care institute of Haryana: a qualitative study in nursing care providers. J Clin Diagn Res 2016;10:LC16–20.



9. World Health Organization (WHO) & United Nations Children's Fund (UNICEF). Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services–the revised Baby-Friendly Hospital Initiative. Geneva (Switzerland): WHO, 2018.
10. Takahashi K, Ganchimeg T, Ota E, Vogel JP, Souza JP, Laopaiboon M, et al. Prevalence of early initation of breastfeeding and determinants of delayed initiation of breastfeeding: secondary analysis of the WHO global survey. Sci Rep 2017;7:44868.


11. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. statement: guidelines for reporting observational studies. Ann Intern Med 2007;147:573–7.


12. Senanayake P, O’Connor E, Ogbo FA. National and rural-urban prevalence and determinants of early initiation of breastfeeding in India. BMC Public Health 2019;19:896.



13. Patel A, Banerjee A, Kaletwad A. Factors associated with prelacteal feeding and timely initiation of breastfeeding in hospital-delivered infants in India. J Hum Lact 2013;29:572–8.


14. Sharma A, Thakur PS, Tiwari R, Kasar PK, Sharma R, Kabirpanthi V. Factors associated with early initiation of breastfeeding among mothers of tribal area of Madhya Pradesh, India: a community based cross sectional study. Int J Community Med Public Health 2016;3:194–9.

15. Jeyakumar A, Jungari S, Nair R, Menon P, Babar P, Bhushan B, et al. Prevalence and determinants of early initiation (EI), exclusive breastfeeding (EBF), and prelacteal feeding among children aged 0-24 months in slums of Pune city, in Maharashtra. Ecol Food Nutr 2021;60:377–93.


16. Uppiretla SB, Mishra SK, Rachakulla HK. Infant feeding practices among mothers in rural Rajamahendravaram, Andhra Pradesh. I J Community Med Public Health 2019;6:2121–6.

17. Randhawa A, Chaudhary N, Gill BS, Singh A, Garg V, Balgir RS. A population-based cross-sectional study to determine the practices of breastfeeding among the lactating mothers of Patiala city. J Family Med Prim Care 2019;8:3207–13.



18. Kuchi S, Sahu S, John J. Too little and too late. Initiation of breastfeeding in Odisha, India: an observational study. J Family Med Prim Care 2021;10:1592–5.



19. Jennifer HG, Muthukumar K. A cross-sectional descriptive study to estimate the prevalence of early initiation and exclusive breast feeding in the rural health training centre of a medical college in Tamilnadu, Southern India. J Clin Diagnostic Res 2012;6:1514–7.
20. Acharya S, Khanal C, Dahal AS, Maharjan M. The determinants of early initiation of breastfeeding practice among mothers attending a tertiary hospital, Kathmandu. J Nepal Paediatr Soc 2019;39:168–73.

21. Mukunya D, Tumwine JK, Nankabirwa V, Ndeezi G, Odongo I, Tumuhamye J, et al. Factors associated with delayed initiation of breastfeeding: a survey in Northern Uganda. Glob Health Action 2017;10:1410975.



22. Tewabe T. Timely initiation of breastfeeding and associated factors among mothers in Motta town, East Gojjam Zone, Amhara regional state, Ethiopia, 2015: a cross-sectional study. BMC Pregnancy Childbirth 2016;16:314.



23. Belachew A. Timely initiation of breastfeeding and associated factors among mothers of infants age 0-6 months old in Bahir Dar City, Northwest, Ethiopia, 2017: a community based cross-sectional study. Int Breastfeed J 2019;14:5.




24. Atyeo NN, Frank TD, Vail EF, Sperduto WAL, Boyd DL. Early initiation of breastfeeding among maya mothers in the Western Highlands of Guatemala: practices and beliefs. J Hum Lact 2017;33:781–9.


25. Ali F, Mgongo M, Mamseri R, George JM, Mboya IB, Msuya SE. Prevalence of and factors associated with early initiation of breastfeeding among women with children aged < 24 months in Kilimanjaro region, northern Tanzania: a community-based cross-sectional study. Int Breastfeed J 2020;15:80.




26. Cozma-Petruţ A, Badiu-Tişa L, Stanciu O, Filip L, Banc R, Gavrilaş L, et al. Determinants of early initiation of breastfeeding among mothers of children aged less than 24 months in Northwestern Romania. Nutrients 2019;11:2988.



27. Kalisa R, Malande O, Nankunda J, Tumwine JK. Magnitude and factors associated with delayed initiation of breastfeeding among mothers who deliver in Mulago hospital, Uganda. Afr Health Sci 2015;15:1130–5.



28. Ahmed AE, Salih OA. Determinants of the early initiation of breastfeeding in the Kingdom of Saudi Arabia. Int Breastfeed J 2019;14:13.



29. Smith LJ, Kroeger M. Impact of birthing practices on breastfeeding. 2nd ed. Sudbury (MA): Jones & Barlett Learning, 2010;:102–3.
30. Babu RA, Keepanasseril A, Kanimozhi K. Practice of early initiation of breastfeeding among postnatal mothers in a tertiary hospital in south India. Int J Adv Med Health Res 2018;5:18–20.

31. Girish M, Mujawar N, Gotmare P, Paul N, Punia S, Pandey P. Impact and feasibility of breast crawl in a tertiary care hospital. J Perinatol 2013;33:288–91.


32. Thomas S, Mohanty N, Dasila PK. Effect of breast crawl on initiation of breastfeeding and initial weight loss among new-borns. Manipal J Nurs Health Sci 2018;4:1–5.
33. World Health Organization (WHO). Opportunities for Africa’s Newborns Practical data, policy and programmatic support for newborn care in Africa [Internet]. Geneva (Switzerland): WHO; 2006 [cited 2021 Mar 28]; Available from: https://www.who.int/pmnch/media/publications/oanfullreport.pdf.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


