Our understanding of developmental dysplasia of the hip (DDH) in newborns, especially premature infants, remains imperfect. The incidence of DDH is 0.1%–2% in newborns [1]. If immature or unstable hips are included, the incidence reaches 15%. This is because DDH ranges from very mild subluxation to dislocation. In addition to the wide disease spectrum, its pathogenesis is multifactorial, making discovery of its risk factors very difficult, such as a family history of DDH, female sex, coexistence of skeletal diseases, breech presentation, first birth, oligohydramnios, left hip joint, and tight swaddling [2]. Moreover, there have been various recommendations for hip joint surveillance timing such as 3–4 weeks, 4–6 weeks, older than 4–6 weeks, and 6 weeks to 8 months [3]. This controversy leads to difficulty in establishing standardized screening guidelines for term and preterm infants.
Agreement is also lacking about the best screening technique or critical clinical findings to eliminate the risk of DDH. However, there is consensus that prognosis is very poor when DDH or unstable hip is left untreated until 2–3 years of age, implying the importance of early detection better prognosis. Early-stage DDH can be simply treated with a Palvik harness with minimal complications. Ultrasonography is the gold standard with high sensitivity and specificity for the diagnosis of infantile DDH. Using ultrasonography, the identification of DDH in the general population has reportedly improved from 1.6–28.5 per 1,000 infants to 34.0–60.3 per 1,000 infants [4].
Several countries have evaluated DDH using routine infantile screening programs. For example, ultrasonography is universally performed for DDH screenings in Austria and Germany, whereas it is selectively performed for infants with risk factors and abnormalities on physical examinations in the US, UK, and Canada, which focus on detecting DDH before 3 months of age.
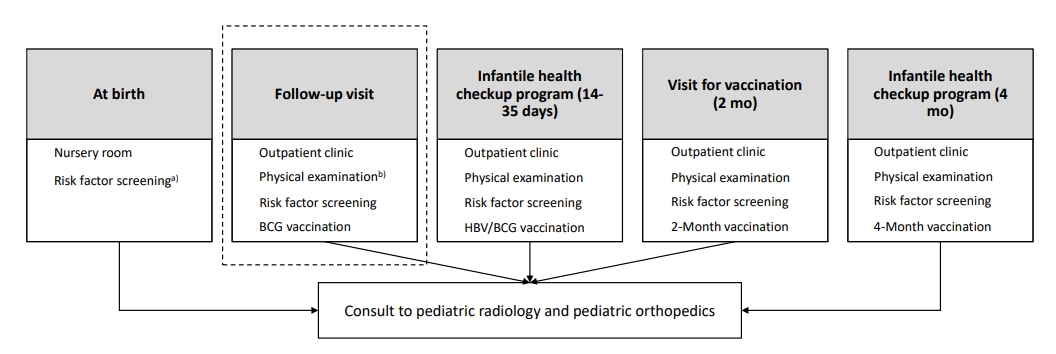
In Korea, as part of an infant health checkup program, infants with risk factors have been screened at 4 months of age since 2007. Fortunately, an additional routine examination at 1 month (14–35 days) has been included in the program since 2021, and it described screening for three major risk factors (breech position in the third trimester, oligohydramnios, and family history). However, no information on the detailed physical examination and further plans for each risk factor has not been included. A possible DDH screening flow chart is presented in Fig. 1.
Especially for infants older than 3 months, the most sensitive examination is that of asymmetric diminished hip abduction [5,6]. Moreover, the presence of uneven buttock creases has low sensitivity and specificity for the detection of DDH. Even the representative physical examinations, the Barlow and Ortolani maneuvers, alone showed a low sensitivity of 54% [7]. Risk factor screening and physical examination are required to improve detection rates. The physical examination identifies uneven limb length and buttock creases, restricted abduction, and abnormal Ortolani and Barlow maneuvers.
When the physical examination is suspicious or inconclusive, ultrasonography can be selectively used for infants 6 weeks to 6 months of age with risk factors [2]. Minor hip abnormalities on ultrasonography in those infants can be resolved without treatment. Radiology with anteroposterior and frog pelvic views can also be an option. Radiology and ultrasonography are effective, especially for infants 4–6 months of age [2]. The importance of a systematic screening program in Korea was described by Cha et al. [8], who reported that more than 95% of pediatric patients treated for DDH were screened at primary clinics and referred to tertiary hospitals in Korea.
The natural course and risk factors for DDH in premature infants remain controversial. Moreover, the mechanical force of a breech presentation, a well-known risk factor in term infants, remains unclear in premature infants. Interestingly, a small number of studies have reported oligohydramnios and female sex as possible risk factors for DDH in premature infants [9]. Multicentric studies are required to examine these subjects. Jeon et al. [3] evaluated the possible risk factors of DDH in premature infants and found that some did not correspond with previous reports. Considering the lack of studies of premature infants, they provided important information about the risk factors of DDH and surveillance time in this population. They subsequently recommended evaluating the hip joints of premature infants later than 38 weeks of gestational age despite other authors recommended evaluations after 44 weeks of gestational age [3,10].
The incidence of hip joint instability in premature infants seems significant, and most such lesions are normalized on follow-up evaluations, although the exact age or timing remains uncertain. These results imply that the hip joint development of premature infants has different physiology; thus, the application of the same screening protocols as term infants would be unsuitable because of the risks of under- or overtreatment.
The incidence of premature delivery is increasing in Korea. Moreover, DDH is very difficult to detect without a history and physical examination. Therefore, its early detection and treatment are crucial. Thus, it would be appropriate to consider the development of more delicate and detailed screening algorithms involving the role of ultrasonography and the development of separate strategies for premature infants. Training programs for clinicians regarding hip joint screening at 1 and 4 months are also required.
See the article “Risk factors and screening timing for developmental dysplasia of the hip in preterm infants” via https://doi.org/10.3345/cep.2021.01074.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


