In 2021, the Korean Society of Nephrology published clinical practice guidelines for the optimal hemodialysis (HD) treatment of patients with kidney failure [1]. Based on an extensive evidenceoriented review, the guidelines provided recommendations for the initiation, dose, modality, anticoagulation, control of volume and blood pressure, and monitoring to maintain HD. In chapter 8, the authors recommended that the nurse-to-patient ratio in pediatric HD be increased to 1:1–2. However, the guidelines did not include other aspects of pediatric HD that differ from those of adults. While the basic concept of HD is similar between adults and children, specific factors must be considered in the latter, including the small dialyzer and circuit, difficult vascular access, and frequent complications [2].
While most adults with kidney failure receive HD, peritoneal dialysis is preferred in children because it is difficult to maintain a vascular access route for HD, and children attend daytime activities, such as school. Pediatric nephrologists choose HD for pediatric patients with kidney failure in the following cases: (1) peritoneal dialysis is impossible due to abdominal conditions such as omphalocele or gastroschisis, bladder exstrophy, diaphragmatic hernia, peritoneal membrane failure, and previous abdominal surgery; (2) presence of diseases requiring HD, such as primary hyperoxaluria and inborn error of metabolism; (3) a short waiting period for a kidney transplant; and (4) lack of an appropriate caregiver [3].
Children on HD experience more common and severe HD-associated complications than adults, including catheter-related problems and hemodynamic instability [4]. Although clinical guidelines recommend arteriovenous fistulas as vascular access for HD in children, central vascular catheters are the most widely used modality for ensuring long-term vascular access in children [5-7]. Catheter-related bloodstream infections are the most common cause of catheter removal and replacement. The Kidney Disease Outcomes Quality Initiative practice guidelines recommend standardized catheter care protocols for hand hygiene, exit-site care, and accessing and disconnecting catheters to reduce catheter-related infections [8]. Central vascular catheters can lead to stenosis or obliteration of major intrathoracic vessels, especially in younger children. During HD, children often experience acute hemodynamic instability, which contributes to morbidity and mortality. Intradialytic hypotension is a common adverse event that induces ischemic insults to the myocardium and brain. It requires immediate treatment, including volume challenge, changes in patient position, lowering of ultrafiltration, or discontinuation of the dialysis session [3].
The correct assessment of dry weight in patients undergoing HD is important for reducing intradialytic hypotension; however, it is difficult in children, whose height and body weight are continuously increasing. Although objective methods including bioimpedance spectroscopy and relative blood volume monitoring have recently been introduced, there is little evidence to support their application in pediatric patients with HD. Children with chronic kidney disease (CKD) have a higher frequency of neurodevelopmental and cognitive dysfunction [9]. Psychosocial problems are also an important issue for pediatric patients with CKD [10]. Several factors contribute to these complications in children on HD, such as uremic toxins, ischemic brain injury caused by intradialytic hypotension, educational disruption due to frequent hospital visits, and traumatic medical experiences.
Although achieving and maintaining pediatric HD is challenging, steady efforts are needed to ensure its safety and reduce its complications, thereby improving clinical outcomes. First, as recommended by the KSN guidelines, the nurse-to-patient ratio should be maintained at 1:1 or 1:2, and an experienced pediatric dialysis nurse is needed to ensure patient safety [1,3,4]. To prevent intradialytic hypotension and hypothermia, pediatric dialysis nurses should frequently monitor patient volume status and vital signs.
Second, vascular access, dialyzer, and extracorporeal circuits must be considered in pediatric HD. A patent vascular access is the most important factor for adequate dialysis. Successful vascular access requires a skilled vascular surgeon and interventional radiologist. Since a child can usually tolerate a maximum of 10% of their blood volume in the extracorporeal circuit, the dialyzer and blood line are selected based on their age and size [2]. The surface area of the dialyzer used in children correlates to 75%–100% of their total body surface area [2,6]. Because of a child’s smaller blood volume, dialyzers with a large surface area can cause hypotension during HD treatment.
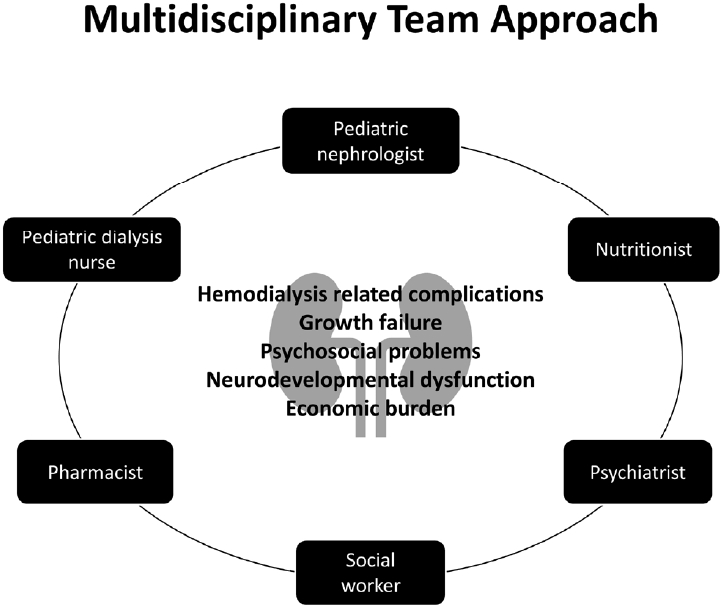
Third, to reduce complications caused by extracorporeal circulation and maintain the efficacy of dialysis, clinicians should limit the blood flow rate and dialysis time and increase the number of dialysis sessions in children, especially infants. Increasing evidence suggests that intensified HD with aggressive nutritional support is effective at improving the nutritional and growth status of children [3,6]. Schedules for intensified HD include extended dialysis time, more frequent short daytime sessions, and daily nocturnal HD. Finally, a skilled multidisciplinary team consisting of pharmacists, social workers, nutritionists, psychiatrists, pediatric nephrologists, and pediatric dialysis nurses is needed to manage dialysis treatment and complications and provide psychosocial support (Fig. 1) [4].





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


