Article Contents
| Clin Exp Pediatr > Volume 67(10); 2024 |
|
Abstract
Background
Mothers must acquire the knowledge and skills needed to fulfill their responsibilities and take care of themselves and their babies.
Purpose
This study aimed to examine the effects of online baby care education and postpartum counseling based on Meleis' transition theory on mothers' readiness for baby care and breastfeeding.
Method
This randomized controlled trial was conducted between May 2022 and May 2023 at the pregnancy follow-up outpatient clinic of a state hospital. The study sample consisted of 102 pregnant women (52 in the intervention group, 50 in the control group).
Results
The mean scores of the intervention group compared to the control group were significantly higher immediately after birth and at 1, 2, and 3 months postpartum. Change over time was significantly higher in repeated measurements of National Institute of Child Health and Human Development scale scores of the intervention and control groups (P=0.001). In the first 24 hours, mothers in the intervention group breastfed more successfully than those in the control group (P<0.001). Mothers in the intervention group exclusively breast fed at a significantly higher rate immediately and at 1, 2, and 3 months postpartum compared to the control group (P<0.001). A statistically significant difference was noted in mean infant height and weight in the intervention group compared to the control group (P<0.05).
Conclusion
Theory-based online education initiated during pregnancy and counseling continued up to 3 months postpartum positively affected the mothers' abilities to care for their infants. Mothers who received education and counseling breastfed their babies more successfully on the first day and breast fed exclusively at a higher rate in the first 3 months.
Graphical abstract.
Motherhood is a developmental transition process that begins with the realization of pregnancy and continues after birth [1]. The mother takes responsibility for the care of the baby with the birth of the baby [1,2]. Mothers are more inexperienced in baby care and breastfeeding, especially with their first baby [3]. Mothers need to acquire some knowledge and skills to fulfill their responsibilities and take care of themselves and their babies [1-6].
Personal experience, cultural level, family attitudes, risky situations in previous pregnancies, number of children, social support systems, knowledge of infant care, self-confidence, readiness for motherhood, etc. affect the perception of motherhood [3,7]. Readiness is the evaluation of one's own abilities and situation, considering the available options, determining new solutions and goals, trying, and realizing them. In cases where the mother is not ready to care for the baby; malnutrition, breastfeeding problems, risk of infectious diseases, growth and developmental retardation in the baby and mortality rates increase [7-10].
A woman's readiness and knowledge about motherhood are personal characteristics that facilitate the transition to motherhood. Expectations about motherhood, loss of control, breastfeeding and insomnia, lack of knowledge, inexperience, and unpreparedness are characteristics that prevent transition [11]. Preparation for the future plays a facilitating role in transition experiences [5]. In the literature, it is stated that Meleis's Transition Theory is the most accurate theory to prepare women for motherhood, to understand the factors facilitating the transition, and to ground care [5,11,12]. Shorey et al. [12] state that Meleis's Transition Theory is an applicable theory to identify the facilitating factors in the transition and adaptation of the mother to her new role and to support the mother. In Meleis theory, it is reported that vulnerability is high during transition periods such as pregnancy, motherhood, menopause, working life, migration, and care processes [5]. Understanding the changes that occur during transition periods and the factors affecting transition will support successful transition [11].
Midwives should train mothers on feeding the baby, establishing sleep routines, communicating with the baby, responding to their needs, and coping with diseases [13], ensuring their adaptation to the postpartum period, and providing postpartum counseling for babies to receive breast milk [14-17]. In the literature, it is stated that training for mothers plays an important role in improving child health [13,18-20]. Research on the effect of education given during pregnancy on preparation for motherhood and breastfeeding is limited [21].
The World Health Organization points out that the use of web and mobile health applications to support communication is an integral part of daily activities [22]. In a study, the effectiveness of home visits to mothers in the postpartum period and web-based nurse/midwife support was examined and it was determined that web-based support is a good alternative to home-based support programs [23]. This study aimed to examine the effects of online baby care education and postpartum counseling based on Meleis's Transition Theory on mothers' readiness for baby care and breastfeeding levels.
The study was conducted in a baby-friendly public hospital in Istanbul between May 2022 and May 2023. The aim of this randomized controlled trial was to investigate the effects of online infant care education and postpartum counseling based on Meleis' transition theory on (1) mothers' readiness for infant care,(2)infants' breastfeeding success, (3) duration of exclusive breastfeeding, and (4) infants’ growth rate in the first 3 months.
The hypotheses of the study were as follows:
H1: Mothers who received online infant care education based on Meleis' Transition Theory and postpartum counseling have higher Readiness for Hygienic Care of the Newborn Scale scores than the control group.
H2: Breastfeeding success of the infants of mothers who received online infant care training based on Meleis' transition theory and postpartum counseling is higher than the control group.
H3: Based on Meleis's Transition Theory, infants of mothers who receive online baby care training and postpartum counseling grow faster than those in the control group.
Before starting the study, approval was obtained from the Institutional Review Board (IRB) of Haliç University Non-Interventional Clinical Research Ethics Committee (IRB Protocol Number: 84; Date: 27.04.2022). The study was recorded in the Clinicaltrials.gov PRS system on (ID: NCT05812833).
Since it is a public hospital, no fee is paid within the scope of health insurance. After an uncomplicated vaginal birth, women remain in the hospital for 24 hours, and 48 hours if they have had a Cesarean delivery.
Istanbul, where the hospital is located the most populous city in Turkey with about 16 million inhabitants, the country. Although approximately 90% of the population are Turkish citizens, the hospital also provides services to individuals from different ethnic groups and races (Syrian, Turkmen, Iranian, Uzbeki). Syrians, who constitute a significant part of the immigrant population in the region, can receive free health services from the hospital where the research was conducted, and from other hospitals affiliated with the Ministry of Health. There are no differences to the treatment and care services provided in terms of race or ethnicity.
Primiparous pregnant women, 32–38 GW, singleton pregnancy, pregnant women who had not attended pregnancy education classes, mothers who had internet access, who could use digital tools (smartphones or computers), who had a healthy baby, whose baby was born at term (between 37–42 GH), mothers who were discharged with their baby, and mothers who had their baby with their mother.
Mother has communication problems, mother has a chronic disease, mother has problems with breastfeeding (breast or newborn), newborn has Intrauterine Growth Retardation or genetic disease, does not attend training sessions.
The sample size of the study was determined using the G*Power (ver. 3.1.7) program, and Cohen standard effect sizes. The minimum sample required for the study was calculated according to a study evaluating the success of nursing interventions in breastfeeding [24], and it was determined that a total of 82 expectant mothers, with at least 41 expectant mothers in each group, should be included in the sample calculation with a 5% alpha margin of error and 95% power. (G*Power 3.1.9.2). Considering the possibility of losses in the sample over time, the study was carried out with 110 individuals, 55 in the intervention group and 55 in the control group.
The researcher who collected the data was not a hospital employee. She visited the hospital 3 days a week between 08.00 AM and 17.00 PM and reached 420 pregnant women. 310 of the women were excluded from the sample because they did not meet the sample selection criteria. A total of 110 mothers were willing to participate and were randomly assigned to either the intervention or the control group in equal numbers via computer-based randomization (https://www.random.org; Fig. 1). In the intervention group, 3 babies of the pregnant women included in the sample were excluded from the study group because their babies were followed up in the intensive care unit with the diagnosis of transient tachypnea of the newborn (TTN) after birth, and in the control group, 5 babies were excluded from the study group because they were followed up in the intensive care unit due to TTN and jaundice. The study was completed with a total of 102 mothers and their babies (intervention group, n=52; control group, n=50). Post hoc analysis performed after the data collection was completed showed that the sampling power was 95% and the sample was adequate.
Readiness for motherhood was assessed to provide information about the transition experiences of the pregnant women included in the study. According to Meleis' transition theory, the most appropriate conditions for transition can be prepared with education. In order for the pregnant women in the intervention group to make a healthy transition to motherhood, it was aimed to prepare them for the role of motherhood with online baby care and breastfeeding training.
The planned education program was applied to the pregnant women in the intervention group during the antenatal period in 2 online sessions. In the first training session, topics such as breastfeeding, the structure of breast milk, advantages of breastfeeding, breastfeeding technique, expressing breast milk, storing expressed milk, infant health monitoring, newborn screening, vaccines, development of emotional bonding with the baby, etc. were explained (approximately 35 minutes). At the end of the session, pregnant women were asked to write a letter to their babies and choose a lullaby.
In the second training session, characteristics of the baby room, safety of the baby, sleep safety, prevention of falls and accidents, common problems (fever, nasal congestion, vomiting, thrush, gas pains, crying, diaper cleaning, umbilical care, etc.) (approximately 20 minutes) were explained. The training was carried out using power point presentation, baby model, breast model, milking pump, milk storage bag, diaper, cotton, etc. demonstration technique. Two videos (approximately 18 minutes) on baby bathing and massage were shown.
The researcher routinely called the mothers once a week until the babies were 3 months old and asked whether they had breastfeeding problems. Mothers were also given the opportunity to reach the researcher at any time when they had problems. The mothers in the control group benefited from the routine services of the clinic and the training documents were sent via Whats-App when the data collection process was over.
A questionnaire was used to collect data regarding the descriptive characteristics of the participants and newborns. These included: the participant’s educational status, delivery method, gestational week, and the infant’s sex, birth weight, length and starting breastfeeding.
The baby monitoring form was developed by the researchers. Expert opinions were obtained to evaluate its face validity. Experts were asked to review the measuring technique and items and evaluate whether they were suitable for measurement. The data obtained with this form were as follows: height, weight, and breastfeeding problems.
Breastfeeding success was evaluated with the "Breastfeeding Diagnosis and Assessment System (LATCH) Scale". The scale was developed by Jensen, Wallece, and Kelsay to evaluate breastfeeding. Its adaptation into Turkish was performed by Yenal and Okumu [25]. In the LATCH scale, 0, 1 or 2 points are given for each criterion. A minimum score of 0 and a maximum score of 10 are obtained from the scale. Scoring is done by observing breastfeeding. The higher the LATCH score, the higher the breastfeeding success. LATCH Cronbach's Alpha value was found to be 0.95 by Yenal and Okumu [25]. In the study group, Cronbach's Alpha value was found to be 0.73.
Readiness for motherhood was evaluated with the "Readiness for Hygienic Care of the Newborn Scale." The scale developed by Çaka and Çınar [26] to assess the readiness of pregnant women for hygienic care of the newborn consists of 10 items. The 7-point Likert-type scale is graded between 1–7, ranging from not ready to completely ready. A minimum score of 10-maximum score of 70 is obtained from the scale. The scale is interpreted over the total score, and high scores indicate that the readiness of the pregnant woman for the care of the newborn is high. Çaka and Çınar [26] found the Cronbach α value of the scale to be 0.93. In the study group, Cronbach α value was found to be 0.73.
Data were collected by the first researcher. The first interview with the participants at 32–38 weeks of gestation was conducted in the pregnancy follow-up outpatient clinic. After the participants in both groups signed the informed consent form, introductory information and the Readiness for Hygienic Care of the Newborn Scale were completed. The Readiness for Hygienic Care of the Newborn Scale and anthropometric measurements of all newborns in the study groups were taken on the first postpartum day (breastfeeding success-LATCH), 1st month, 2nd month, and 3rd month.
The data were analyzed using IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA). Baseline characteristics and outcome variables were compared using appropriate frequencies, percentages, means, and standard deviations. The Kolmogorov-Smirnov test was employed to assess the normality assumption. For the comparison of quantitative data with a normal distribution, the “t-test in independent groups” was applied for the difference between the 2 independent groups, the “t-test in dependent groups” was used for the comparison of 2 dependent variables, and “analysis of variance in repeated measurements” was employed for the comparison of more than 2 dependent variables.In case of a significant difference, the post hoc “Bonferroni” test was utilized to identify the group that contributed to the difference.
The “Mann-Whitney U test” test was applied to measure the difference between the 2 independent groups to compare quantitative data without normal distribution. “Chi-square analysis” was employed for the difference between categorical variables. If the expected value in the cells was less than 5, “Fisher exact test” was applied. Significance was considered at P<0.05.
It was found that the groups were similar in terms of age, educational status, employment status, income, family type, planned pregnancy, gestational age of the baby and sex of the baby (P>0.05) (Table 1).
In the intervention group, the mean total score of the Readiness for Hygienic Care of the Newborn Scale at postpartum, 1st, 2nd, and 3rd months were significantly higher compared to the control group (P<0.001) (Table 2). The change in the scale scores over time in repeated measurements (pregnancy, postpartum period, 1st, 2nd, and 3rd month) of the intervention and control groups was statistically significantly higher (P<0.001)(Table 2).
In the first 24 hours, the mean LATCH total score of the mothers in the intervention group was 8.88±1.04 and 5.32±1.18 in the control group, and the mean score of the intervention group was significantly higher than that of the control group (P<0.001) (Table 3).
It was observed that mothers in the intervention group fed their babies exclusively with breast milk at a statistically significantly higher rate in the postpartum period, 1st month, 2nd month, and 3rd month compared to the control group (P<0.001) (Table 4).
It was found that mothers in the intervention group gave pacifiers at a lower rate in the postpartum period, 1st month, 2nd month, and 3rd month compared to the control group (P<0.001) (Table 5).
There was no statistically significant difference (P>0.05) in the birth length and weight of the babies in the intervention and control groups. The height of the babies was found to be longer in the intervention group than in the control group at the 1st, 2nd, and 3rd months (P<0.05) (Table 6). The weight of the babies was lower in the intervention group compared to the control group at the 2nd and 3rd months (P<0.05)(Table 6). The change in the height and weight of the babies over time in repeated measurements (postpartum, 1st, 2nd, and 3rd month) was found to be statistically significantly higher (P<0.001) (Table 2). The change in the height of the babies in the intervention group over time was not statistically significant (P>0.05) (Table 6).
This study aimed to examine the effects of online baby care education and postpartum counseling based on Meleis's Transition Theory on mothers' readiness for baby care and breastfeeding levels. As a result of the study, it was found that the mothers who received theory-based education and counseling intervention had higher readiness to care for their babies, the average height and weight of the babies in both groups were in the healthy percentile, and the height and weight of the babies in the control group were higher than the babies in the intervention group.
Adaptation, reactions, and perceptions to the changes brought about by pregnancy and motherhood are different. Women's adaptation is influenced by their personal experiences, cultural level, family attitudes, existing physical and mental illnesses, risky situations experienced in previous pregnancies, number of children, voluntary pregnancy status, social support systems, readiness for motherhood, etc. The role of motherhood is defined as a period that begins in the prenatal period and is completed with the formation of a maternal identity in the first year after birth [5,17,19]. In Turkey, 79% of women and 68% of newborns received care within the first 2 days in the postpartum period [27]. The mother needs to adapt to the physiological and psychological changes she experiences, accept her baby, gain sufficient knowledge and skills for her maternal role, and care for herself and her baby [28]. In the literature, it is stated that mothers need information about infant care and that trainings play an important role in improving child health [18,19]. In the research group, it was observed that mothers who received theory-based education and counseling had higher readiness for infant care. In a systematic review, it was determined that the training given to mothers on infant care was effective in preparing them for the role of motherhood [29]. Dol et al. [1] found that mothers' self-efficacy increased with the postpartum mobile support application.
Mothers access information about the care of their babies from the prenatal period through the internet and social media. However, it is known that there is intense information pollution in the digital environment [30]. It was found that 88% of mothers obtained information about baby care on the internet [3]. In a study conducted with Aboriginal women, it was reported that mothers' difficulty in accessing information on infant care negatively affected neonatal health [31]. It is indisputably accepted that health professionals should evaluate the knowledge and skills of expectant mothers regarding infant care and their adaptation to the role of motherhood, and support mothers with education and counseling services, starting in the antenatal period [32]. No study was found in which the effect of online baby care education and postpartum remote counseling support on mothers' preparation for infant care was explained. The results of the study suggest that online education and counseling are effective in preparing mothers for infant care.
Exclusive breastfeeding, especially for the first 6 months, is recommended to protect the health of infants [22]. Breastfeeding is directly associated with infant health. Studies have shown that breastfeeding education during pregnancy and postpartum breastfeeding counseling increase exclusive breastfeeding rates [33-35]. Korkut Öksüz and İnal [33] examined the effect of breastfeeding support provided via WhatsApp on breastfeeding. In Nigeria, Flax et al. [34] evaluated the effect of remote support methods (e.g. telephone, WhatsApp text message or WhatsApp group) on breastfeeding at 6 and 24 weeks postpartum. Sevda and Sevil [33] and Flax et al. [34] found that the duration of exclusive breastfeeding increased in groups supported via WhatsApp. In our study group, it was observed that infants of mothers who received theory-based online infant care education and counseling breastfed more successfully on the first day and were fed exclusively with breast milk at a higher rate in the first 3 months compared to the control group. Our study is the first study we know of in Turkey in which the effects of online infant care education and postpartum remote counseling support on breastfeeding were evaluated. It can be said that online education and postpartum remote counseling support are effective in maintaining exclusive breastfeeding. In our study, it was determined that the height of the babies in the intervention group was statistically significantly higher in the first, second and third months compared to the control group. Repeated measurements showed that there was no difference in the intervention group, whereas the increase in height was significantly higher in the control group. It was determined that the babies in the control group gained more weight than the intervention group in the second- and third-month measurements. Anthropometric values of babies should be within normal limits for a healthy start to life and healthy growth and development. Anthropometric values were within normal limits according to the percentiles determined for Turkish children. The higher weight gain of the babies in the control group in our study may be explained by the low number of breastfed babies. When the relationship between feeding type and weight gain was examined, it was determined that infants who received formula weighed more than breastfed infants [14,15]. In a study comparing the nutritional characteristics and growth of infants, it was determined that there was a relationship between exclusive breastfeeding rates and body weight, height, and BMI z score [14]. In a randomized controlled study, it was determined that infants of mothers who were given breastfeeding education and counseling for 6 months were fed more breast milk and had higher height and weight [35]. It can be said that online education and postpartum counseling support positively affect the growth of babies.
The study could not be double-blinded due to its nature. The data were obtained by the researcher. Since the participants and the researcher were not blinded to each other, some participants in the intervention group may have reported more favorable outcomes. The results of the study are limited to the data of 102 mothers and their babies who were followed up in the pregnancy follow-up outpatient clinic of a public hospital. The fact that the study was conducted with mothers who had internet access and was conducted in a single center can be considered as other limitations.
In this study, due to the pandemic, participants in the control group may have been less supported by healthcare professionals than usual. To minimize this limitation, the researcher had to answer the questions of the participants in the control group during the interviews or refer those who needed face-to-face counseling to infant health follow-up clinics.
In conclusion, theory-based online education initiated during pregnancy and ongoing counseling up to 3 months postpartum positively affected mothers' preparation for infant care. Mothers who received training and counseling breastfed their babies more successfully on the first day and exclusively breastfed at a higher rate in the first 3 months. Online infant care education and counseling can be considered as an alternative to standard care, especially when face-to-face support is not available.
Footnotes
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Fig. 1.
Flow diagram of the study (CONSORT 2018). NICU, neonatal intensive care unit; TTN, transient tachypnea of the newborn.
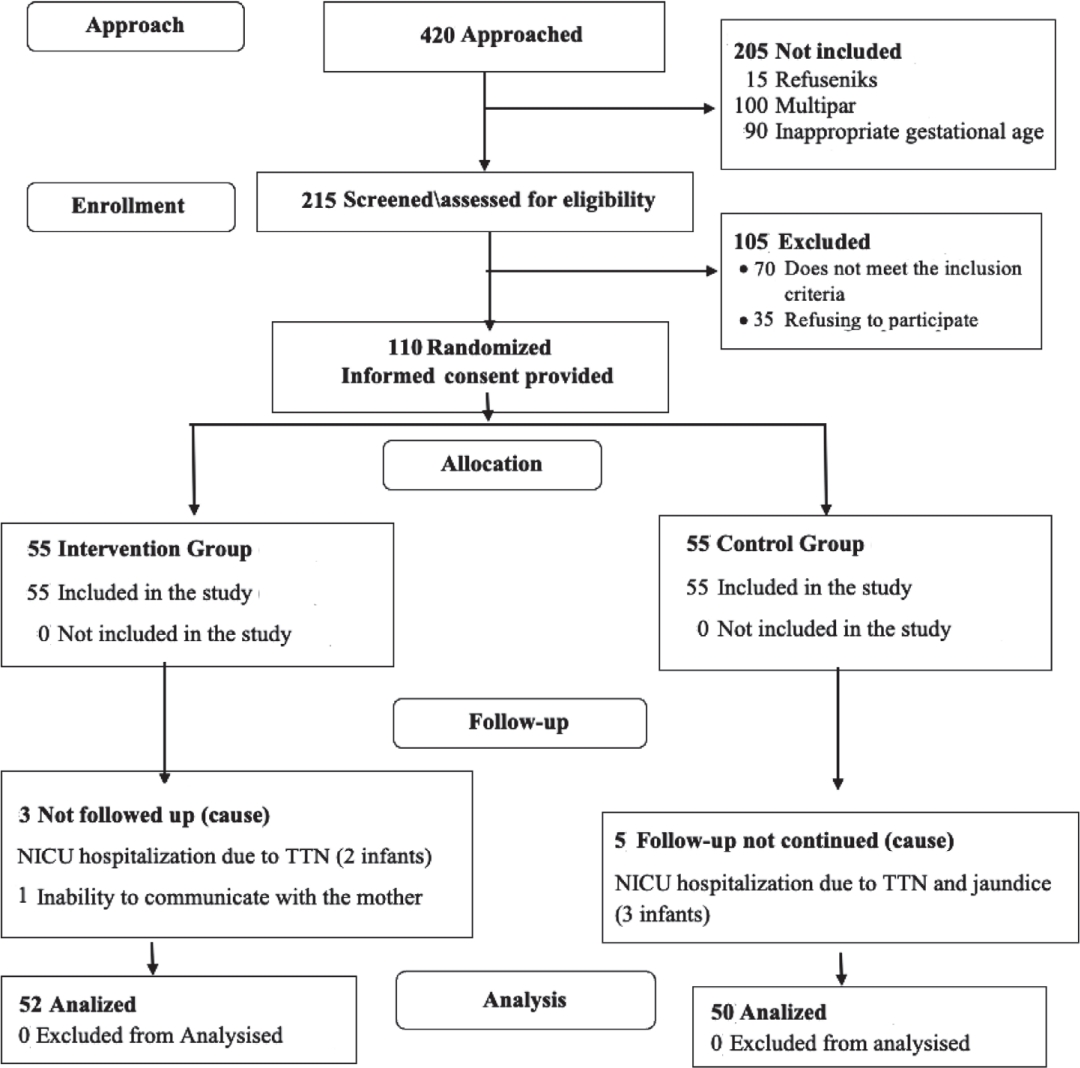
Table 1.
Distribution and comparison of socio-demographic and obstetric characteristics of mothers and infants according to groups (N=102)
| Variable | Intervention group (n=52) | Control group (n=50) | Test | P value |
|---|---|---|---|---|
| Mother age (yr) | 26.35±3.71 (19–35) | 26.88±4.14 (19.00–35.00) | 1,249.50a) | 0.734 |
| Gestation age (wk) | 39.03±1.02 (37.00–41.00) | 38.78±1.21 (37.00–41.00) | 1,126.00a) | 0.225 |
| Education status | ||||
| Primary school | 11 (21.2) | 10 (20) | ||
| High school | 16 (30.8) | 16 (32) | 0.290b) | 0.986 |
| University and above | 25 (48.1) | 24 (48) | ||
| Working status | ||||
| Working | 14 (26.9) | 22 (44) | 3.255b) | 0.071 |
| Not working | 38 (73.1) | 28 (56) | ||
| Revenue status | ||||
| Income less than expense | 13 (25) | 15 (30) | ||
| Income equals expense | 26 (50) | 22 (44) | ||
| Income is more than expense | 13 (25) | 13 (26) | 0.437b) | 0.804 |
| Family type | ||||
| Nuclear | 46 (88.5) | 40 (80) | 1.380b) | 0.240 |
| Wide | 6 (11.5) | 10 (20) | ||
| Planned pregnancy | ||||
| Planning | 49 (94.2) | 42 (84) | 2.773b) | 0.960 |
| Not planning | 3 (5.8) | 8 (16) | ||
| Type of birth | ||||
| Cesarian | 33 (63.5) | 29 (58) | 0.319b) | 0.102 |
| Vaginal birth | 19 (36.5) | 21 (42) | ||
| Sex of the baby | ||||
| Girl | 27 (51.9) | 17 (34) | 3.338b) | 0.68 |
| Boy | 25 (48.1) | 33 (66) |
Table 2.
Comparison of mothers' Readiness for Hygienic Care of the Newborn Scale scores according to months (N=102)
| Follow-ups | Intervention group (n=52) | Control group (n=50) | Test | P value |
|---|---|---|---|---|
| Pregnant (1) | 24.90±7.88 (10–39) | 24.86±8.81 (10–42) | 12.638a) | 0.830 |
| Postpartum (2) | 59.15±7.97 (39–70) | 37.28±4.91 (24–45) | 54.000a) | <0.001 |
| 1st month (3) | 62.30±6.62 (39–70) | 54.28±8.17 (30–70) | 508.500a) | <0.001 |
| 2nd month (4) | 65.50±4.73 (51–70) | 56.80±9.32 (22–69) | 365.000a) | <0.001 |
| 3rd month (5) | 67.69±1.97 (63–70) | 58.02±6.14 (35–67) | 49.500a) | <0.001 |
| Test | 217.172b) | 532.638b) | ||
| P value | <0.001 | <0.001 | ||
| Bonferroni | 1<2; 1<3; 1<4; 1<5; 2<3; 2<4; 2<5; 3<4; 3<5; 4<5 | 1<2; 1<3; 1<4; 1<5; 2<3; 2<4; 2<5 |
Table 3.
Comparison of LATCH Breastfeeding Diagnosis and Assessment Scale Scores by groups (N=102)
| Intervention group (n=52) | Control group (n=50) | Test | P value | |
|---|---|---|---|---|
| LATCH total score | 8.88±1.04 (7.00–10.00) | 5.32±1.18 (2.00–8.00) | 49.500a) | <0.001 |
Table 4.
Comparison of infants' feeding patterns by groups (N=102)
| Baby’s diet | Intervention group (n=52) | Control group (n=50) | Test | P value |
|---|---|---|---|---|
| Postpartum | ||||
| Breast milk only | 50 (96.2) | 26 (52) | 26.165a) | <0.001 |
| Breast milk+formula | 2 (3.8) | 24 (48) | ||
| 1st month | ||||
| Breast milk only | 52 (100) | 25 (50) | ||
| Breast milk+formula | 0 (0) | 21 (42) | 38.829b) | <0.001 |
| Formula | 0 (0) | 4 (8) | ||
| 2nd month | ||||
| Breast milk only | 51 (98.1) | 28 (56) | 27.371b) | <0.001 |
| Breast milk+formula | 1 (1.9) | 17 (34) | ||
| Formula | 0 (0) | 5 (10) | ||
| 3rd month | ||||
| Breast milk only | 50 (96.2) | 25 (50) | ||
| Breast milk+formula | 2 (3.8) | 16 (32) | 29.720b) | <0.001 |
| Formula | 0 (0) | 9 (18) |
Table 5.
Comparison of pacifier status by groups (N=102)
| Baby’s diet | Intervention group (n=52) | Control group (n=50) | Test | P value |
|---|---|---|---|---|
| Postpartum | ||||
| Yes | 0 (0) | 31 (62) | 46.317a) | <0.001 |
| No | 52 (100) | 19 (38) | ||
| 1st month | ||||
| Yes | 5 (9.6) | 38 (76) | 46.067a) | <0.001 |
| No | 47 (90.4) | 12 (24) | ||
| 2nd month | ||||
| Yes | 4 (7.7) | 23 (46) | 19.219a) | <0.001 |
| No | 48 (92.3) | 27 (54) | ||
| 3rd month | ||||
| Yes | 4 (7.7) | 24 (48) | 20.795a) | <0.001 |
| No | 48 (92.3) | 26 (52) |
Table 6.
Comparison of anthropometric measurements of infants according to groups (N=102)
| Measurements |
Intervention group (n= 52) |
Control group (n=50) |
Test | P value | ||
|---|---|---|---|---|---|---|
| Mean±SD | Range | Mean±SD | Range | |||
| Height (cm) | ||||||
| Birth (1) | 50.75±2.26 | 42.00–54.00 | 50.66±1.92 | 47.00–57.00 | 1,113.000a) | 0.203 |
| 1st month (2) | 53.07±2.26 | 45.00–57.00 | 52.62±1.96 | 49.00–60.00 | 1,011.000a) | 0.050 |
| 2nd month (3) | 55.00±2.03 | 47.00–59.00 | 54.30±1.95 | 52.00–61.00 | 900.000a) | 0.007 |
| 3rd month (4) | 57.23±1.77 | 51.00–61.00 | 56.80±1.61 | 55.00–62.00 | 1,012.000a) | 0.049 |
| Test | 1.212b) | 1,192.755b) | ||||
| P value | 0.274 | <0.001 | ||||
| Bonferroni | 1<2, 1<3, 1<4,1, 2<3, 2<4, 3<4 | 1<2, 1<3, 1<4,1, 2<3, 2<4. 3<4 | ||||
| Weight (g) | ||||||
| Birth (1) | 3,295.61±357.06 | 2,500.00–4,000.00 | 3306.40±334.22 | 2,500.00–4,000.00 | 1,283.000a) | 0.909 |
| Discharge (2) | 2,903.86±1,018.39 | 2,450.00–3,850.00 | 3012.84±948.58 | 2,450.00–3,980.00 | 1,217.500a) | 0.581 |
| 1st month (3) | 4,120.84±696.20 | 3,210.00–4,920.00 | 4214.20±386.23 | 3,200.00–4,950.00 | 1,241.500a) | 0.695 |
| 2nd month (4) | 5,234.90±445.30 | 4,000.00–6,200.00 | 5397.00±387.85 | 4,350.00–6,300.00 | 1,000.500a) | 0.045 |
| 3rd month (5) | 6,170.38±465.43 | 5,100.00–6,980.00 | 6619.20±419.03 | 5,350.00–7,280.00 | 581.000a) | <0.001 |
| Test | 4.340b) | 845.334bb) | ||||
| P value | 0.040 | <0.001 | ||||
| Bonferroni | 1<3, 1<4, 1<5, 2<1, 2<3,2<4,2<5, 4<5 | 1<3, 1<4, 1<5, 2<1, 2<3,2<4,2<5, 4<5 | ||||
References
1. Dol J, Richardson B, Murphy GT, Aston M, McMillan D, Campbell-Yeo M. Impact of mobile health interventions during the perinatal period on maternal psychosocial outcomes: a systematic review. JBI Evid Synth 2020;18:30–55.


2. Yılmaz Bursa Ö, Aksoy AB. Investigation of parental self-regulation competencies of mothers with 0–1-year-old babies according to some variables. Kalem Int J Educ Human Sci 2023;13:257–75.
3. Yıldız H, Boyacı B. Mothers' knowledge levels about pre-discharge neonatal care, their needs and related factors in the postpartum period. Mersin Univ J Health Sci 2019;12:1–10.
4. Meighan M. Mercer's becoming a mother theory in nursing practice. In: Alligood MR, editor. Nursing theory: utilization & application. 5th ed. New York: Mosby, 2013.
5. Meleis A. Transitions theory: middle range and situation spesific theories in nursing research and practices. New York: Springer Publishing, 2010.
6. Öztürk Öztürk, Erci B. Primipar mothers in postpartum period given maternity and newborn education increased attachment: posttest with control group semi experimental research. Balıkesır Health Sci J 2016;5:129–34.

7. Durmaz A, Gün Kakaşçı Ç, Başar F. The relationship of postpartum maternal attachment and mothers' happiness levels with sociodemographic and obstetric characteristics: a cross-sectional study. Turk Klinikleri J Nurs Sci 2021;13:17–22.
8. Hajeebhoy N, Nguyen PH, Mannava P, Nguyen TT, Mai LT. Suboptimal breastfeeding practices are associated with infant illness in Vietnam. Int Breastfeed J 2014;9:12.




9. Mukunya D, Tumwine JK, Nankabirwa V, Ndeezi G, Odongo I, Tumuhamye J, et al. Factors associated with delayed initiation of breastfeeding: a survey in Northern Uganda. Glob Health Action 2017;10:1410975.




10. Woldie TG, Kassa AW, Edris M. Assessment of exclusive breastfeeding practice and associated factors in Mecha District, Northwest Ethiopia. Sci J Public Health 2014;2:330–6.

11. Barimani M, Vikström A, Rosander M, Forslund Frykedal K, Berlin A. Facilitating and inhibiting factors in transition to parenthood - ways in which health professionals can support parents. Scand J Caring Sci 2017;31:537–46.



12. Shorey S, Ng YPM, Ng ED, Siew AL, Mörelius E, Yoong J, et al. Effectiveness of a technology-based supportive educational parenting program on parental outcomes (part 1): randomized controlled trial. J Med Internet Res 2019;21:e10816.



13. Cox JE, Harris SK, Conroy K, Engelhart T, Vyavaharkar A, Federico A, et al. A parenting and life skills intervention for teen mothers: a randomized controlled trial. Pediatrics 2019;143:e20182303.



14. Altinba Z, Güldemir HH, Garipa ao lu M. Evaluation of nutrition and growth-development status of six-12-month-old infants. J Child 2020;20:13–9.
15. Yolda H, Dinçer T, Garipa o lu M. Evaluation of growth, development and nutritional characteristics of 0-6 month old babies. J Health Acad 2021;8:29–35.
16. Khodabandeh F, Mirghafourvand M, KamaliFard M, Mohammad-Alizadeh-Charandabi S, Asghari Jafarabadi M. Effect of educational package on lifestyle of primiparous mothers during postpartum period: a randomized controlled clinical trial. Health Educ Res 2017;32:399–411.


18. Güzel A, Uçan Yamaç S, Kara F. The evaluation of the applications used in baby care by the mothers with first babies. Balıkesır Health Sci J 2017;6:108–17.

19. Horwood C, Butler L, Barker P, Phakathi S, Haskins L, Grant M, et al. A continuous quality improvement intervention to improve the effectiveness of community health workers providing care to mothers and children: a cluster randomised controlled trial in South Africa. Hum Resour Health 2017;15:39.




20. Nawabi F, Alayli A, Krebs F, Lorenz L, Shukri A, Bau AM, et al. Health literacy among pregnant women in a lifestyle intervention trial: protocol for an explorative study on the role of health literacy in the perinatal health service setting. BMJ Open 2021;11:e047377.



21. Zibellini J, Muscat DM, Kizirian N, Gordon A. Effect of health literacy interventions on pregnancy outcomes: a systematic review. Women Birth 2021;34:180–6.


22. World Health Organization. Postpartum care of the mother and newborn 2013. Geneva (Switzerland): World Health Organization, 2013.
23. Sawyer MG, Reece CE, Bowering K, Jeffs D, Sawyer ACP, Mittinty M, et al. Nurse-moderated internet-based support for new mothers: non-inferiority, randomized controlled trial. J Med Internet Res 2017;19:e258.



24. Necipoğlu D, Bebiş H, Seviğ Ü. The effect of nursing interventions on immigrant women living in Northern Cyprus on their breastfeeding self-efficacy and success: a randomized controlled trial. Health Care Women Int 2021;42:235–47.


25. Yenal K, Okumus H. LA study examining the reliability of the ATCH Breastfeeding diagnostic scale. HEMAR-G J 2003;5:38–44.
26. Çaka SY, Çınar N. Development of the scale of readiness of pregnant women for hygienic care of the newborn, validity and reliability study. Dokuz Eylül Univ Fac Nurs Electron J 2020;13:10–8.
27. Hacettepe University Institute of Population Studies. Turkey demographic and health survey advanced analysis report. Ankara (Turkey): Hacettepe University Institute of Population Studies, 2018.
28. Yılmaz A, Bayar A, Esenay FI. Determination of mothers' postpartum infant care needs: a qualitative study. Mersin Univ J Health Sci 2018;11:147–56.
29. Sayık D, Örsal Ö. Parents' self-confidence in infant care and influencing factors in Turkey: a systematic review. Osmangazi Tıp Dergisi 2019;41:434–47.
30. Aryani EI, Lindawati YI. Single parent women's strategy in providing children's education needs: a case study on village women. J Gend Child Prim Stud 2023;1:49–59.
31. Simpson N, Wepa D, Bria K. Improving antenatal engagement for Aboriginal women in Australia: A scoping review. Midwifery 2020;91:102825.


32. Özkan T, Çankaya S. Pregnancy adaptation and prenatal attachment levels of pregnant women with and without the threat of preterm birth. Selcuk J Health 2023;4:256–74.
33. Sevda KÖ, Sevil İ. Continuous lactation support provided through the whatsapp messaging application: a randomized controlled trial. J Hum Lact 2023;39:666–78.



34. Flax VL, Ipadeola A, Schnefke CH, Ralph-Opara U, Adeola O, Edwards S, et al. Breastfeeding interpersonal communication, mobile phone support, and mass media messaging increase exclusive breastfeeding at 6 and 24 weeks among clients of private health facilities in Lagos, Nigeria. J Nutr 2022;152:1316–26.









 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


