Article Contents
| Clin Exp Pediatr > Volume 68(2); 2025 |
|
Abstract
Background
Pediatric migraines are primarily treated with medications. However, recognizing the triggers related to patient behaviors and lifestyle is also important.
Methods
This study included 102 pediatric patients with migraine diagnosed using the third edition of the International Classification of Headache Disorders who visited our pediatric headache clinic between November 2021 and October 2022. We reviewed the patients’ clinical features, imaging studies, screening tests for behaviors and emotions, and questionnaires regarding triggers. Statistical analyses were performed using the independent sample Student t test and linear-by-linear association test.
Results
The 102 patients (44 males, 58 females; mean age, 12.0±2.9 years) were classified into migraine without aura (n=58) and migraine with aura (n=44) groups. Sleep disturbances were the most frequent trigger (76.5%). Other triggers included academic stress (66.7%), motion sickness (62.7%), and fatigue (52.9%). Academic stress was the most significant trigger for pain severity in 44.1% of patients. Abnormal behavioral or psychiatric assessment results were associated with a higher number of triggers.
Graphical abstract. MWOA, migraine without aura.
Headache is a significant disorder that can affect the quality of life of children and adolescents and may even contribute to disabilities.1) Chronic headaches can have various harmful effects on a patient’s life, leading to school absences, decreased academic performance, and impaired social relationships such as friendships. In Korea, the one-year prevalence of headaches among schoolchildren is 29.1%, including 8.7% for migraines, 13.7% for tension-type headaches, and 6.7% for other types [2].
Many triggers are known to provoke migraine attacks, including stress, dietary factors, and environmental changes [3]. Additionally, gastrointestinal issues like constipation have also been identified as significant factors influencing headache symptoms in children and adolescents [4]. A detailed understanding of these factors may help the clinical management of migraines. Although the identification of trigger factors is often recommended as a basic strategy for migraine treatment, clinicians frequently rely on medications. Moreover, a lack of systematic analysis, particularly in pediatric cases with uncertain self-reporting, hinders comprehensive research [3,5,6].
The role of nonpharmacological interventions in the management of pediatric headaches has gained significant attention. Lifestyle modifications, including maintaining regular sleep patterns and making dietary adjustments, have been shown to reduce the frequency and severity of headaches [7]. Additionally, research on academic stress and its impact on adolescents' overall well-being has shown that academic stress can significantly lower life satisfaction and increase depression [8]. And, recent studies indicate that the COVID-19 pandemic can have long-term negative effects on the mental health of children and adolescents [9]. These mental health issues may, in turn, exacerbate physical symptoms like headaches, suggesting the need for a holistic approach to managing pediatric headaches that includes mental health support and lifestyle adjustments.
Therefore, this study aimed to evaluate the factors that trigger migraine and identify the most significant factors that could contribute to the management of pediatric migraine.
We retrospectively reviewed the data of 102 patients who visited the headache clinic of Hallym University Kangnam Sacred Heart Hospital between November 2021 and October 2022. subjects aged 5-18 years with migraine without aura (MWOA) and migraine with aura (MWA) were diagnosed according to the criteria of the third edition of the International Classification of Headache Disorders (ICHD-III) [10].
Among the 199 patients with headaches who visited our clinic during the study period, 92 patients with secondary or other headaches were excluded. Five additional participants were excluded because they did not respond to the trigger factor questionnaire.
We recorded biographical data, lifestyle characteristics, general medical history, and family history for the baseline survey. Headache-related characteristics such as frequency, intensity, clinical characteristics, and duration were also documented. Imaging studies (e.g., brain magnetic resonance imaging and cervical spine radiography) have been conducted. Behavioral and psychiatric screening tests such as the Korean Child Behavior Checklist (K-CBCL), State Anxiety Inventory for Children (SAIC), Trait Anxiety Inventory for Children (TAIC), and Children's Depression Inventory (CDI), were also performed.
The participants were asked to choose their potential trigger factors based on their previous experiences using our questionnaire, which was developed based on the triggers identified in previous studies reported in the literature [3,5,11,12]. The questionnaire included questions regarding 24 trigger factors: sleep disturbance, academic stress, family conflict, romantic relationship issues, smartphone use, hunger, migraine-triggering foods, caffeine sensitivity, physical inactivity, overexercise, fatigue, medication overuse, bright light, noise, strong odors, introverted or extroverted personality, anxiety, depression, hot or cold weather, menstruation, obesity, and motion sickness. We provided subcategories for more detailed responses to academic stress, family conflict, and sleep disturbance. Moreover, while patients were encouraged to identify all the triggers applicable to them, they were asked to rank the triggers based on the magnitude of their impact on individual well-being. This approach acknowledges the potential variation in the influence of different trigger factors, recognizing that not all triggers affect patients equally (Supplementary material 1).
Statistical analyses were conducted using IBM SPSS Statistics ver. 28.0 (IBM Co., Armonk, NY, USA). The independent samples Student t test was used to compare the headache characteristics between the 2 groups. A linear-by-linear association analysis was used to investigate the relationship between the risk of academic stress and patient age. The study used statistical methods, including the Mann-Whitney U test, correlation analysis, and regression analysis, to examine the relationship between trigger factors and behavioral/psychiatric measures, such as the K-CBCL, SAIC, TAIC, and CDI. Statistical results were considered significant if P<0.05. All P values were 2-tailed.
This study was reviewed and approved by the Institutional Review Board of the Hallym University Kangnam Sacred Heart Hospital (2023-08-005). Given its retrospective nature, this study was exempt from the need for informed consent from participants.
The 102 patients (male-to-female ratio=44:58) had a mean age of 12.0±2.9 years and were divided into 2 groups: MWOA (n=58) and MWA (n=44). Of the 58 MWOA patients, 24 (41.4%) and of the 44 MWA patients, 17 (38.6%) meet the criteria for chronic migraine. No significant differences were found in age, headache severity, or number of trigger factors between the 2 groups. The frequency of headaches was significantly higher in the MWA group, with an average of 17.4±18.5/mo compared to the MWOA group (15.6±11.2/mo) (P=0.045). Furthermore, the duration of headaches was also significantly longer in the MWA group, with an average of 13.1±17.5 hours, compared to the MWOA group (8.9±9.8 hours) (P=0.030) (Table 1).
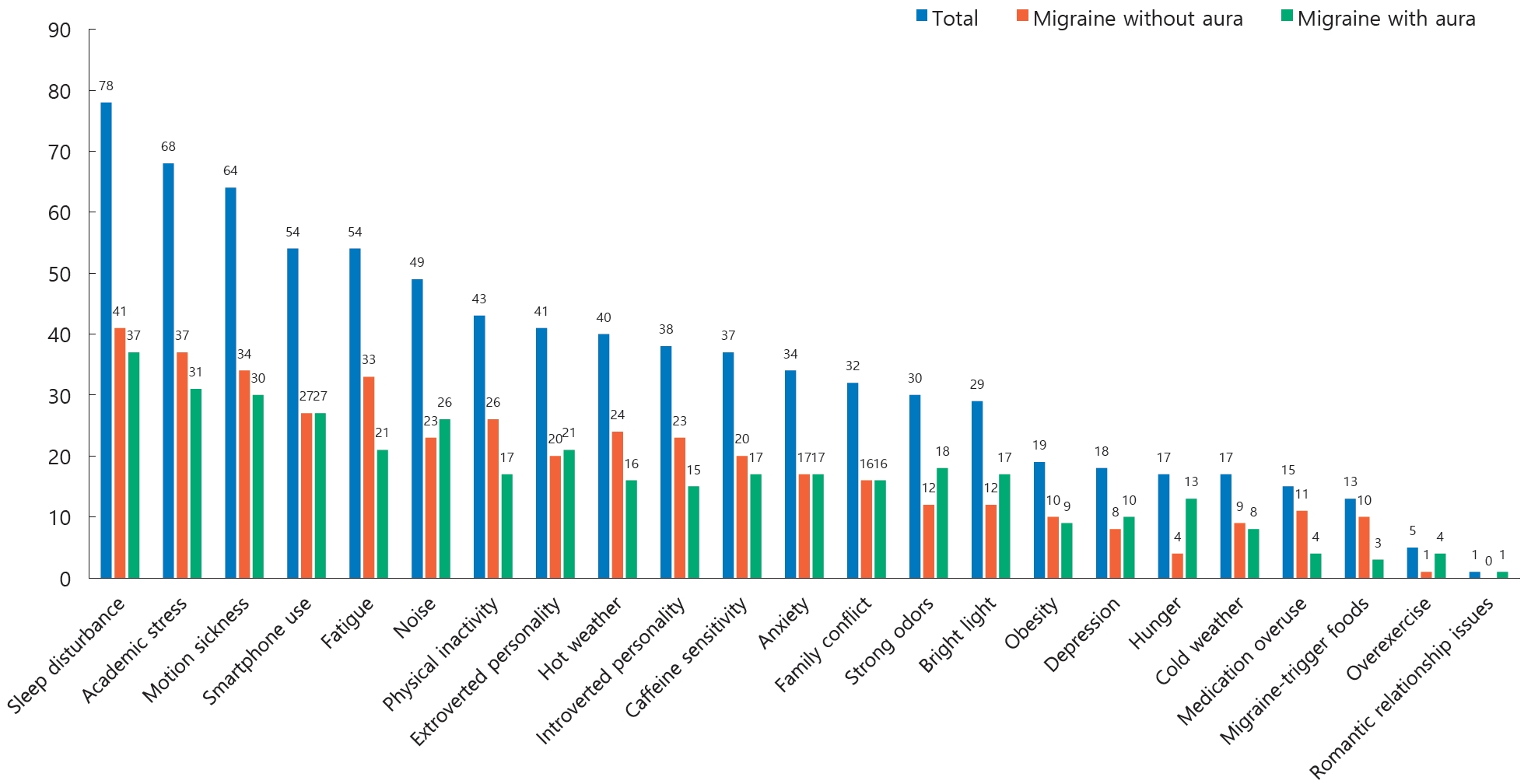
Patients were asked to select all the options on the headache trigger questionnaire that applied to them. Sleep disturbance (76.5%, n=78 of 102) was the most frequent trigger factor in both groups (MWOA: 70.7%, n=41 of 58; MWA: 84.1%, n=37 of 44). The other common triggering factors, in order of frequency, were academic stress (66.7 %, n=68 of 102), motion sickness (62.7%, n=64 of 102), and fatigue (52.9%, n=54 of 102; Fig. 1). Of the 58 female patients, 25 (43.1%) reported that their headaches were triggered by menstruation. It should be noted that the study did not specifically determine how many of these patients had experienced menarche.
When comparing the frequency of trigger factors between the MWOA group and the MWA group, sleep disturbance was reported by 70.7% (n=41 of 58) of MWOA patients, followed by academic stress (63.8%, n=37 of 58), motion weakness (58.6%, n=34 of 58), fatigue (56.9%, n=33 of 58), and smartphone use (46.6%, n=27 of 58). In the MWA group, sleep disturbance was reported by 84.1% (n=37 of 44) of the patients, followed by academic stress (70.5%, n=31 of 44), motion weakness (68.2%, n=30 of 44), smartphone use (61.4%, n=27 of 44, and noise (59.1%, n=26 of 44).
We categorized the trigger factors for sleep disturbance into the following 5 subcategories: lack of sleeping hours, irregular sleeping hours, daytime sleepiness, difficulty falling asleep, and frequent awakening during sleep. Among the 102 patients, 43 (42.2%) reported daytime sleepiness as the most frequent factor, followed by 42 (41.2%), 37 (36.3%), 35 (34.3%), and 22 (21.6%) who reported irregular sleeping hours, lack of sleeping hours, difficulty falling asleep, and frequent awakening during sleep, respectively. In the MWOA group, 23 patients (39.7%, n=23 of 58) reported daytime sleepiness and irregular sleeping hours as the predominant factors. Subsequently, 21 patients (36.2%, n=21 of 58) reported difficulty falling asleep, 16 (27.6%, n=16 of 58) reported lack of sleeping hours, and 11 (19.0%, n=11 of 58) reported frequent awakening during sleep. In the MWA group, lack of sleeping hours was the most frequently reported factor in 21 patients (47.7%, n=21 of 44), followed by daytime sleepiness in 20 (45.5 %, n=20 of 44), irregular sleeping hours in 19 (43.2%, n=19 of 44), difficulty falling asleep in 14 (31.8 %, n=14 of 44), and frequent awakening during sleep in 11 (25 %, n=11 of 44).
Academic stress, the second most prevalent triggering factor, was categorized into 5 subcategories: academic performance, academic workload, teacher relationships, friendships, and issues with private tutoring. Among the 78 patients who selected academic stress as a trigger, 35 (44.9%) reported academic performance as the most frequent factor, followed by 27 (34.6%) reporting friendships, 24 (30.8%) issues with private tutoring, 16 (20.5%) academic workload, and 6 (7.7%) teacher relationships. Among the 37 patients in the MWOA group reporting academic stress as a trigger, 17 (45.9%) reported issues with private tutoring, 16 (43.2%) reported friendships, 13 (35.1%) reported academic performance, 11 (29.7%) reported academic workload, and 3 (8.1%) reported teacher relationships. Among the 31 patients in the MWA group, 22 (71.0%) reported academic performance, 11 (35.5%) reported friendships, 7 (22.6%) reported issues with private tutoring, 5 (16.1%) reported academic workload, and 3 (9.7 %) reported teacher relationships.
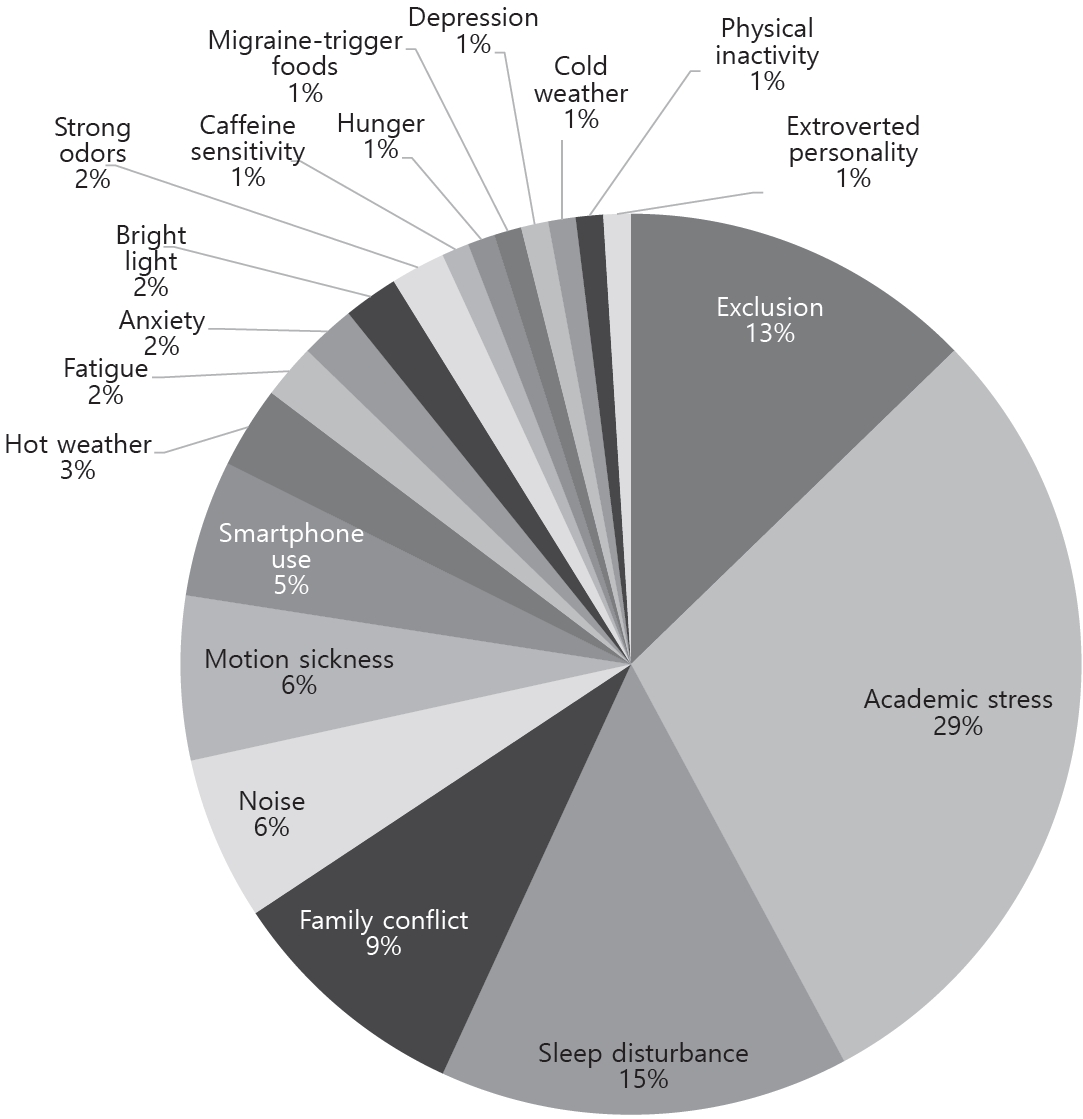
We examined 89 patients to identify the trigger factors that exerted the most intense impact on each individual. An additional 13 patients whose strongest trigger factors could not be assessed were excluded from the analysis. Of the remaining 89 patients, 30 reported academic stress as the most intense trigger factor, accounting for 44.1% of the 68 patients who identified academic stress as a trigger and 29.4% of the total 102 patients. Other intense triggering factors included sleep disturbances (14.7%, n=15 of 102), family conflict (8.8%, n=9 of 102), motion sickness (5.9%, n=6 of 102), noise (5.9%, n=6 of 102), and smartphone use (4.9%, n=5 of 102; Fig. 2).
Our linear-by-linear association analysis indicated that the risk of academic stress as a migraine-triggering factor tended to increase with age (P=0.023). Two patients without academic performance scale data were excluded after a comparative analysis using an independent sample Student t test on the T value of the K-CBCL academic performance scale in 100 patients. Participants were divided into those who chose academic stress as a triggering factor and those who did not. The mean T value of the academic performance scale in the patients who selected academic stress as a trigger factor was significantly lower, at 50.1±7.6, compared to those who did not consider it a trigger factor, with a mean score of 55.7±7.0 (P<0.001). Regression analysis revealed that patients who selected academic stress as a trigger factor complained of longer (P<0.05) and more frequent (P<0.05) headaches. Specifically, those who selected academic stress and fatigue as triggering factors complained of headaches more frequently (P<0.05).
Behavioral and psychiatric problems were assessed using the K-CBCL, SAIC, TAIC, and CDI. To compare the number of trigger factors, the patients were divided into 2 groups based on their test results: one group fell within the normal range, and the other fell outside. After conducting an analysis using the Mann-Whitney U test, it was reported that the number of trigger factors was significantly higher in all patients who fell outside the normal range (Table 2).
The T value of the total problem scores on the K-CBCL and the number of trigger factors showed a significant positive correlation in our correlation analysis (r=0.312; P=0.001) (Fig. 3).
Migraine is one of the most significant types of primary headaches. It can greatly affect the lives of school-aged children, possibly lowering their quality of life and, in some cases, causing disability [1]. Additionally, various trigger factors, such as stress and fatigue, can induce migraine attacks [3]. Therefore, it is crucial to identify, prevent, or manage the triggers that may cause these diseases.
Our study explored the triggering factors associated with pediatric migraine. Sleep disturbance, academic stress, motion sickness, and fatigue are the most frequently reported triggers. Among females, menstruation was a notable trigger, ranking lower than noise but higher than physical inactivity. In a study focusing on 101 pediatric patients with migraines in France, researchers found that lack of sleep (51.4%), stress (44.6%), warm climate (41.9 %), noise (32.4%), and excitement (29.7%) were the most commonly reported trigger factors [13]. Another study indicated that stress (75.5% of 102 patients) was the most common individual trigger, followed by a lack of sleep (69.6%), warm climate (68.6%), and video games (64.7%). Stress has also been consistently reported as a frequent trigger associated with migraine attacks (24.5%) [14].
However, it is worth noting that trigger factors may vary regionally in terms of frequency and significance. For instance, in a study conducted in Eastern India, where the climate is generally mild and rainy, exposure to sunlight and hot, humid weather was identified as a common trigger, accounting for 94% of cases (n=188 200) [15]. Building on this insight, a cross-cultural study of patients residing in Korea could be meaningful for future research. Specifically, exploring the potential differences in the types and frequencies of trigger factors among patients who grow up in various cultures and regions outside Korea may offer valuable insights.
In this study, sleep disturbance was the most prevalent trigger in the MWOA and MWA groups. This aligns with the findings of a previous study that explored the prevalence and characteristics of headaches in a teenage population and their associations with comorbidities and lifestyle. Among students with headaches in that study, shorter sleep times (7.6±1.1 vs. 7.9±1.1 hours, P<0.01) and a higher prevalence of non-regular sleeping habits, insomnia, daytime sleepiness, and unrestful sleep were reported (P<0.001) [16]. In our study, daytime sleepiness was identified as the primary factor in 42.2% of the patients, followed by irregular sleeping hours in 41.2% (n=42 of 102).
Of the 89 patients who selected the most intense trigger factors, 30 identified academic stress as the primary trigger. Interestingly, this corresponded to 44.1% of the 68 participants who categorized academic stress as a trigger. The 15 patients who selected sleep disturbance as the most intense factor constituted 19.2% of the 78 patients who identified sleep disturbance as a trigger. This indicates a distinction between the common trigger factors that patients perceive as triggering headaches and those that patients experience as the most potent triggers of their migraines.
Academic stress emerged as the primary trigger of headaches, and the likelihood of academic stress serving as a trigger increased with age (P=0.023). Individuals who identified academic stress as a trigger not only demonstrated lower levels of academic performance (P<0.001) but also reported more frequent (P<0.05) and prolonged headaches (P<0.05). Furthermore, in a study involving high school students from South Korea and Sweden, a survey analysis indicated that both groups experienced a certain stress level, with Korean students appearing to experience higher stress levels than their Swedish counterparts [17]. Therefore, gaining a deeper understanding of students' levels of academic stress and seeking possible means of addressing it are essential in Korea.
Anxiety was identified as a trigger in 29.3% of the patients, whereas depression was identified as a trigger in 13.8 %. In the K-CBCL, SAIC, TAIC, and CDI evaluations, patients who fell within the abnormal range exhibited more trigger factors than those in the normal range. A previous study involving 61,375 adolescents in Canada also reported an association between migraines and mood/anxiety disorders [18]. Another study has identified anxiety sensitivity as a predictor of headache pain, headache-related disability, and perceived trigger susceptibility [5]. Considering the associations observed in studies on migraine and psychiatric factors, there is a need to incorporate psychiatric considerations into the management of migraines.
In the present study, an increased number of triggers did not necessarily correlate with increased pain severity. However, other studies have revealed a contrasting pattern, as headaches associated with triggers were linked to greater pain intensity (P<0.001). Specifically, participants who reported headaches that were not associated with triggers (n=327) reported a mean visual analogue scale (VAS) score of 3.9±2.0, whereas those who reported headaches associated with triggers (n=772) reported a mean VAS score of 4.6±2.3 [19].
The major limitation of this study was the inaccuracy of recall. A more precise investigation could have been achieved if participants had evaluated and reported their triggers each time a headache occurred. A previous study on adults used the results reported through a smartphone-based headache diary application [19]. Therefore, using a real-time recording method via a headache diary application for children and adolescents is beneficial.
In conclusion, this study significantly advances our understanding of pediatric patients with migraines. The identification of sleep disturbance, academic stress, motion sickness, and fatigue as frequent trigger factors enhanced our insight into migraine triggers in the pediatric population. Academic stress emerged as the most intense trigger, and its impact intensified with age.
This study's exploration of the intricate connections between psychiatric factors, such as anxiety and depression, and migraine triggers offers a comprehensive perspective. This examination underscores the interplay between mental health and migraines and emphasizes the importance of comprehensive care.
Furthermore, it is crucial to recognize that common and intense triggers vary among patients. This insight prompts reconsidering trigger management strategies, highlighting the need for personalized interventions that align with each patient’s specific trigger factors.
Understanding these trigger factors is vital for clinicians to manage patients with migraines. Counseling patients to alleviate specific triggers, such as sleep disturbances and stress, and promote overall lifestyle improvements is recommended for optimal clinical care.
Supplementary material
The supplementary material 1 for this article is available at https://doi.org/10.3345/cep.2024.00738.
Footnotes
Acknowledgments
The authors express their gratitude to the participants who participated in the study.
Fig. 3.
Correlation between total problem scores in Korean Child Behavior Checklist and the number of triggers.

Table 1.
Patients' demographic variables by migraine status
References
1. Raucci U, Boni A, Evangelisti M, Della Vecchia N, Velardi M, Ursitti F, et al. Lifestyle modifications to help prevent headache at a developmental age. Front Neurol 2021;11:618375.



2. Rho YI, Chung HJ, Lee KH, Eun BL, Eun SH, Nam SO, et al. Prevalence and clinical characteristics of primary headaches among school children in South Korea: a nationwide survey. Headache 2012;52:592–9.


3. Wöber C, Holzhammer J, Zeitlhofer J, Wessely P, Wöber-Bingöl C. Trigger factors of migraine and tension-type headache: experience and knowledge of the patients. J Headache Pain 2006;7:188–95.




4. Park MN, Choi MG, You SJ. The relationship between primary headache and constipation in children and adolescents. Korean J Pediatr 2015;58:60–3.



5. Pellegrino ABW, Davis-Martin RE, Houle TT, Turner DP, Smitherman TA. Perceived triggers of primary headache disorders: a meta-analysis. Cephalalgia 2018;38:1188–98.




6. Peroutka SJ. What turns on a migraine? A systematic review of migraine precipitating factors. Curr Pain Headache Rep 2014;18:454.



7. Moschiano F, D’Amico D, Ramusino MC, Micieli G. The role of diet and lifestyle in adolescents with headache:a review. Neurol Sci 2013;34 Suppl 1:S187–90.



8. Rudolf R, Lee J. School climate, academic performance, and adolescent well-being in Korea:The roles of competition and cooperation. Child Indic Res 2023;16:917–40.


9. Jin B, Lee S, Chung US. Jeopardized mental health of children and adolescents in coronavirus disease 2019 pandemic. Clin Exp Pediatr 2022;65:322–9.




10. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1–211.


11. Yamanaka G, Morichi S, Suzuki S, Go S, Takeshita M, Kanou K, et al. A review on the triggers of pediatric migraine with the aim of improving headache education. J Clin Med 2020;9:3717.



12. Park JW, Chu MK, Kim JM, Park SG, Cho SJ. Analysis of trigger factors in episodic migraineurs using a smartphone headache diary applications. PLoS One 2016;11:e0149577.



13. Solotareff L, Cuvellier JC, Duhamel A, Vallée L, Tich SNT. Trigger factors in childhood migraine: a prospective clinic-based study from North of France. J Child Neurol 2017;32:754–8.



14. Neut D, Fily A, Cuvellier JC, Vallée L. The prevalence of triggers in paediatric migraine: a questionnaire study in 102 children and adolescents. J Headache Pain 2012;13:61–5.




15. Chakravarty A, Mukherjee A, Roy D. Trigger factors in childhood migraine:a clinic-based study from eastern India. J Headache Pain 2009;10:375–80.




16. Torres-Ferrus M, Vila-Sala C, Quintana M, Ajanovic S, Gallardo VJ, Gomez JB, et al. Headache, comorbidities and lifestyle in an adolescent population (The TEENs Study). Cephalalgia 2019;39:91–9.



17. Rystedt C. Stress in high school—a comparison between south Korea and Sweden. Int J Environ Res Public Health 2019;16:3432.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


