1. Yadav S, Lee B. Neonatal respiratory distress syndrome [updated 2023 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK560779/.
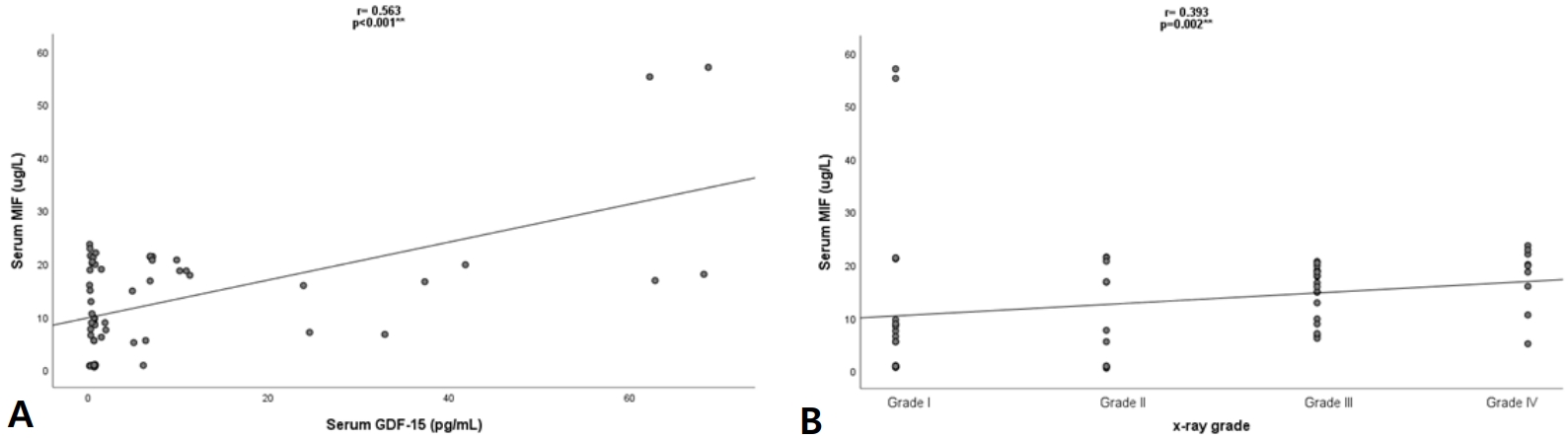
5. Abdelbaseer KA, Hassan MH, Sayed MA, Bakri AH. Role of cytokines in neonatal respiratory distress syndrome: a review article. SVU Int J Med Sci 2023;6:770ŌĆō86.

6. Paralkar V, Wistow G. Cloning the human gene for macrophage migration inhibitory factor (MIF). Genomics 1994;19:48ŌĆō51.


11. Abdelbaseer KA, Abdel mawgood EA, Hassan MH, Ibrahem MH. Role of growth differentiation factor15 in pediatric cardiac patients. SVU Int J Med Sci 2024;7:900ŌĆō10.

13. Silverman WA, Andersen DH. A controlled clinical trial of effects of water mist on obstructive respiratory signs, death rate and necropsy findings among premature infants. Pediatrics 1956;17:1ŌĆō10.

16. Moudi B, Heidari Z, Mahmoudzadeh-Sagheb H, Hashemi M. Gene polymorphisms of macrophage migration inhibitory factor affect susceptibility to chronic hepatitis B virus infection in an Iranian cohort. Microbiol Immunol 2016;60:390ŌĆō6.


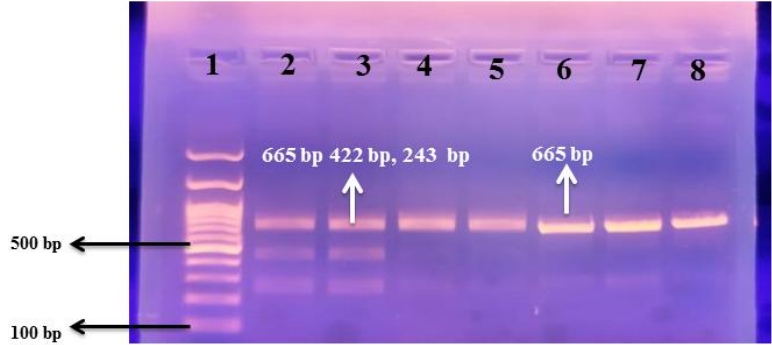
17. Atar R, Dayer D, Jalalifar M, Keikhaei B, Asadi Z. The rs4808793 polymorphism of GDF-15 associates with significantly elevated ferritin in both thalassemia major and thalassemia intermedia. Clin Cancer Investig J 2021;10:117ŌĆō21.

18. Nikitina IV, Inviyaeva EV, Krog-Jensen OA, Vtorushina VV, Lenyushkina AA, Krechetova LV, et al. Plasma cytokine level changes in preterm neonates with respiratory disorders in the early neonatal period. Akush Ginekol (Mosk) 2021;8:133ŌĆō42.

20. Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2017;3:CD004454.


21. Kong X, Xu F, Wang Z, Zhang S, Feng Z. Antenatal corticosteroids administration on mortality and morbidity in premature twins born at 25~34 gestational weeks: a retrospective multicenter study. Eur J Obstet Gynecol Reprod Biol 2020;253:259ŌĆō65.


23. Aslamzai M, Froogh BA, Mukhlis AH, Faizi OA, Sajid SA, Hakimi Z. Factors associated with respiratory distress syndrome in preterm neonates admitted to a tertiary hospital in Kabul city: a retrospective cross-sectional study. Glob Pediatr 2023;3:100035.

24. Abilbayeva A, Tarabayeva A, Bozhbanbayeva N, Yelyubayeva D. Risk factors for mortality in low birth weight infants with respiratory distress syndrome. J Clin Med Kaz 2024;21:79ŌĆō84.

26. Shashidhar A, PN SR, Jose J. Downes score vs. Silverman Anderson score for assessment of respiratory distress in preterm newborns. Pediatr Oncall J 2016;13:66ŌĆō8.
27. Silveira Neves G, Silveira Nogueira Reis Z, Maia de Castro Romanelli R, Dos Santos Nascimento J, Dias Sanglard A, Batchelor J. The role of chest X-ray in the diagnosis of neonatal respiratory distress syndrome: a systematic review concerning low-resource birth scenarios. Glob Health Action 2024;17:2338633.


28. Tigabu Kebede Z, Matebe YH, Demisse AG, Yimer MA, Mekasha A, Worku A, et al. Hematologic profiles of Ethiopian preterm infants with clinical diagnoses of early-onset sepsis, perinatal asphyxia, and respiratory distress syndrome. Glob Pediatr Health 2020;7:2333794X20960264.


29. Marseglia L, D'Angelo G, Granese R, Falsaperla R, Reiter RJ, Corsello G, et al. Role of oxidative stress in neonatal respiratory distress syndrome. Free Radic Biol Med 2019;142:132ŌĆō7.


31. Abdelrashid S, Aref M. Platelet indices as a predictive marker in neonates with respiratory distress. Egypt Pediatr Assoc Gaz 2024;72:21.


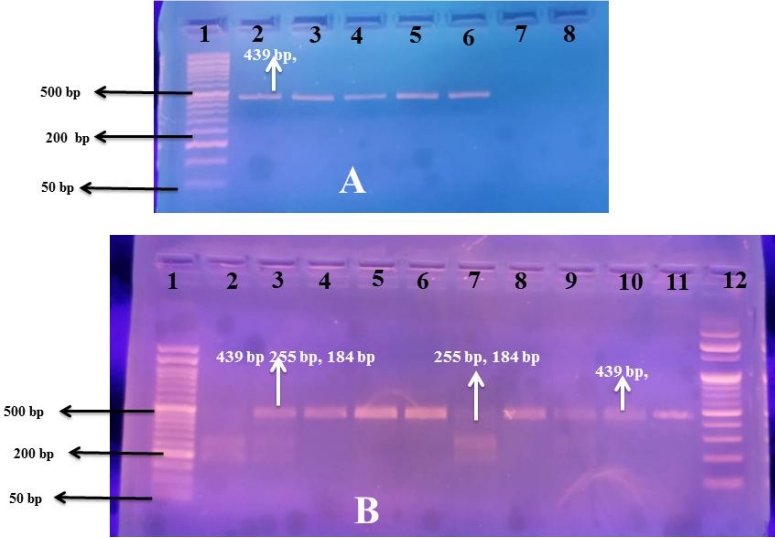
33. Mohany KM, Sayed AA, El-Asheer OM, Raheem YF, Abbas AM, Fawzy AM, et al. The association of LPCAT1-rs9728 polymorphism with cord blood IL-10, MIF, and VEGF levels in neonatal respiratory distress syndrome: a case-control study. Egypt J Bronchol 2024;18:25.


38. Zhang X, Wang R, Zhang X, Yang Y, Tian R. Ferroptosis related CPT1A and GDF-15 gene polymorphisms are risk factors for lung adenocarcinoma: a case-control study. Gene 2025;933:149002.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


