Article Contents
| Clin Exp Pediatr > Volume 68(10); 2025 |
|
Abstract
Background
Asthma severity is influenced by various immunomodulators; however, the specific roles of thyroid hormones and endothelin in childhood asthma in the South Indian population remain unexplored.
Purpose
This study investigated the impact of thyroid hormone and endothelin levels on asthma control among children in South India.
Methods
We divided 90 subjects aged 10–15 years into 3 groups as categorized by the Global Initiative for Asthma guidelines: 30 healthy children, 30 patients with well-controlled asthma, and 30 patients with poorly controlled asthma. Fasting blood samples were collected to analyze endothelin levels and thyroid function. Pulmonary function tests were performed using a portable spirometer to assess forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and the FEV1/FVC ratio.
Results
Thyroid-stimulating hormone (TSH) levels were significantly elevated in the well-controlled (4.66±1.91 mIU/L) and poorly controlled (6.51±4.04 mIU/L) asthma groups versus the control group (P<0.001). Similarly, endothelin levels showed a marked increase (4.65±0.38 pg/mL vs. 18.51±6.13 pg/mL), with the poorly controlled group exhibiting the highest levels (P<0.001). A strong negative correlation was observed between FEV1/FVC% and serum endothelin levels (r=-0.76) on a Pearson correlation analysis.
Asthma, a chronic lung disease characterized by bronchial inflammation, has emerged as a significant public health concern globally, affecting approximately 300 million individuals worldwide. In India alone, 35 million people suffer from asthma, posing substantial challenges in lung care, particularly among school children, where it can impact education and quality of life [1]. Research has elucidated complex mechanisms underlying asthma, yet further investigation is necessary to mitigate associated complications. Notably, evidence suggests that effective asthma management is intricately linked to non-respiratory comorbidities, such as hormonal homeostasis, specifically the pituitary-thyroid axis. Both asthma and thyroid dysregulation share common lung inflammation and immunological pathways [2]. Moreover, corticosteroid-based asthma treatments can influence thyroid hormone synthesis and metabolism, highlighting the importance of considering the interplay between asthma and thyroid function in clinical management.
Beyond hormonal influences, endothelin-1 (ET-1), a potent vasoconstrictor produced by various cells, has been identified as a predictor of several morbidities, including stroke and cardiovascular diseases (CVDs) [3]. Notably, elevated endothelin levels have been linked to increased airway obstruction and asthma severity, suggesting its potential as a biomarker for disease progression [4]. Although studies have investigated the role of thyroidstimulating hormone (TSH) status in adult asthma populations, data on pediatric populations, particularly in South India, remain scarce [5]. Furthermore, the relationship between serum endothelin levels and TSH levels in children is largely unexplored. This study aims to address this knowledge gap by comparing and associating serum levels of endothelin and thyroid hormones in children with and without asthma, focusing on the pediatric South Indian population over a period of 2 years.
This cross-sectional study was conducted by the Department of Biochemistry in collaboration with the Department of Paediatrics at a tertiary care hospital, following approval from the Institutional Research and Ethics Committees. A total of 60 pediatric asthma patients, aged 10–15 years, were enrolled over a period of 2 years. At the time of diagnosis, all participants were on some form of maintenance therapy but had a history of irregular treatment adherence.
Patients were classified into 2 groups based on their Asthma Control Test (ACT) scores: well-controlled asthma (ACT score 20–25, n=30), and poorly controlled asthma (ACT score 5–15, n=30). The ACT is a standardized questionnaire assessing asthma symptoms, reliever medication use, and the patient’s self-assessed control over the past 4 weeks. An ACT score of 16–19 indicates not well-controlled asthma, but for this study, only patients with scores in the well-controlled and poorly controlled categories were included. Partly controlled asthma patients representing an intermediate and heterogeneous group were excluded to avoid overlapping categories.
Study participants were stratified with reference to thyroid function. Those with TSH between 0.4 and 4.0 mU/L and free T4 between 0.8 and 1.8 ng/dL were classified as euthyroid. Subjects exhibiting subclinical hypothyroidism were defined by a mildly elevated TSH (5.0–10.0 mU/L) in conjunction with normal free T4 (0.8–1.8 ng/dL) and total T4 (5.0–12.0 μg/dL) levels. Overt hypothyroidism was diagnosed in participants with TSH exceeding 10.0 mU/L and reduced free T4 (<0.8 ng/dL) and total T4 (<5.0 μg/dL) [6]. Subjects with other lung diseases (bronchiectasis, emphysema, infective bronchitis) and Chronic illnesses (hypertension, diabetes, renal failure, cyanotic heart diseases, known thyroid disorders and other endocrine disorders) were excluded. Thirty age- and sex-matched healthy individuals served as controls. Written informed consent was obtained from parents/guardians. Waist and hip circumference were measured using standardized measuring tape and waist-hip ratio (WHR) was calculated from the measured values. Body mass index (BMI) was calculated using the formula (weight in kg/height in m2). Pulmonary function test was performed by a trained technician in the pulmonology department who was experienced in spirometry and handling pediatric subjects. The study subjects were seated with a nose clip in place. To ensure reproducibility the test was repeated 3 times and the best of the 3 were taken. Pulmonary function tests were measured using a portable spirometer (MIR Winspiro Spirobank II), assessing forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio. MIR Winspiro Spirobank II spirometer uses an integrated Global Lung Initiative 2012 reference equation for calculating the predictive values of FEV1, FVC and FEV1/FVC ratio [7]. This equation takes into account the age, sex, height and ethnicity of the study participants. The spirometer automatically calculated z scores and percent predicted values and this was used to categorize patients based on standardized cutoff. Under aseptic precautions, 2 mL of blood sample was collected. The levels of serum ET-1 were determined using a specific and sensitive commercially available enzyme-linked immunosorbent assay according to manufacturer’s instructions (Bioassay Technology Laboratory, China) systems and thyroid hormones were measured using Chemiluminescence. The data was expressed as mean±standard deviation. One-way analysis of variance was used to compare the study parameters. Pearson correlation analysis evaluated relationships between pulmonary function tests, endothelin levels, and thyroid function tests. IBM SPSS Statistics ver. 20.0 (IBM Co., USA) was used for analysis, and a P value <0.05 was considered statistically significant.
The mean age of the study population was 13.79±1.65 years. Asthma subjects had higher BMI and higher WHR compared to non-asthmatic controls (Table 1). Poorly controlled asthma subjects showed significant reductions in pulmonary function (FEV1, FVC, FEV1/FVC ratio). Serum endothelin levels were significantly higher in poorly controlled asthma patients (P<0.001). Poorly controlled asthma patients had significantly increased TSH levels and decreased T4 levels (P<0.001) compared to well-controlled and healthy subjects. Furthermore, the serum T3 level does not show any significant results among the study subjects. Furthermore, asthma control and thyroid hormone status showed a significant positive association. The prevalence of euthyroid status decreased from 96.67% in controls to 66.67% in poorly controlled asthma patients. Conversely, subclinical hypothyroidism increased from 3.33% in controls to 20% in poorly controlled asthma patients, and overt hypothyroidism rose from 0% to 13.33% (Table 2).
Endothelin levels exhibited a significant negative correlation with pulmonary function indices, including FEV1% (r=-0.83), FVC% (r=-0.82), and FEV1/FVC (r=-0.79) (Fig. 1). Similarly, TSH levels showed a strong negative correlation with FEV1% (r=-0.51), FVC% (r=-0.41), and FEV1/FVC (r=-0.56) (Fig. 2) Additionally, TSH levels showed a strong positive association with endothelin levels (r=0.41), while endothelin levels were significantly negatively correlated with T4 levels (r=-0.56).
Receiver operating characteristic analysis of serum ET-1 in asthma control demonstrated an optimal cutoff of 6.7 pg/mL, achieving an area under the curve of 0.98 for excellent diagnostic accuracy; at this threshold, sensitivity reached 97% and specificity was 87%, (Fig. 3) indicating strong potential for ET 1 as a clinical biomarker to distinguish well controlled from poorly controlled asthma. These findings suggest a potential interplay between endothelin-mediated vascular or systemic effects and thyroid function, which may collectively influence pulmonary performance.
There are increased endothelin levels and increased risk of hypothyroidism in poorly controlled asthma than well-controlled asthma in the pediatric population. Asthma is a multifaceted disorder encompassing diverse endotypes and phenotypes. Notably, childhood asthma differs significantly from adult-onset asthma in terms of triggers and inflammatory pathways. This study examined the serum levels of endothelin and thyroid hormones in children with and without asthma and on the association of endothelin levels and thyroid focusing on the pediatric South Indian population. Early identification and intervention can potentially mitigate morbidity and mortality associated with cardiovascular complications [7,8].
Asthma, characterized by hyperresponsive lung inflammation, can lead to chronic hypoxia, potentially triggering a cascade of biochemical changes that increase the risk of future complications which often remain under-evaluated. The consequences are alarming, as CVD is the leading cause of death worldwide. In India, asthma management is suboptimal, with 82% of patients with early symptoms and 70% with severe asthma receiving inadequate care due to various factors, including variable symptom presentation, healthcare provider workload, and limited resources, particularly in primary healthcare settings. Furthermore, access to diagnostic spirometry, the gold standard for asthma diagnosis, is often impractical in resource-constrained settings, exacerbating the issue [9,10].
Thyroid hormones profoundly impact metabolism and cardiovascular function, influencing cardiac contractility and electrical activity. Alterations in thyroid hormone levels can lead to significant cardiovascular complications. Our study revealed a substantial proportion of asthma patients with subclinical and overt hypothyroidism, exhibiting a negative correlation with lung function tests. This aligns with existing research indicating a link between asthma and increased hypothyroidism risk [2]. A study done by Eliseeva et al. [11] in 51 children showed subclinical hypothyroidism was prevalent in bronchial asthma. Liu et al. [12] found that maternal hypothyroidism may increase the risk of asthma in children. Sundaram et alet al. [13] reported that hyperthyroidism complicates asthma treatment. Notably, our study found no cases of hyperthyroidism, contrasting with the findings of Sundaram et al. [13] Kim [14] developed a predictive model for the development of childhood asthma as a valuable tool for clinical diagnosis of disease.
Altered thyroid hormone sensitivity impairs pulmonary function, affecting respiratory muscles, membrane fluidity, and neurochemical transmission. This disruption may compromise immunological function through chronic inflammation, oxidative stress, and metabolic dysregulation, as thyroid hormones regulate key enzymes [15].
The pathogenesis of asthma and hypothyroidism involves complex immune mechanisms. While asthma is typically associated with Th2-mediated inflammation, recent research has identified non-Th2 asthma subtypes involving alternative pathways. Key immune cells implicated in asthma development include Th1 cells and Th17 cells which contribute to hypothyroidism pathogenesis through inflammatory pathways. Notably, non-Th2 asthma subtypes have emerged, highlighting diverse immunological mechanisms beyond traditional Th2-mediated responses [16].
ET-1, is a potent vasoconstrictor and broncho constrictor with diverse physiological and pathological roles. ET-1 is a peptide produced by various cells, including endothelial cells, vascular smooth-muscle cells, and bronchial epithelial cells. Notably, bronchial epithelial cells from asthmatic patients exhibit increased ET-1 expression. Elevated ET-1 levels have been detected in the airways of asthmatic individuals, where it contributes to several pathological processes, including stimulating mucus secretion and airway edema, promoting smooth-muscle cell growth (mitogenesis) and enhancing bronchial hyper-responsiveness. Furthermore, ET-1 is believed to exert proinflammatory effects in the airways by acting as a chemoattractant and upregulating other inflammatory mediator, such as interleukins IL-6 and IL-8. Recent research has highlighted its contribution to disease, leading to the development of endothelin receptor antagonists for therapeutic use [17].
Endothelin drives tissue remodeling by promoting extracellular matrix synthesis, myofibroblast differentiation, and mesenchymal cell proliferation. They also contribute to asthma-induced cardiac remodeling [18]. Endothelin exhibits differential effects on alveolar macrophages contingent upon disease severity [19]. Serum ET-1 levels in adult asthmatics are normal in between attacks, but they are high during acute attacks. These elevated levels are inversely correlated with airflow measurements and decrease with treatment. The FEV1/FVC ratio and plasma ET-1 levels were shown to be significantly correlated negatively (P<0.01). These findings imply that the degree of acute asthma may be reflected in circulating ET-1 levels [20]. In our study, we used serum endothelin for differentiating well-controlled and poorly controlled in comparison with healthy control with the optimum cuff of 6.7 pg/mL with sensitivity of 97% and specificity of 87%. Our results corroborate Aoki T's earlier findings, demonstrating endothelin's involvement in asthma severity however endothelin receptor antagonists fail to exhibit substantial therapeutic benefits, warranting further investigation [21]. Also, El-Gamal et al. [22] reported increased plasma ET-1 in children during asthmatic episodes. Moreover, in our study, there was a significant association between serum endothelin levels, pulmonary function test and TSH levels. Hence, this finding could provide novel insight into the biochemical mechanisms and their interplay with TSH. Higher endothelin concentrations in pediatric asthma patients are associated with lower lung function. Increased inflammation or airway blockage may be indicated by elevated ET-1, a strong vasoconstrictor and fibrosis mediator. These results point to ET-1 as a possible biomarker for evaluating the deterioration of lung function in asthmatic patients. Research has indicated that ET-1 plays a part in the pathophysiology of bronchoconstriction since it is substantially elevated in children with asthma during acute episodes as opposed to remission periods and healthy controls [23].
A study done by Voelkel and Tuder24) in 2000 states that hypoxia increases ET-1 levels through 2 mechanisms which included enhanced ET-1 gene expression via transcription factors like activator protein-1 and increased activity of endothelin-converting enzymes. Despite this finding, clinical validation on the use of serum endothelin as a novel marker in disease stratification, and pharmacological response and on the pulmonary function decline in asthma may be noteworthy. A few limitations of our study include the lack of assessment of treatment history, duration, smaller sample size, excluding partially controlled asthma patients, and heterogeneous population. Although age and gender matching aimed to reduce confounding, it may not fully eliminate selection bias and, given the small sample size (n=30 per group), could further limit generalizability. These issues could be addressed in future research.
In conclusion, the study revealed a strong association between endothelin levels, FEV1/FVC ratios, and TSH levels. These findings suggest that serum endothelin could serve as a potential surrogate marker for assessing asthma severity.
Footnotes
Fig. 1.
Correlation between pulmonary function and serum endothelin levels in pediatric asthma. (A) Increased endothelin levels were associated with a lower FVC%. (B) A significant inverse correlation was observed between FEV1/FVC ratio and serum endothelin. (C) Inverse correlation between serum endothelin and FEV1%. This pattern suggests that ET-1 may contribute to airway inflammation, bronchoconstriction, and remodeling, leading to measurable declines in lung function. ET-1 is a potent vasoconstrictor and proinflammatory mediator, as shown by the observed physiological impairment in these children with asthma [22]. ET-1, endothelin-1; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.

Fig. 2.
Correlation between thyroid hormone and pulmonary function test results in pediatric patients with asthma. (A) A weak inverse correlation was observed between FVC and TSH, suggesting that higher TSH levels may be modestly associated with reduced lung function. (B) An inverse relationship between FEV1/FVC ratio and TSH levels in pediatric patients with asthma. (C) A significant inverse correlation was observed as FEV1% decreased. Elevated TSH, often indicative of subclinical or overt hypothyroidism, appeared to be correlated with worsening pulmonary function in children with asthma, potentially due to its effects on respiratory muscle strength, airway inflammation, or systemic metabolism [15]. FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; TSH, thyroid-stimulating hormone.

Fig. 3.
Receiver operating characteristic (ROC) analysis showing the diagnostic accuracy of endothelin-1 (ET-1) at distinguishing between well-controlled and poorly controlled asthma. A serum ET-1 level of 6.7 pg/mL (area under the curve, 0.98) effectively differentiated between subjects with well-controlled and poorly controlled asthma with high sensitivity (97%) and specificity (87%). These findings suggest that ET-1 level could offer meaningful support for assessing asthma control status and potentially enhance clinical decision-making in pediatric asthma management [11,16].
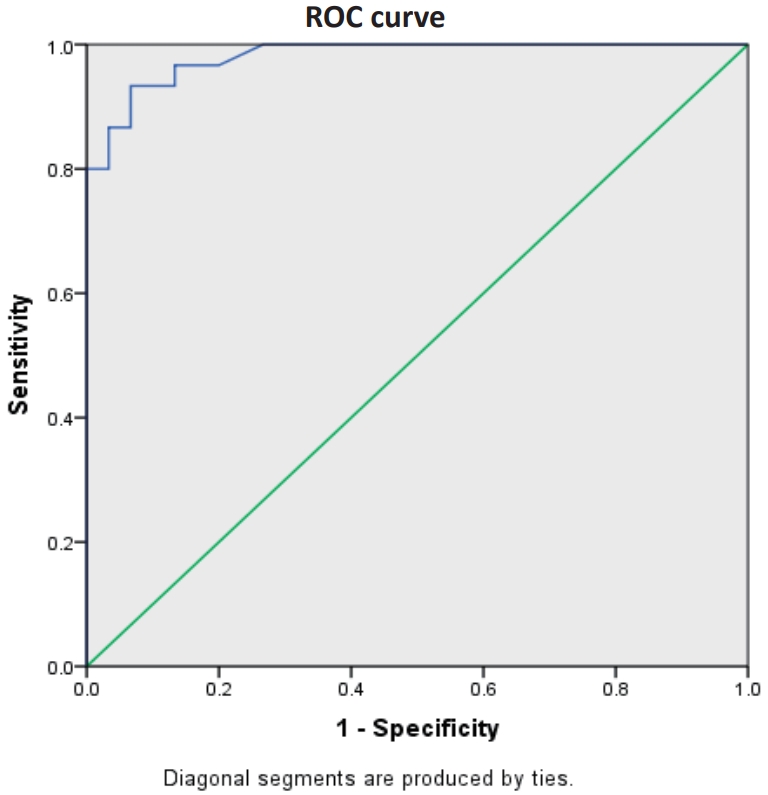
Table 1.
General characteristics, lung function, and biochemical evaluation results, and medications of patients with well- or poorly controlled asthma versus healthy controls
Values are presented as mean±standard deviation.
BMI, body mass index; WHR, waist-to-hip ratio; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; TSH, thyroid-stimulating hormone; T3, triiodothyronine; T4, tetraiodothyronine.
Boldface indicates a statistically significant difference with P<0.05.
Table 2.
Thyroid status by study group
References
2. Huang SC, Gau SY, Huang JY, Wu WJ, Wei JC. Increased risk of hypothyroidism in people with asthma: Evidence from a real-world population-based study. J Clin Med 2022;11:2776.



3. Torres Crigna A, Link B, Samec M, Giordano FA, Kubatka P, Golubnitschaja O. Endothelin-1 axes in the framework of predictive, preventive and personalised (3P) medicine. EPMA J 2021;12:265–305.




4. Spiropoulos K, Trakada G, Nikolaou E, Prodromakis E, Efremidis G, Pouli A, et al. Endothelin-1 levels in the pathophysiology of chronic obstructive pulmonary disease and bronchial asthma. Respir Med 2003;97:983–9.


5. Bingyan Z, Dong W. Impact of thyroid hormones on asthma in older adults. J Int Med Res 2019;47:4114–25.




6. Khandelwal D, Tandon N. Overt and subclinical hypothyroidism: who to treat and how. Drugs 2012;72:17–33.


7. Cooper BG, Stocks J, Hall GL, Culver B, Steenbruggen I, Carter KW, et al. The Global Lung Function Initiative (GLI) network: bringing the world’s respiratory reference values together. Breathe (Sheff) 2017;13:e56–64.



8. Daniels SR. Cardiovascular disease risk factors and atherosclerosis in children and adolescents. Curr Atheroscler Rep 2001;3:479–85.



9. Hekking PP, Bel EH. Developing and emerging clinical asthma phenotypes. J Allergy Clin Immunol Pract 2014;2:671. –80. quiz 681.


10. Swarnakar R, Dhar R. Call to action: addressing asthma diagnosis and treatment gaps in India. Lung India 2024;41:209–16.



11. Eliseeva T, Tush E, Bolshova E, Prachov A, Polyakova V, Balabolkin I, et al. P17 Thyroid status in children with bronchial asthma (BA). Arch Dis Child 2019;104:A162.

12. Liu X, Andersen SL, Olsen J, Agerbo E, Schlünssen V, Dharmage SC, et al. Maternal hypothyroidism in the perinatal period and childhood asthma in the offspring. Allergy 2018;73:932–9.



13. P S, K G, Jm J. Thyroid disease and asthma. Lung India 1998;16:83.
14. Kim BS. Is the predictive model for asthma development useful as a tool for diagnosing pediatric asthma? Clin Exp Pediatr 2020;63:102–3.




16. Wang Z, Lu B, Wu M, Gu T, Xu M, Tang F, et al. Reduced sensitivity to thyroid hormones is associated with lung function in euthyroid individuals. Heliyon 2024;10:e30309.



18. Nakas-Icindic E, Zaciragic A, Hadzovic A, Avdagic N. Endothelin in health and disease. Bosn J Basic Med Sci 2004;4:31–4.




19. Chanez P, Vignola AM, Albat B, Springall DR, Polak JM, Godard P, et al. Involvement of endothelin in mononuclear phagocyte inflammation in asthma. J Allergy Clin Immunol 1996;98:412–20.


20. Sato H, Nagano T, Suraya R, Hazama D, Umezawa K, Katsurada N, et al. Reduction in circulating endothelin-1 levels by inhaled COPD medications. Respir Med 2025;240:108027.


21. Aoki T, Kojima T, Ono A, Unishi G, Yoshijima S, Kameda- Hayashi N, et al. Circulating endothelin-1 levels in patients with bronchial asthma. Ann Allergy 1994;73:365–9.

22. El-Gamal Y, Hossny E, Awwad K, Mabrouk R, Boseila N. Plasma endothelin-1 immunoreactivity in asthmatic children. Ann Allergy Asthma Immunol 2002;88:370–3.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


