Article Contents
| Clin Exp Pediatr > Volume 55(7); 2012 |
Abstract
Purpose
With feasibility in the diagnoses of congenital heart disease (CHD) in the antenatal period, we suspect changes have occurred in its incidence. No data have been reported about the current incidence of simple forms of CHD in Korea. We have attempted to assess the recent incidence and characteristics of CHD in the neonatal care unit of a secondary referral medical center.
Methods
Medical records of 497 neonatal care unit patients who underwent echocardiography in the past 5 years were reviewed. Pre-term infants with patent ductus arteriosus and other transient, minimal lesions were excluded from this study.
Results
Although the number of inpatients remained stable, the incidence of simple forms of CHD showed a gradual decrease over the 5-year study period; a markedly low incidence of complex forms was seen as well. CHD was observed in 3.7% full-term and 6.8% pre-term infants. CHD was observed in 152 infants weighing >2,500 g (3.5% of corresponding birth weight infants); 65 weighing 1,000 to 2,500 g (9.3%); and 6 weighing <1,000 g (8.0%). The incidence of CHD was higher in the pre-term group and the low birth weight group than in each corresponding subgroup (P<0.001); however, the incidence of complex CHD in full-term neonates was high. The number of patients with extracardiac structural anomalies has also shown a gradual decrease every year for the past 5 years.
Congenital heart disease (CHD) is a common cause of perinatal morbidity and mortality and many of cases are associated with extracardiac anomalies1-4). With the feasibility of fetal echocardiography, remarkable changes have occurred in the incidence of hemodynamically significant CHD. Antenatal imaging studies have improved the care and outcome for selected fetuses with severe cardiac malformations. A few studies have reported on the impact of fetal echocardiography with regard to the incidence of significant or complex CHD5-7). Usually, cases with severe structural cardiac anomaly could be detected relatively easily on fetal echocardiography and patients could be referred to the tertiary center before delivery, by which the CHD pattern in secondary and tertiary medical referral centers might have changed8). However, cases with minor defects might be neglected on fetal imaging study and the incidence of non-complex CHD is expected not to have changed. However, few population-based reports on recent incidence of CHD focused on simple CHD have been published. The incidence of simple forms of CHD at secondary referral medical centers might be more valuable because patients with these lesions rarely transfer to tertiary centers during the fetal period.
We attempted to assess the recent incidence and trends of CHD at a single neonatal care unit of the secondary referral medical center in Korea.
Retrospective analysis of the medical records of a 5-year period (January 2004 to December 2008) was performed in a neonatal intensive care unit (NICU) and nursery unit (NU) of St. Vincent's Hospital, which is a secondary referral medical center in Korea. The number of patients admitted to the NICU and NU during the five-year period was 5,127. A total of 497 patients (243 males, 254 females) underwent echocardiography for various reasons. Excluding cases with patent ductus arteriosus (PDA) in prematurity, patent foramen ovale (PFO) and small secondum atrial septal defect (ASD) (Ōēż3 mm), and minimal peripheral pulmonic stenosis (PS) (peak flow velocityŌēż2.0 m/sec), a total of 223 patients (4.3% of total inpatients) diagnosed with CHD was included as subjects in this study (103 males and 120 females) (Table 1). Among these patients with CHD, 122 patients (54.5%) were born at our institution and 101 patients (45.4%) were born at local clinics and transferred to our institution with various symptoms and signs. Whereas most of all the inborn patients underwent antenatal sonography of which 3 patients were diagnosed with complex CHD antenatally on the fetal echocardiography, it was hard to get detailed information on the antenatal care at local primary obstetrical clinics and all of them were diagnosed with CHD postnatally. Median age of patients at admission was 1 day after birth (ranging from the first day of life to 29 days) and median birth weight was 2,860 g (810 to 5,700 g); median gestational age was 38 weeks (27+4 to 41+4 weeks). The male to female ratio of patients with CHD (n=223) was 0.83:1 and the reasons for admission included prematurity care, respiratory distress syndrome, necrotizing enterocolitis, apnea, and others in 70 pre-term patients, and murmur, hyperbilirubinemia, transient tachypnea of the newborn, meconium aspiration, sepsis, gastroenteritis, and others in 153 full-term babies.
In this study, all the patients included were infants only that are younger than 1 month after birth and we regarded the lesion of CHD as an simple one if the lesion has left to right shunt that does not cause cyanosis such as ASD, ventricular septal defect (VSD), PDA or an non-critical obstructive lesion such as mild to moderate PS. On the contrary, a lesion that has severe morphologic abnormality and leads to cyanosis was regarded as an complex CHD such as hypoplastic left heart syndrome (HLHS), transposition of great arteries (TGA), double outlet of right ventricle (DORV), etc. In order to avoid double counts, cases with multiple types of lesions were categorized into one disease that is hemodynamically the most important.
Data between each group were compared using the chi-square test (SPSS ver. 12.0 [SPSS Inc., Chicago, IL, USA]) and a P value of less than 0.05 was considered statistically significant.
While the total numbers of patients in the NICU and NU were constant, total numbers of neonates with CHD, cases with ASD, VSD, and PS showed a gradual decrease during the study period (Fig. 1). In 2004, the proportion of patients with total CHD among patients in the NICU and NU of that year was 6.0% (67 cases out of 1,125 patients), but 2.8% (27/974) in 2008. On the other hand, the numbers of patients admitted to the NICU and NU for 5 years were relatively constant, approximately 1,000 patients each year (1,125 patients in 2004, 950 in 2005, 1,022 in 2006, 1,056 in 2007, and 974 in 2008).
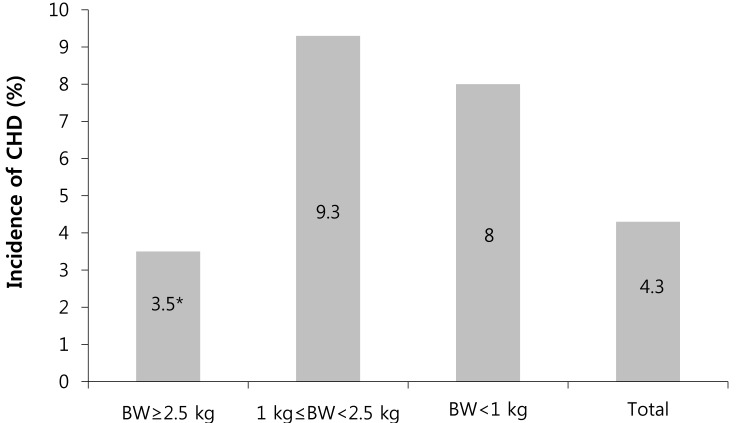
For comparisons of subgroups of patients diagnosed with CHD, we speculated on the total number of patients according to gestational age, birth weight, and other clinical characteristics. Among the 1,022 premature infants with gestational age less than 37 weeks, 70 cases (6.8%) had CHD, whereas among the 4,105 full-term patients, 153 cases (3.7%) had CHD. In accordance with the proportion of each group, total incidence of CHD was higher in pre-term patients (P<0.001) (Fig. 2).
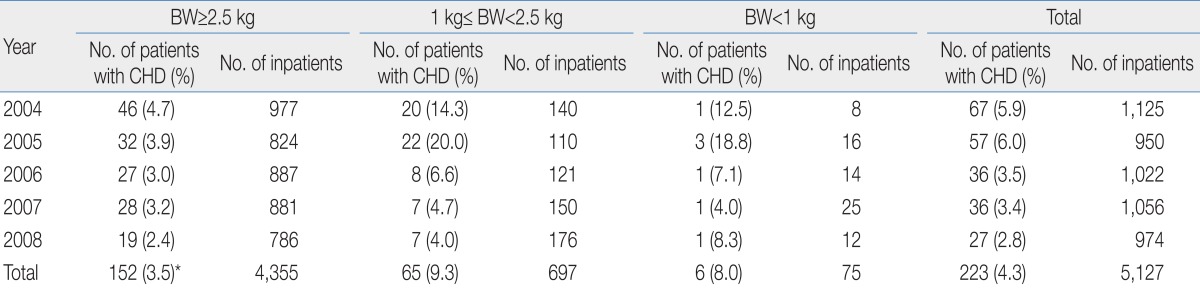
When patients were categorized according to their birth weight (Ōēź2,500 g, 1,000 to 2,500 g, <1,000 g), the incidence of CHD was highest in the subgroup of birth weight 1,000 to 2,500 g, (9.3%) (P<0.001, compared with the other two groups) (Fig. 3). In the subgroup of 75 patients with birth weight <1,000 g, 6 patients (8%) had CHD. Hence, the incidence of CHD was higher in low birth weight groups than in non-low birth weight groups (Table 2).
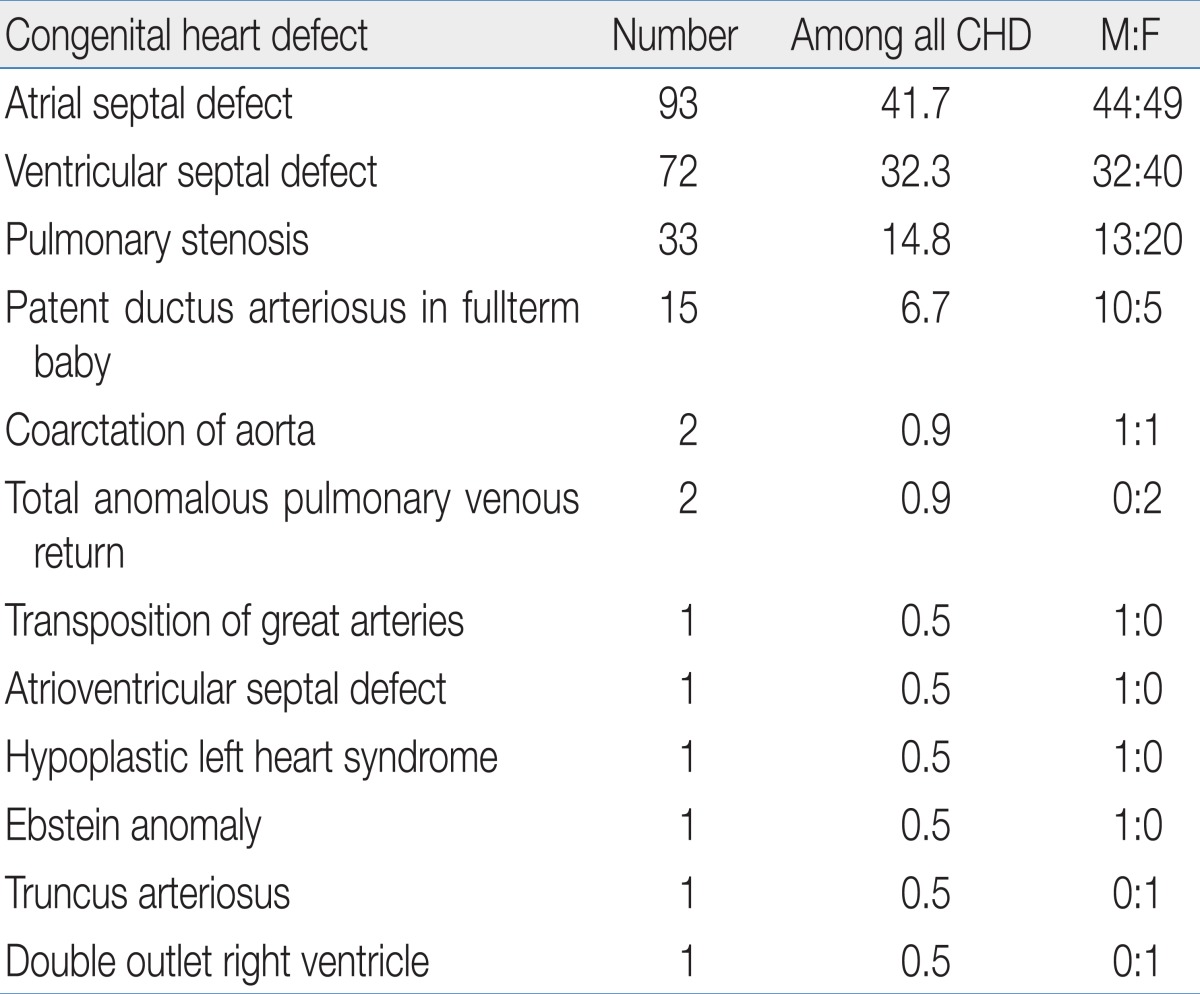
Diagnoses of CHD were as follows: ASD (n=93, 41.7%), VSD (n=72, 32.3%), and PS (n=33, 14.8%). There were two cases each of coarctation of aorta (CoA) and total anomalous pulmonary venous return (TAPVR). One patient with TAPVR revealed the abnormal drainage was supracardiac type and the other infracardiac type. There was one case each of TGA, atrioventricular septal defect (AVSD), HLHS, Ebstein anomaly, truncus arteriosus (TA), and DORV (Table 3). Incidence of complex CHD was higher in full-term neonates (n=8, 80%) (Table 4).
Because the patients included in this study were patients in the NICU or NU, the majority (40%) of cases with CHD in this study were initially diagnosed within 5 days after birth. Numbers of cases according to age at initial diagnosis after birth (days) were as follows; 90 (40%) within 5 days, 40 (18%) on 6 to 10 days, 25 (11%) on 11 to 15 days, 16 (8%) on 16 to 20 days and 52 (23%) later than 20 days after birth. Most patients who underwent study with echocardiography at their very early age after birth, underwent double checking echocardiography before discharge.
Regarding the prognosis of the patients, among the population of 70 premature baby with CHD, there were 3 fatal cases; one with severe hydrops fetalis and Ebstein anomaly, the other one who was severely small for gestational age with VSD and Edward syndrome, and another one with sepsis who had ASD. One case was transferred for cardiac surgery with d-TGA on the first day after birth. Among the population of 153 full-term babies with CHD, there were 3 fatal cases; one with HLHS, the other with severe persistent pulmonary hypertension of the newborn who had ASD, and another one with sepsis who had CoA. Seven patients of full-term baby group transferred to cardiac centers with severe PS, TAPVR, AVSD, DORV, TGA, TA and CoA, and three other patients transferred to tertiary referral centers with extracardiac problems.
The most common symptom leading to study with echocardiography was cardiac murmur. Other symptoms included tachypnea and cyanosis after birth (Fig. 4). Out of 223 neonates with CHD, five patients were syndromatic. Three neonates had Edward syndrome and the other two had Down syndrome and Turner syndrome each.
We also checked the extracardiac structural anomaly that could be feasible for antenatal detection and the numbers of cases each year were as follows: 25 cases in 2004, 25 in 2005, 10 in 2006, 10 in 2007, and 7 in 2008. In particular, the numbers of cases with anomaly of the digits and cleft palates showed a gradual decrease (Data are not shown here).
An altered pattern of CHD in tertiary NICUs in Korea has recently been reported, with 68.4% of patients prenatally diagnosed with CHD and 78.0% with significant complex CHD6). Recent incidence of CHD in Korea was reported as 2.4 to 3.8/1,000 live births and up to 70.7% of CHD was reported as benign and complex heart anomalies were extremely rare9). Our data showed more than 90% of CHD were simple forms. With regarding these findings, we attempted to determine recent trends of simple forms of CHD among patients of the NICU and NU in the fetal echocardiographic era in Korea, not nationwide population based incidence of simple CHD. It is known that the incidence of CHD shows remarkable variation according to ethnicity and inclusion criteria of minor defects, mostly depending on the numbers of small muscular VSD10). For this reason, in epidemiologic study, rigorous inclusion criteria for each study are mandatory. In this study, as we studied incidence of CHD in sick patients admitted to the NICU, even after exclusion of cases with PDA in prematurity, PFO, and mild peripheral PS, the total number of patients with CHD was 223 (4.3%), which was much higher than the previously reported incidence of 5 to 8 /1,000 live births in the general population as expected.
Our findings of a gradual decrease in numbers of simple CHD might be combined with decreased numbers of extracardiac congenital anomaly or chromosomal abnormality, or owing to the trend of transferring pregnant mothers with high risk pregnancy to tertiary medical centers. However, minor defects are usually not regarded as problematic or are not even detected before delivery and the incidence of complex cardiac anomaly has originally been low; our data imply that minor cardiac defects, as well as complex CHD lesions, might also have been decreased. Gradual decrease of numbers of extracardiac anomaly, including digits and cleft palates, may indirectly implicate that structural anomaly might have been aborted in the early stage of gestation. A recent report on termination rates in Korea revealed that pregnancy termination rates have remained unchanged, whereas mortality of CHD patients has continued to decline11).
Similar phenomena have been reported in several countries. A recent epidemiologic study in Taiwan revealed a downward trend, not only in severe forms of CHD, but also in simple forms of CHD; however, the reasons for this trend are unclear12). Yang et al.13) revealed that use of fetal echocardiography resulted in significantly reduced incidence of live-born CHD in Beijing, China. Khoshnood et al.14) observed that decreases in perinatal mortality might have been related in part to increases in pregnancy termination for severe cases of CHD in Paris.
Our observation shows that the overall incidence of CHD was higher in the low birth weight group and pre-term babies. Reasons for the higher incidence of CHD observed in premature infants and in the low birth weight group remain unclear. Malik et al.15) reported that infants with congenital heart defects are approximately twice as likely to be small for their gestational age as control subjects. Godfrey et al.16) reported increased incidence of CHD in very low birth weight infants, as compared with the general population. Tanner et al.17) reported that pre-term infants have more than twice as many cardiovascular malformations as do infants born at term. Remarkably, outcome of pre-term infants with CHD was significantly worse than that for full-term infants18,19).
That the incidence of complex CHD was higher in full-term neonates (n=8, 80%) in our study is quite interesting. Several studies have reported higher incidence of CHD in premature or low birth weight groups; however, we could find no reports showing that complex or ductal-dependent cardiac lesions are frequently found in full-term patients, compared with premature babies. Further study regarding this point with a larger patient population is needed.
Unlike previous studies20-25), ASD accounted for the highest percentage, followed by VSD, and PS in order. This result is probably due to the fact that subjects of this study were all neonates. Usually the incidence of CHD varies depending whether premature babies are included into the subjects or not. Hoffman and Kaplan10) determined that the reasons for variability of the incidence of CHD and relative frequency of different major forms of CHD from study to study is dependent upon how early the diagnosis is made. If tiny muscular VSD present at birth and other trivial lesions were included, the incidence was increased. Regarding the timing of initial echocardiographic study on the patients included here, most of the patients were evaluated cardiac problem at their very early age after birth. As one third of the patients diagnosed with CHD was pre-term babies among which one third of pre-term babies were extremely low birth weight infants, and most of them were examined with echocardiography before their 40 weeks of gestational age, hence, the results may differed from the incidence of CHD of older pediatric population groups.
A recent study of the incidence of CHD in an Asian pediatric population showed higher incidence of PS and Tetralogy of Fallot (TOF), with lower incidence of left-sided obstructive lesions, TGA and tricuspid atresia, compared with western populations12). Results of our study also revealed lower incidence of left sided obstruction. And the incidence of TOF was extraordinarily low, which might imply that TOF can be diagnosed relatively easily during the fetal period.
This study has several limitations. All of the subjects of this study were inpatients only of the NICU and NU, and this was a retrospective single center study. Since not all patients underwent echocardiography, minor cardiac defects might have been missed and the true incidence might be somewhat higher than that reported here. As we could not get detailed history of antenatal study with fetal echocardiography, we could not reveal the impact of fetal imaging to these changes of epidemiologic findings that might had affected. Finally, a secondary referral medical center is not absolutely free from the selection bias of the patients either.
A large, multicenter, and population-based study is needed in order to elucidate the true incidence of CHD in Korea.
References
1. Mitchell SC, Korones SB, Berendes HW. Congenital heart disease in 56,109 births. Incidence and natural history. Circulation 1971;43:323ŌĆō332.


2. Grech V, Gatt M. Syndromes and malformations associated with congenital heart disease in a population-based study. Int J Cardiol 1999;68:151ŌĆō156.


3. Jung SC, Kim SS, Yoon KS, Lee JS. Prevalence of congenital malformations and genetic diseases in Korea. J Hum Genet 1999;44:30ŌĆō34.


4. Hoffman JI. Incidence of congenital heart disease: I. Postnatal incidence. Pediatr Cardiol 1995;16:103ŌĆō113.


5. Kovalchin JP, Silverman NH. The impact of fetal echocardiography. Pediatr Cardiol 2004;25:299ŌĆō306.

6. Chung ML, Lee BS, Kim EA, Kim KS, Pi SY, Oh YM, et al. Impact of fetal echocardiography on trends in disease patterns and outcomes of congenital heart disease in a neonatal intensive care unit. Neonatology 2010;98:41ŌĆō46.


7. Levey A, Glickstein JS, Kleinman CS, Levasseur SM, Chen J, Gersony WM, et al. The impact of prenatal diagnosis of complex congenital heart disease on neonatal outcomes. Pediatr Cardiol 2010;31:587ŌĆō597.



8. Geggel RL. Conditions leading to pediatric cardiology consultation in a tertiary academic hospital. Pediatrics 2004;114:e409ŌĆōe417.


9. Jung JW, Kim NS, Lee SY, Park IS. Recent trends in the frequency of congenital heart diseases: nationwide survey in Korea [abstract] 2010;In: The 3rd Congress of Asia-Pacific Pediatric Cardiac Society; 2010 Jul 6-8; Chiba, Japan. ŌĆō225.
10. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890ŌĆō1900.


11. Lee JE, Jung KL, Kim SE, Nam SH, Choi SJ, Oh SY, et al. Prenatal diagnosis of congenital heart disease: trends in pregnancy termination rate, and perinatal and 1-year infant mortalities in Korea between 1994 and 2005. J Obstet Gynaecol Res 2010;36:474ŌĆō478.


12. Wu MH, Chen HC, Lu CW, Wang JK, Huang SC, Huang SK. Prevalence of congenital heart disease at live birth in Taiwan. J Pediatr 2010;156:782ŌĆō785.


13. Yang XY, Li XF, Lu XD, Liu YL. Incidence of congenital heart disease in Beijing, China. Chin Med J (Engl) 2009;122:1128ŌĆō1132.

14. Khoshnood B, De Vigan C, Vodovar V, Goujard J, Lhomme A, Bonnet D, et al. Trends in prenatal diagnosis, pregnancy termination, and perinatal mortality of newborns with congenital heart disease in France, 1983-2000: a population-based evaluation. Pediatrics 2005;115:95ŌĆō101.


15. Malik S, Cleves MA, Zhao W, Correa A, Hobbs CA. National Birth Defects Prevention Study. Association between congenital heart defects and small for gestational age. Pediatrics 2007;119:e976ŌĆōe982.


16. Godfrey M, Schimmel MS, Hammerman C, Farber B, Glaser J, Nir A. The incidence of congenital heart defects in very low birth weight and extremely low birth weight infants. Isr Med Assoc J 2010;12:36ŌĆō38.

17. Tanner K, Sabrine N, Wren C. Cardiovascular malformations among preterm infants. Pediatrics 2005;116:e833ŌĆōe838.


18. Dees E, Lin H, Cotton RB, Graham TP, Dodd DA. Outcome of preterm infants with congenital heart disease. J Pediatr 2000;137:653ŌĆō659.


19. Kecskes Z, Cartwright DW. Poor outcome of very low birthweight babies with serious congenital heart disease. Arch Dis Child Fetal Neonatal Ed 2002;87:F31ŌĆōF33.



20. Kapoor R, Gupta S. Prevalence of congenital heart disease, Kanpur, India. Indian Pediatr 2008;45:309ŌĆō311.

21. Forrester MB, Merz RD. Descriptive epidemiology of selected congenital heart defects, Hawaii, 1986-1999. Paediatr Perinat Epidemiol 2004;18:415ŌĆō424.


22. Stephensen SS, Sigfusson G, Eiriksson H, Sverrisson JT, Torfason B, Haraldsson A, et al. Congenital cardiac malformations in Iceland from 1990 through 1999. Cardiol Young 2004;14:396ŌĆō401.


23. Sam├Īnek M, Vor├Łskova M. Congenital heart disease among 815,569 children born between 1980 and 1990 and their 15-year survival: a prospective Bohemia survival study. Pediatr Cardiol 1999;20:411ŌĆō417.


Fig.┬Ā1
Numbers of patients diagnosed with congenital heart disease (CHD) during the study. Patent ductus arteriosus (PDA) in prematurity, mild peripheral pulmonary stenosis, and small atrial septal defect (ASD)Ōēż3 mm were excluded in this study. VSD, ventricular septal defect; PS, pulmonic stenosis.
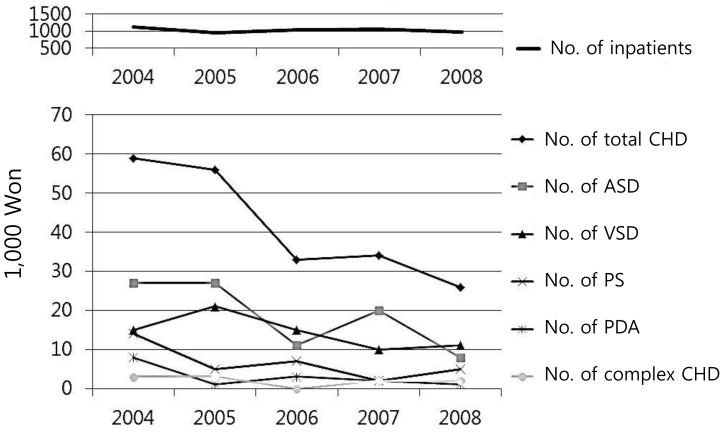
Fig.┬Ā2
Incidence of congenital heart disease (CHD) in full-term and pre-term patients among patients of each gestational age group (*P<0.001, compared with the pre-term group).

Fig.┬Ā3
Incidence of congenital heart disease (CHD) (%) in each birth weight group during the study period (*P<0.001, compared with the other 2 groups). BW, body weight.
Table┬Ā1
Incidence of Congenital Heart Disease (CHD) in Full-term and Pre-term Patients for Each Gestational Age Group during the Study Period






 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


