Introduction
Single coronary artery (SCA) is a rare congenital anomaly of the coronary arteries arising from a single coronary ostium1). The clinical significance of SCA is not clear, and it is generally considered to be a benign entity. There are some case reports of SCA in adults, but there are a few such reported cases in children. We report a case of a 13-year-old girl with right coronary artery arising from the left circumflex artery who presented with chest pain.
Case report
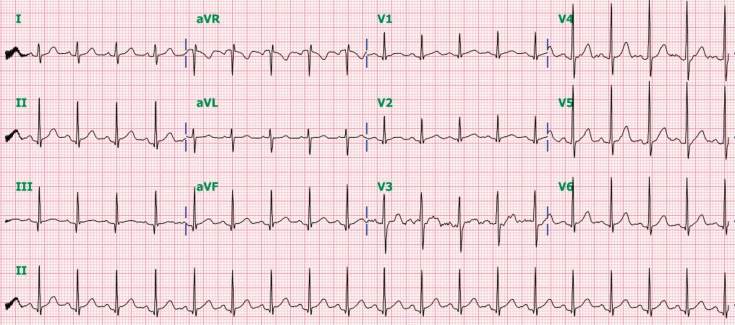
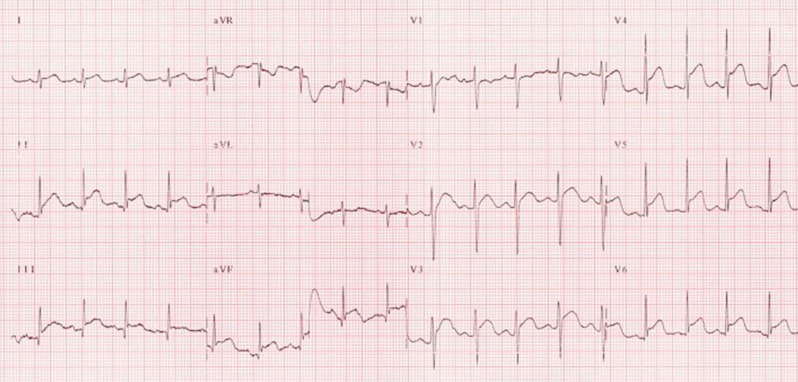
A previously healthy 13-year-old girl visited our Emergency Department due to left-sided chest pain that had occurred suddenly 10 hours ago. The pain was continuous pressing in nature without any radiation, and it improved on bending forward but worsened with deep inspiration. She had no specific past medical history such as Kawasaki disease, asthma, and no family history of heart or lung disease. She did not appear ill; and her vital signs were as follows: blood pressure was 133/79 mmHg, heart rate was 117 beats/min, and temperature was 37.6Ōäā. Her weight was 40 kg. The physical examination did not reveal any other specific findings, especially her lung sound was normal Electrocardiogram (ECG) showed sinus tachycardia with a heart rate of 114 beats/min without ST segment changes (Fig. 1), and the chest x-ray was normal. We performed echocardiography that revealed normal regional wall motion and normal anatomy. However, her cardiac enzyme levels were slightly elevated; N-terminal prohormone brain natriuretic peptide was 257.6 pg/mL, troponin I was 2.138 ng/mL, and creatine kinase-myoglobin (CK-MB) was 13.02 ng/mL. The next day, she again complained of severe chest pain. Her blood pressure was 100/60 mmHg. Her ECG was taken again, and it showed marked ST elevation in the V4-V6 left precordial leads and inferior leads and ST depression in aVR lead, which was suggestive of myocardial ischemia (Fig. 2). Also, her cardiac enzyme levels were elevated; troponin I was 4.310 ng/mL, CK-MB was 10.78 ng/mL. Although the chest pain regressed spontaneously, further evaluation was performed.
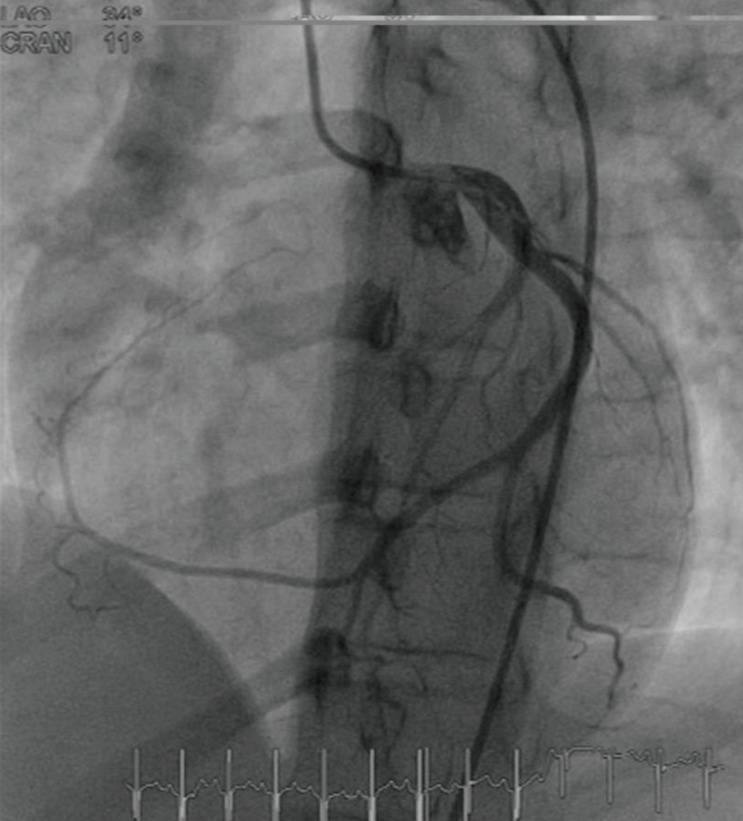
We performed coronary angiography; left coronary artery (LCA) was bifurcated normally into left anterior descending (LAD) and left circumflex (LCX) coronary arteries, and it showed the absence of normally originating right coronary artery (RCA). An aberrant branch was extended from the distal LCX, which crossed the crux and continued to the right atrioventricular groove, covering the territory of the RCA (Fig. 3). There was no focal stenotic lesion in LCX including abberant branch. LAD and its branches (septal perforator branch, diagonal branch) also had no stenotic lesion. We also performed cardiac computed tomography and confirmed the absence of the RCA and the presence of a well-developed LCX coronary artery covering the right side of the heart (Fig. 4). A treadmill test was performed and the results were normal. She had no symptoms and electrocardiographic findings were normal during exercise. She was discharged without any medications; however, a regular follow-up was recommended.
Discussion
An isolated SCA is defined when only one coronary artery arises from the aorta by a single coronary ostium, supplying the entire heart1). SCA is a very rarely encountered disease entity, and its reported incidence in adults is only from 0.024% to 0.066%1,2). Also, it is occasionally associated with other cardiac anomalies such as transposition of the great vessels, a coronary arteriovenous fistula, or a bicuspid aortic valve3). A SCA can result in the development of cardiac ischemia, cardiomyopathy, and congestive heart failure4). Myocardial ischemia may occur if there is only insignificant or absent coronary artery narrowing.
Based on Lipton classifications1), the first division was made between the right-type (R) and left-type (L) according to the site of origin of SCA. Next, the artery was designated as group I, II, or III depending on its anatomical course. Group I had an anatomical course of either a RCA or LCA. Group II anomalies arise from the proximal part of the normal RCA or LCA, and cross the base of the heart before assuming the normal position of the inherent coronary artery. Group III describes the anomaly where the LAD and LCX arise separately from the proximal part of the normal RCA. According to this classification1), our patient was classified as L-I type, which is the presence of a markedly dominant LCX artery but the absence of a RCA. There would be some published reports of an anomalous RCA arising from the LAD5,6), but the reported cases of an anomalous RCA originating from the LCX are relatively less7,8,9,10).
Sudden death in young competitive athletes is often caused SCA11). But, there are only a few cases in the pediatric and adolescent age group; these anomalies are rarely suspected or identified during life and are usually first recognized at autopsy, largely because there is insufficient clinical suspicion as well as the difficulties implicit in routine examination or clinical testing for these malformations12).
Mostly, SCA has a benign course, and it is known that SCA does not interfere with coronary perfusion. But some reports stated that patients with SCA could develop significant ischemic heart disease13), and the patients with SCA who usually present with myocardial infarction have stenosis of the coronary artery. Especially, the R II-III type and L II-III type anomalies, having a coronary artery branch following a dangerous course, may predispose to fatal myocardial ischemia. But there were some reports suggesting that the incidence of coronary artery bypass graft in patients with L-I type of anomaly such as the RCA originating from the LCX was about 33%9).
SCA was incidentally detected on angiography while we were evaluating the patient for chest pain. Our patient had abnormal ECG showing ST-elevation in inferior leads and left precordial leads with reciprocal change in aVR and elevated cardiac enzyme levels suggesting myocardial ischemia. The cause of myocardial ischemia was uncertain, because there was no stenosis and the result of treadmill test was negative. Certain mechanisms could be considered, such as the coronary steal phenomenon due to the abnormal vessel or microvascular damage, and slow controlled ischemia caused by long travel distance of abnormal coronary artery7). There is a report of a case similar to our patient, in which there was no stenosis, but the authors thought that the patient had myocardial ischemia due to an abnormally slow coronary flow in the RCA, because there was abnormally slow angiographic filling in the RCA territory7). Hence, they treated the patient with calcium channel blockers like diltiazem and nitrates, and the chest pain resolved after taking medications. The cause of chest pain can be considered to be coronary artery spasm-induced myocardial ischemia10). Since we did not perform coronary artery spasm test such as the ergonovine test, the diagnosis of coronary artery spasm could not be definitely excluded.
We advised her to avoid heavy exercise and to develop healthy eating habits to prevent atherosclerosis. Also, we explained to the patient that she might need to take medications and to undergo a regular follow-up of symptoms. If a patient complains of chest pain due to SCA, but does not exhibit significant stenotic lesions in the SCA on coronary angiography like our patient, other tests should be considered. We have to consider performing stress tests such as single photon emission computed tomography, treadmill test whether or not myocardial ischemia develops in response to stress.
And strategies for clinical identification of coronary artery anomalies are as follows: if clinical symptom such as exertional syncope or chest pain appears, physicians have to consider noninvasive examination like transthoracic or transesophageal echocardiography. And then, sonographer cannot find coronary arteries from their usual coronary sinuses, we may suggest further examination such as coronary arteriography or computed tomography.
We believe that this is the first report of a pediatric case of SCA with RCA originating from the LCX artery in Korean population. Therefore, although it is very rare, we can consider the diagnosis of coronary artery anomaly in pediatric patients with an unusual presentation of myocardial ischemia.




 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


