Introduction
Rotavirus and norovirus are the most common causative agents of acute gastroenteritis in children aged <5 years worldwide [1]. Children with rotavirus infection of the small intestine may experience diarrhea, vomiting, and fever. However, it is generally self-limiting and lasts only a few days [2]. Since the introduction of rotavirus vaccines, the burden of the disease has reduced significantly; however, rotavirus remains a common cause of hospitalization [3]. Rotavirus is known to cause systemic infection according to recent extraintestinal spread findings [4]. Rotavirus infection shows a wide spectrum of central nervous system (CNS) manifestations, including benign convulsions with mild gastroenteritis (CwG), acute meningoencephalitis, white matter injuries, and lethal encephalitis/encephalopathies [4,5]. However, although it has not yet been clearly identified as a risk factor for rotavirus-related CNS complications, regional or racial differences are suspected, as it is reported more often in East Asia than in Europe or the United States [6].
CwG is the most commonly encountered CNS complication, occurring in previously healthy infants and children aged 6 months to 3 years [7]. It is characterized by afebrile brief tonic-clonic seizures between the 1st and 5th sick days of gastroenteritis, tending to occur repetitively over several days. However, the findings of interictal electroencephalography, cerebrospinal fluid (CSF), and brain magnetic resonance imaging (MRI) examinations are mostly normal [1,7]. Despite clustered seizures, long-term anti-seizure medication is usually not required because of the good prognosis [7]. In addition to CwG, diverse clinicoradiological features related to rotavirus infection in the brain have been reported, as various brain MRI protocols, such as fluid attenuated inversion recovery and diffusion-weighted imaging, have been widely and early applied in clinical settings [5]. Rotavirus-induced CNS complications primarily involve acute encephalopathy with transient and reversible changes rather than acute encephalitis with destructive lesions on MRI. These include white matter injuries in neonates, mild encephalopathy with a reversible splenial lesion, acute encephalopathy with biphasic seizures and reduced diffusion, and posterior reversible encephalopathy syndrome [8-10]. Despite many reports of rotavirus infection and CNS manifestations, definite and consistent evidence of its pathophysiological mechanisms is lacking [2,11].
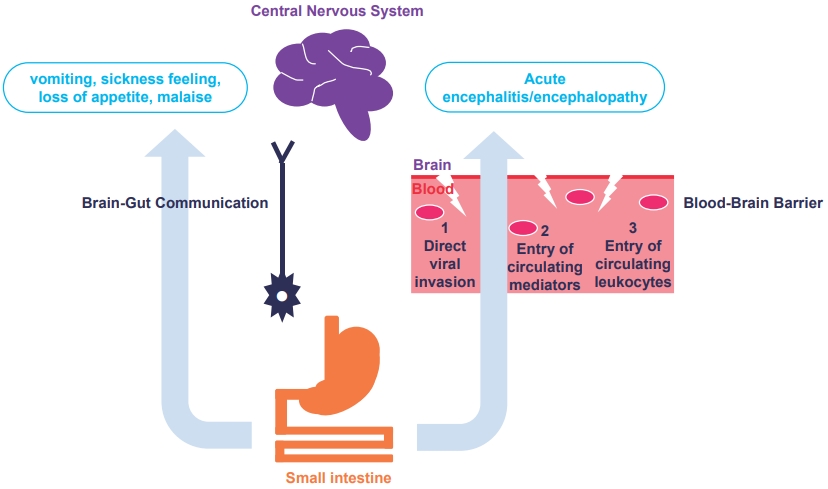
Based on the author’s arguments, the following hypotheses were proposed (Fig. 1) [5]. First, CNS-driven symptoms such as vomiting, sickness, loss of appetite, and malaise are considered brain-gut communication in rotavirus infection [2,11]. This includes activating the vagal nerves that project to regions of the brain via enterotoxin nonstructural viral protein 4-dependent 5-hydroxytryptamine release [11]. Second, previously described CNS complications are explained as direct CNS effects, although rotavirus antigen and ribonucleic acid are rarely detected in the CSF [5]. Potential mechanisms by which the pathogen causes these diverse CNS complications are: (1) direct viral invasion into the CNS; (2) CNS entry of deleterious brain-damaging mediators; and (3) CNS entry of activated circulating leukocytes [5]. The most likely mechanism is that the blood-borne rotavirus enters the brain via disrupted and increased vascular permeability of the bloodbrain barrier (BBB); thus, the direct viral infection of neuronal cells induces cytopathic results [2,11]. Various circulating mediators produced during rotavirus infection can damage BBB integrity and induce hypothalamic dysregulation. According to several recent studies, inflammatory cytokines and reactive oxygen species levels are significantly elevated in the CSF [2,5]. Finally, systemic inflammation-induced circulating leukocytes can transmigrate across the BBB and injure neuronal cells.
Although the burden of rotavirus infection has been reduced owing to the widespread introduction of vaccines, rotavirusinduced CNS complications remain important. Diverse clinicoradiological features can be identified using brain imaging in the early stages of neurological symptoms. This may be attributed to the gut-brain communication as well as direct CNS entry of various mediators, immune cells, and even the virus itself. An increased understanding of rotavirus-induced CNS manifestations will enable more precise management in the future.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


