Article Contents
| Clin Exp Pediatr > Volume 65(11); 2022 |
|
Abstract
In the early days of the coronavirus disease 2019 (COVID-19) pandemic, allergic diseases, especially asthma, were considered to be risk factors for severe COVID-19 infection, hospitalization, and death. These concerns stemmed from the idea that individuals with allergic diseases are generally more susceptible to respiratory virus infections, which are major causes of exacerbation of allergic diseases. However, epidemiologic data with mechanistic studies showed that the associations between severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and clinical outcomes of allergic diseases are complex and affected by diverse factors such as allergic disease severity, phenotypes, and control status with current medications. In addition, children generally have less severe clinical outcomes of COVID-19 than those of adults, which complicates the association between allergic diseases and COVID-19-related outcomes among them. The present review summarizes the potential association between allergic diseases and COVID-19-related outcomes and discusses the factors requiring consideration. The findings viewed herein will aid the management of allergic diseases in patients with SARS-CoV-2 infection and the establishment of medical polices for managing patients with allergic diseases.
Individuals with allergic diseases, particularly asthma, are more susceptible to respiratory virus infections, which are the leading causes of exacerbations of allergic diseases [1]. Accordingly, in the early days of the coronavirus disease 2019 (COVID-19) pandemic, patients with allergic diseases were considered to have higher risk for COVID-19-related morbidity and mortality [2]. However, accumulating evidence suggests that allergic diseases are not always associated with poor clinical outcomes of COVID-19 and that the relation between allergic diseases and COVID-19 is rather complex. Considering the relatively high prevalence of allergic diseases, a considerable number of patients with them become infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Various factors of allergic diseases, including phenotypes, medications, and control status, should be considered when predicting the clinical outcomes of COVID-19 in patients with allergic diseases. The present review summarizes the complex relationship between COVID-19-related outcomes and allergic diseases (Table 1) to aid the management of SARS-CoV-2 infections among patients with allergic diseases.
Since the beginning of the COVID-19 pandemic, patients with asthma and their caregivers have been concerned about increased susceptibility to SARS-CoV-2 infection and severe COVID-19. The COVID-19 pandemic has affected the patterns of visits to medical institutions during asthma exacerbations. Patients with more severe asthma visited emergency departments and were hospitalized more often during versus before the pandemic [3]. To better predict the clinical outcomes of patients with asthma who become infected with SARS-CoV-2, several factors including the medical history, severity, and treatment of individual asthma cases should be considered. Moreover, to manage asthma during the COVID-19 pandemic, each patient’s asthma phenotype and endotype require elucidation.
Viral respiratory infections are common causes of asthma exacerbation in children and adults. Several studies have reported a substantial reduction in asthma exacerbation during the COVID-19 pandemic [4-10]. However, whether SARS-CoV-2 infections cause or are associated with acute exacerbation in patients with asthma remains controversial [11]. Such associations might be independent of improved asthma control during the COVID-19 pandemic considering possible confounding factors such as social distancing, minimal social interactions, and lower susceptibility of younger individuals to SARS-CoV-2 infection [5,12]. To date, few studies have reported that SARS-CoV-2 infection can trigger asthma exacerbation but does not cause severe asthma exacerbation [13-15]. Further large-scale studies are needed to confirm these associations between SARS-CoV-2 infection and asthma exacerbation.
In the early stages of the COVID-19 pandemic, the effect of asthma on COVID-19 severity in children was examined in small studies, partially because of the lower prevalence of COVID-19 in children [16]. Whether asthma is a risk factor for COVID-19-associated hospitalization or severe COVID-19 remains controversial. Some studies have reported that asthma is not a risk factor for severe COVID-19 (Table 2) [16,17]. However, others reported that children (12–17 years) with asthma are at higher risk of requiring hospitalization for COVID-19 [18]. It has also reported that COVID-19 patients aged ≥16 years with asthma are more likely to require critical care (adjusted odds ratio [aOR], 1.20; 95% confidence interval [CI], 1.05–1.37), noninvasive ventilation (aOR, 1.36; 95% CI, 1.18–1.57), and oxygen supplementation (aOR, 1.33; 95% CI, 1.17–1.50) than those without asthma [19]. These findings suggest that the association between asthma and severe COVID-19 is complex and that the characteristics of the study population require consideration to reveal the potential connections.
Asthma severity and control status affect COVID-19 severity. Because the prevalence of severe asthma in children is relatively low compared with that in adults [20], few studies have reported the effects of severe asthma on the clinical outcomes of COVID-19 in adolescents. Children aged 12-17 years with asthma prescribed one (adjusted hazard ratio [aHR], 2.58; 95% CI, 1.82–3.66) or 2 or more (aHR, 3.80; 95% CI, 2.41–5.95) courses of oral corticosteroids in the year preceding the COVID-19 pandemic were reportedly at greater risk of COVID-19-related hospitalization [18]. In adults, uncontrolled asthma (OR, 1.64; 95% CI, 1.35–2.00) and the requirement of higher amounts of asthma medications, such as high-dose inhaled corticosteroid (ICS) combined with long-acting β-agonists (OR, 1.40; 95% CI, 1.22–1.60), was associated with severe COVID-19.21) Also, in patients aged ≥16 years, severe asthma significantly increases COVID-19-related mortality rates (aHR, 1.96; 95% CI, 1.25–3.08) [19].
One reason for the ongoing debate about the association between asthma and COVID-19 outcome is the difference in asthma phenotype and endotype among patients [17,22]. Allergic asthma, compared with nonallergic asthma, is associated with a lower risk of COVID-19-related hospitalization [22]. Moreover, nonallergic asthma is associated with severe COVID-19, while allergic asthma is not [22]. Although the mechanisms underlying these associations are unclear, the relation between angiotensin-converting enzyme 2 (ACE2) receptor expression in the airway and the degree of Th2 inflammation with genetic predisposition may provide some clues [22-24].
ICS is the mainstay of asthma medications [25]. However, concern exists regarding whether ICS use is associated with an increased risk of susceptibility to SARS-CoV-2 infection or severe COVID-19 due to the potential immunosuppressive effects of ICS through increased susceptibility to secondary infection, viral replication promotion, and delayed viral clearance [26,27]. However, ICS can be safely used in patients with asthma even during the COVID-19 pandemic and SARS-CoV-2 infection [28]. Several studies have reported that patients aged 16–49 years using ICS with or without long-acting β-agonists do not carry an increased risk for COVID-19-related in-hospital mortality [19]. The proportion of ICS usage in adult asthma patients is significantly lower among those who are hospitalized due to COVID-19 than among those who are not [29]. Moreover, ICS use in adult asthma patients is not associated with COVID-19 related mortality [28]. The potential protective role of ICS against COVID-19 may be due to the suppressive effect of ICS on coronavirus replication [30], which can also support its use to treat COVID-19 itself. Furthermore, ACE2 and transmembrane serine protease 2 (TMPRSS2) gene expression levels are lower in asthma patients receiving ICS treatment [31]. Previous studies reported that ICS use is safe regardless of SARS-CoV-2 infection; therefore, ICS should be used as prescribed. The discontinuation of asthma medication is linked with poorly controlled asthma and decreases quality of life [32,33]. Therefore, maintaining a stable asthmatic status helps improve the clinical course and outcomes of COVID-19.
Studies on the safety of chronic or regular systemic corticosteroid treatment in COVID-19 patients remain scarce, and the results of the few studies to date are inconclusive. A need for systemic corticosteroid treatment indicates severe uncontrolled asthma associated with increased risks of severe COVID-19 and COVID-19-related mortality rates [2,34].
Since COVID-19 symptoms can often accompany upper respiratory tract infections, it can be difficult to distinguish from common cold and allergic rhinitis. The European Academy of Allergy and Clinical Immunology (EAACI) provides a set of criteria to distinguish COVID-19 from other rhinologic diseases using a modified Delphi process [35]. Smell dysfunction, taste dysfunction, dyspnea, and cough are predominant symptoms of COVID-19, whereas sneezing, stuffy nose, and nasal pruritus with ocular itch or redness predominantly indicate allergic rhinitis. For the common cold, a runny and stuffy nose are the most common symptoms. When more than 2 rhinologic diseases develop simultaneously, more diverse symptoms may present.
During the COVID-19 pandemic, medications used for allergic rhinitis treatment, including intranasal corticosteroids, have been safely administered to patients with allergic rhinitis and SARS-CoV-2 infection. Although no studies have examined the association between intranasal corticosteroid use and COVID-19-related disease burden in children, studies in adults showed that intranasal corticosteroid therapy is associated with a lower risk of severe COVID-19 outcomes, including hospitalization, intensive care unit admission, and mortality [36]. Similar patterns were observed when intranasal corticosteroids were administered to patients who had never been diagnosed with allergic rhinitis [36]. Therefore, intranasal corticosteroids can be safely used in the management of allergic rhinitis even during SARS-CoV-2 infection.
Atopic dermatitis is one of the most common chronic inflammatory skin diseases [37]. The association between atopic dermatitis and COVID-19 outcomes has been less commonly investigated [38]. During the COVID-19 pandemic, an increased incidence of skin irritation and exacerbation of atopic dermatitis was reported, particularly among healthcare workers with prolonged use of personal protective equipment and increased work-related stress levels. Some studies in adults showed that atopic dermatitis was associated with an increased risk of COVID-19 [39,40]. Conversely, others reported that patients with atopic dermatitis do not have a significantly increased risk of SARS-CoV-2 infection [41]. On the other hand, the risk of COVID-19-related hospitalization was significantly lower in children with atopic dermatitis, compared with those without atopic dermatitis, with no differences noted in the prevalence of COVID-19-related severity and critical care admission [42]. These findings underline the complex relation among SARS-CoV-2 infection, COVID-19 outcomes, and atopic dermatitis.
Furthermore, concern exists regarding the effects of medications used to treat atopic dermatitis on SARS-CoV-2 infection and COVID-19 outcomes. Treatment with methotrexate for 1 year was not associated with severe COVID-19, COVID-19-related hospitalization, or critical care admission among children [42]. However, use of systemic corticosteroids for 1 year was associated with an increased risk of COVID-19-related hospitalization [42]. Even during the COVID-19 pandemic, well-controlled status of atopic dermatitis with appropriate medication is important for its proper management.
Only few studies have investigated the association between food allergy and COVID-19. A recent report stated that food allergy is associated with a decreased risk of SARS-CoV-2 infection [43]. One plausible explanation might be behavioral changes in patients with food allergy, such as a decreased requency of eating out. Apart from the association between food allergy and COVID-19, emphasis was placed on appropriate strategies for the management of food allergy with anaphylaxis during the pandemic due to the restriction of access to medical facilities [44,45]. These strategies included the use of telemedicine to improve treatment decision-making, full-time carrying of epinephrine autoinjector devices, and avoidance of known allergens [44,45].
Type 2 inflammation might play a role in the association among allergic diseases, protective role of the therapies for asthma and allergic rhinitis, allergen sensitization, individuals’ allergic phenotypes and endotypes, and COVID-19-related outcomes [46]. However, further research is needed to elucidate these associations. Expression levels of ACE2, the target of SARS-CoV-2 spike protein binding, are inversely correlated with type 2 cytokine levels, whereas TMPRSS2 gene expression levels are positively correlated with type 2 cytokine levels in the primary airway epithelial cells obtained from patients with or without type 2 asthma [23]. Moreover, an inverse correlation between allergic sensitization and ACE2 expression levels in the nasal epithelium was noted regardless of the presence of asthma [24]. In children with asthma, the degree of allergic sensitization is inversely correlated with ACE2 expression levels [24]. However, ACE2 expression levels are not reduced in patients with non-atopic asthma [24], suggesting that the protective effect of allergic diseases is limited to patients with type 2 inflammation.
Blood eosinophils, a type 2 inflammatory response marker, promote protective responses against respiratory viruses [47]. Patients with eosinophil counts >200/µL show a significantly decreased risk of COVID-19-related mortality regardless of the presence of asthma in adults [48]. Adults with asthma with absolute eosinophil counts >150/µL reportedly show decreased COVID-19-related mortality rates, which supports the observation of decreased COVID-19-related mortality in patients with type 2 asthma phenotype [49].
SARS-CoV-2 infection in children has a milder clinical course and less severe morbidity and mortality than that in adults (Fig. 1) [50]. Although the reasons for age-related differences in susceptibility to and disease severity of COVID-19 remain poorly understood, several studies focused on the key host proteins involved in SARS-CoV-2 cellular entry, including ACE2, TMPRSS2, and furin protein [51], which may also play a role in the association between allergic diseases and SARS-CoV-2 infection. SARS-CoV-2 binds to ACE2 on human airway cells, and the subsequent activation of serine protease, such as TMPRSS2, stimulates the spike protein to allow cellular entry [52]. ACE2 gene expression in the nasal epithelium increases with age [53,54], which can explain the decreased susceptibility to and milder symptoms of COVID-19 in children compared with that in adults. Furthermore, TMPRSS2 expression levels are increased by circulating androgens, which suggests that men are significantly more likely to develop severe COVID-19 than women and pubertal children show more severe COVID-19 symptoms than prepubertal children [55]. Although additional research is needed, differences in the expression levels of SARS-CoV-2 binding factors according to age might partially explain the differences in susceptibility to SARS-CoV-2 infection and COVID-19 severity [51].
Allergen immunotherapy can alter the clinical course of asthma and allergic rhinitis, even in children. Concern exists about the continuity of allergen immunotherapy in respiratory tract infections, including SARS-CoV-2 infection. A study on the effect of allergen immunotherapy in children infected with influenza virus indicated that children on maintenance doses of allergen immunotherapy show fewer symptoms and quick recovery from respiratory tract infections [56]. These findings suggest that allergen immunotherapy can be continued even during respiratory virus seasons, and likewise, during the COVID-19 pandemic [57].
The EAACI recommends administration of the COVID-19 vaccine at intervals of 7 days from subcutaneous allergen immunotherapy due to potential side effects [57]. In addition, it is recommended to discontinue sublingual immunotherapy 3 days before COVID-19 vaccination and resume 7 days after COVID-19 vaccination [57].
Biologics can be prescribed for uncontrolled severe asthma and moderate to severe atopic dermatitis, even in children and adolescents [58]. The biologics used in allergic diseases block type 2 inflammation pathways [58]. Some epidemiologic studies reported that biologics are not associated with an increased risk of COVID-19 [59] and that patients treated with biologics have a relatively low prevalence of COVID-19-related hospitalization [29]. Biologics used to treat asthma are not associated with increased risks of SARS-CoV-2 infection or severe COVID-19 [60-62]. In addition, dupilumab therapy for severe atopic dermatitis is safely and continuously used for better disease outcome, regardless of the presence of COVID-19 [63,64], as dupilumab does not affect antibody levels after mRNA vaccination for COVID-19 [65]. Based on the above mentioned findings, biologics can be safely used even during the COVID-19 pandemic.
The age at which children can be vaccinated against COVID-19 has been gradually expanded, although more data are required to confirm the adverse reactions of COVID-19 vaccine in younger children [66]. COVID-19 vaccination can be safely administered in children and adolescents with allergic diseases except in cases of polysorbate or poly-ethylene glycol allergy and COVID-19 vaccine allergy. The pre-vaccine risk stratification algorithm can be used with a thorough history taking of adverse reactions to vaccines or other medications [67].
Evidence is limited on the potential effects of allergen immunotherapies and biologics targeting Th2 inflammation on anti-infectious vaccines [57]. A previous study showed that allergen immunotherapy has no effect on the booster vaccine dose for tickborne encephalitis [68]. Omalizumab therapy is well tolerated in response to live attenuated influenza vaccine [69]. Although further evidence is needed, allergen immunotherapy and biologics for allergic diseases can be safely used regardless of COVID-19 vaccination.
The risk of SARS-CoV-2 infection and severe COVID-19 outcomes are not elevated in patients with well-controlled asthma, particularly the type 2 phenotype of asthma and other allergic diseases. The mainstay treatment, i.e., ICS, intranasal corticosteroid, and topical corticosteroid can be safely used even in SARS-CoV-2-infected patients with allergic diseases. COVID-19 vaccine can also be safely administered to patients with allergic diseases. Moreover, allergen immunotherapy and biologics used to treat allergic diseases can be safely continued without concern about antibody responses.
Fig. 1.
Comparison of clinical features of COVID-19 between children and adults with potential mechanisms. Children generally have less severe clinical outcomes of COVID-19 than those of adults. Differences in the expression levels of SARS-CoV-2 binding factors, such as ACE2, TMPRSS2, and furin protein, according to age might partially explain the differences in susceptibility to SARS-CoV-2 infection and COVID-19 severity. COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ACE2, angiotensin-converting enzyme 2; TMPRSS2, transmembrane serine protease 2.
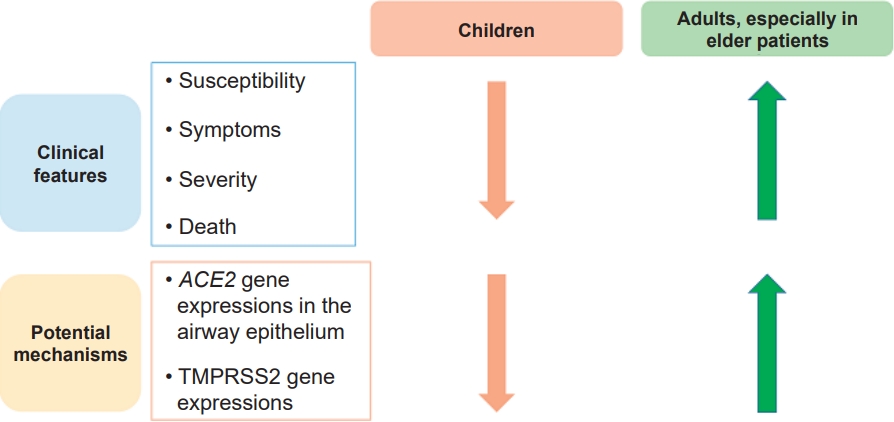
Table 1.
Summary of the association between allergic diseases and COVID-19-related outcomes
Table 2.
Summary of results of studies on the impact of asthma and allergic rhinitis on COVID-19-related outcomes
References
1. Cui J, Zhang Y, Zhao H, Sun X, Chen Z, Zhang Q, et al. The relationship between lower respiratory tract microbiome and allergic respiratory tract diseases in children. Front Microbiol 2021;12:630345.



2. Adir Y, Saliba W, Beurnier A, Humbert M. Asthma and COVID-19: an update. Eur Respir Rev 2021;30:210152.



3. Alabdulkarim N, Gai J, Bost J, Pillai D, Teach SJ, Rastogi D. Effect of the COVID-19 pandemic on morbidity among children hospitalized for an asthma exacerbation. Ann Allergy Asthma Immunol 2022;129:194. –8. e1.


4. Yang Z, Wang X, Wan XG, Wang ML, Qiu ZH, Chen JL, et al. Pediatric asthma control during the COVID-19 pandemic: a systematic review and meta-analysis. Pediatr Pulmonol 2022;57:20–5.




5. Fan HF, He CH, Yin GQ, Qin Y, Jiang N, Lu G, et al. Frequency of asthma exacerbation in children during the coronavirus disease pandemic with strict mitigative countermeasures. Pediatr Pulmonol 2021;56:1455–63.



6. Ferraro VA, Zamunaro A, Spaggiari S, Di Riso D, Zanconato S, Carraro S. Pediatric asthma control during the COVID-19 pandemic. Immun Inflamm Dis 2021;9:561–8.




7. Golan-Tripto I, Arwas N, Maimon MS, Bari R, Aviram M, Gatt D, et al. The effect of the COVID-19 lockdown on children with asthma-related symptoms: a tertiary care center experience. Pediatr Pulmonol 2021;56:2825–32.



8. Guijon OL, Morphew T, Ehwerhemuepha L, Galant SP. Evaluating the impact of coronavirus disease 2019 on asthma morbidity: a comprehensive analysis of potential influencing factors. Ann Allergy Asthma Immunol 2021;127:91–9.


9. Levene R, Fein DM, Silver EJ, Joels JR, Khine H. The ongoing impact of COVID-19 on asthma and pediatric emergency health-seeking behavior in the Bronx, an epicenter. Am J Emerg Med 2021;43:109–14.



10. Shah SA, Quint JK, Sheikh A. Impact of COVID-19 pandemic on asthma exacerbations: Retrospective cohort study of over 500,000 patients in a national English primary care database. Lancet Reg Health Eur 2022;100428.



11. Skevaki C, Karsonova A, Karaulov A, Fomina D, Xie M, Chinthrajah S, et al. SARS-CoV-2 infection and COVID-19 in asthmatics: a complex relationship. Nat Rev Immunol 2021;21:202–3.




12. Solanke F, Easton S, Selby A, James D, Roberts G. Impact of COVID-19 pandemic on emergency department attendances for young people. Arch Dis Child 2022;107:e27.

13. Ruano FJ, Somoza Alvarez ML, Haroun-Diaz E, Vazquez de la Torre M, Lopez Gonzalez P, Prieto-Moreno A, et al. Impact of the COVID-19 pandemic in children with allergic asthma. J Allergy Clin Immunol Pract 2020;8:3172–4.e1.



14. Ono Y, Obayashi S, Horio Y, Niimi K, Hayama N, Ito Y, et al. Asthma exacerbation associated with COVID-19 pneumonia. Allergol Int 2021;70:129–30.



15. Garcia-Pachon E, Ruiz-Alcaraz S, Baeza-Martinez C, Zamora-Molina L, Soler-Sempere MJ, Padilla-Navas I, et al. Symptoms in patients with asthma infected by SARS-CoV-2. Respir Med 2021;185:106495.



16. Nursoy MA, Bulbul L, Yazici M, Altinel N, Ustabas Kahraman F, Ozkul Saglam N, et al. Comparison of clinical features of COVID-19 infection in children with asthma and their healthy peers. Pediatr Pulmonol 2022;57:1693–700.




17. Eggert LE, He Z, Collins W, Lee AS, Dhondalay G, Jiang SY, et al. Asthma phenotypes, associated comorbidities, and long-term symptoms in COVID-19. Allergy 2022;77:173–85.




18. Dolby T, Nafilyan V, Morgan A, Kallis C, Sheikh A, Quint JK. Relationship between asthma and severe COVID-19: a national cohort study. Thorax 2022;Mar 30 thoraxjnl-2021-218629. https://doi.org/10.1136/thoraxjnl-2021-218629. [Epub].

19. Bloom CI, Drake TM, Docherty AB, Lipworth BJ, Johnston SL, Nguyen-Van-Tam JS, et al. Risk of adverse outcomes in patients with underlying respiratory conditions admitted to hospital with COVID-19: a national, multicentre prospective cohort study using the ISARIC WHO Clinical Characterisation Protocol UK. Lancet Respir Med 2021;9:699–711.


20. Lee E, Song DJ, Kim WK, Suh DI, Baek HS, Shin M, et al. Associated factors for asthma severity in Korean children: a Korean childhood asthma study. Allergy Asthma Immunol Res 2020;12:86–98.




21. Karlsson Sundbaum J, Konradsen JR, Vanfleteren L, Axelsson Fisk S, Pedroletti C, Sjoo Y, et al. Uncontrolled asthma predicts severe COVID-19: a report from the Swedish National Airway Register. Ther Adv Respir Dis 2022;16:17534666221091183.


22. Zhu Z, Hasegawa K, Ma B, Fujiogi M, Camargo CA Jr, Liang L. Association of asthma and its genetic predisposition with the risk of severe COVID-19. J Allergy Clin Immunol 2020;146:327–9.e4.



23. Kimura H, Francisco D, Conway M, Martinez FD, Vercelli D, Polverino F, et al. Type 2 inflammation modulates ACE2 and TMPRSS2 in airway epithelial cells. J Allergy Clin Immunol 2020;146:80–8.e8.



24. Jackson DJ, Busse WW, Bacharier LB, Kattan M, O'Connor GT, Wood RA, et al. Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2. J Allergy Clin Immunol 2020;146:203–6e3.



25. Chipps BE, Murphy KR, Oppenheimer J. 2020 NAEPP guidelines update and GINA 2021-asthma care differences, overlap, and challenges. J Allergy Clin Immunol Pract 2022;10:S19–30.


26. Singanayagam A, Glanville N, Girkin JL, Ching YM, Marcellini A, Porter JD, et al. Corticosteroid suppression of antiviral immunity increases bacterial loads and mucus production in COPD exacerbations. Nat Commun 2018;9:2229.




27. Singanayagam A, Glanville N, Cuthbertson L, Bartlett NW, Finney LJ, Turek E, et al. Inhaled corticosteroid suppression of cathelicidin drives dysbiosis and bacterial infection in chronic obstructive pulmonary disease. Sci Transl Med 2019;11:e. aav3879.



28. Adir Y, Fireman Klein E, Saliba W. Inhaled corticosteroids and COVID-19 outcomes in asthma: the Israeli experience. ERJ Open Res 2022;8:00014.



29. Izquierdo JL, Almonacid C, Gonzalez Y, Del Rio-Bermudez C, Ancochea J, Cardenas R, et al. The impact of COVID-19 on patients with asthma. Eur Respir J 2021;57:2003142.



30. Matsuyama S, Kawase M, Nao N, Shirato K, Ujike M, Kamitani W, et al. The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting the viral replication-transcription complex in cultured cells. J Virol 2020;95:e01648–20.




31. Peters MC, Fahy JV. Erratum: COVID-19-related Genes in sputum cells in asthma: relationship to demographic features and corticosteroids. Am J Respir Crit Care Med 2020;202:1744–6.



32. Cekic S, Karali Z, Cicek F, Canitez Y, Sapan N. The impact of the COVID-19 pandemic in adolescents with asthma. J Korean Med Sci 2021;36:e339.




33. Lacwik P, Szydlowska D, Kupczyk M, Palczynski C, Kuna P. High levels of anxiety during the COVID-19 pandemic as a risk factor of clinical worsening in patients with severe asthma. J Allergy Clin Immunol Pract 2021;9:1381–3.



34. Chhiba KD, Patel GB, Vu THT, Chen MM, Guo A, Kudlaty E, et al. Prevalence and characterization of asthma in hospitalized and nonhospitalized patients with COVID-19. J Allergy Clin Immunol 2020;146:307. –14.e4. .



35. Hagemann J, Onorato GL, Jutel M, Akdis CA, Agache I, Zuberbier T, et al. Differentiation of COVID-19 signs and symptoms from allergic rhinitis and common cold: an ARIA-EAACI-GA(2) LEN consensus. Allergy 2021;76:2354–66.

36. Strauss R, Jawhari N, Attaway AH, Hu B, Jehi L, Milinovich A, et al. Intranasal corticosteroids are associated with better outcomes in coronavirus disease 2019. J Allergy Clin Immunol Pract 2021;9:3934–40.e9.



38. Alkhalifah A. Risk factors for hand eczema in the general population of Saudi Arabia during the COVID-19 pandemic: an internet-based cross-sectional study. JAAD Int 2022;6:119–24.



39. Fan R, Leasure AC, Damsky W, Cohen JM. Association between atopic dermatitis and COVID-19 infection: a case-control study in the All of Us research program. JAAD Int 2022;6:77–81.



40. Patrick MT, Zhang H, Wasikowski R, Prens EP, Weidinger S, Gudjonsson JE, et al. Associations between COVID-19 and skin conditions identified through epidemiology and genomic studies. J Allergy Clin Immunol 2021;147:857–69.e7.



41. Nguyen C, Yale K, Casale F, Ghigi A, Zheng K, Silverberg JI, et al. SARS-CoV-2 infection in patients with atopic dermatitis: a cross-sectional study. Br J Dermatol 2021;185:640–1.




42. Raiker R, Pakhchanian H, Jenkins K, Shen LY. COVID-19 outcomes in pediatric patients with atopic dermatitis: a multicenter analysis. Dermatitis 2022;Apr 28 https://doi.org/10.1097/DER.0000000000000881. [Epub].

43. Seibold MA, Moore CM, Everman JL, Williams BJM, Nolin JD, Fairbanks-Mahnke A, et al. Risk factors for SARS-CoV-2 infection and transmission in households with children with asthma and allergy: a prospective surveillance study. J Allergy Clin Immunol 2022;150:302–11.



44. Brar KK, Harizaj A, Nowak-Wegrzyn A. Management of anaphylaxis during the SARS-CoV-2 pandemic. Curr Treat Options Allergy 2021;8:88–96.




45. Greenhawt M, Shaker M, Stukus DR, Fleischer DM, Hourihane J, Tang MLK, et al. Managing food allergy in schools during the COVID-19 pandemic. J Allergy Clin Immunol Pract 2020;8:2845–50.



46. Carr TF, Kraft M. Asthma and atopy in COVID-19: 2021 updates. J Allergy Clin Immunol 2022;149:562–4.



47. Flores-Torres AS, Salinas-Carmona MC, Salinas E, Rosas-Taraco AG. Eosinophils and respiratory viruses. Viral Immunol 2019;32:198–207.


48. Ho KS, Howell D, Rogers L, Narasimhan B, Verma H, Steiger D. The relationship between asthma, eosinophilia, and outcomes in coronavirus disease 2019 infection. Ann Allergy Asthma Immunol 2021;127:42–8.



49. Ferastraoaru D, Hudes G, Jerschow E, Jariwala S, Karagic M, de Vos G, et al. Eosinophilia in asthma patients is protective against severe COVID-19 illness. J Allergy Clin Immunol Pract 2021;9:1152–62.e3.



50. Moon HJ, Kim K, Kang EK, Yang HJ, Lee E. Prediction of COVID-19-related mortality and 30-day and 60-day survival probabilities using a nomogram. J Korean Med Sci 2021;36:e248.




51. Abrehart T, Suryadinata R, McCafferty C, Jacobson J, Ignjatovic V, Robinson P, et al. Age-related differences in SARS-CoV-2 binding factors: An explanation for reduced susceptibility to severe COVID-19 among children? Paediatr Respir Rev 2022;S1526-0542(22)00009-4. https://doi.org/10.1016/j.prrv.2022.01.008. [Epub].


52. Oz M, Lorke DE. Multifunctional angiotensin converting enzyme 2, the SARS-CoV-2 entry receptor, and critical appraisal of its role in acute lung injury. Biomed Pharmacother 2021;136:111193.



53. Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA 2020;323:2427–9.



54. Heinonen S, Helve O, Andersson S, Janer C, Suvari L, Kaskinen A. Nasal expression of SARS-CoV-2 entry receptors in newborns. Arch Dis Child Fetal Neonatal Ed 2022;107:95–7.


55. Vahidy FS, Pan AP, Ahnstedt H, Munshi Y, Choi HA, Tiruneh Y, et al. Sex differences in susceptibility, severity, and outcomes of coronavirus disease 2019: Cross-sectional analysis from a diverse US metropolitan area. PLoS One 2021;16:e0245556.



56. Li Y, Wang D, Zhi L, Zhu Y, Qiao L, Zhu Y, et al. Respiratory tract infections in children with allergic asthma on allergen immunotherapy during influenza season. Sci Rep 2021;11:2083.




57. Jutel M, Torres MJ, Palomares O, Akdis CA, Eiwegger T, Untersmayr E, et al. COVID-19 vaccination in patients receiving allergen immunotherapy (AIT) or biologicals-EAACI recommendations. Allergy 2022;77:2313–36.




58. Russo D, Di Filippo P, Attanasi M, Lizzi M, Di Pillo S, Chiarelli F. Biologic therapy and severe asthma in children. Biomedicines 2021;9:760.



59. Adir Y, Humbert M, Saliba W. COVID-19 risk and outcomes in adult asthmatic patients treated with biologics or systemic corticosteroids: Nationwide real-world evidence. J Allergy Clin Immunol 2021;148:361–7.e13.



60. Choi YJ, Park JY, Lee HS, Suh J, Song JY, Byun MK, et al. Effect of asthma and asthma medication on the prognosis of patients with COVID-19. Eur Respir J 2021;57:2002226.



61. Rial MJ, Valverde M, Del Pozo V, Gonzalez-Barcala FJ, Martinez-Rivera C, Munoz X, et al. Clinical characteristics in 545 patients with severe asthma on biological treatment during the COVID-19 outbreak. J Allergy Clin Immunol Pract 2021;9:487–9.e1.



62. Ungar B, Glickman JW, Golant AK, Dubin C, Marushchak O, Gontzes A, et al. COVID-19 symptoms are attenuated in moderate-to-severe atopic dermatitis patients treated with dupilumab. J Allergy Clin Immunol Pract 2022;10:134–42.



63. El-Qushayri AE, Mahmoud MA, Salman S, Sarsik S, Nardone B. Dupilumab therapy in atopic dermatitis is safe during COVID-19 infection era: A systematic review and meta-analysis of 1611 patients. Dermatol Ther 2022;35:e15476.


64. Kridin K, Schonmann Y, Solomon A, Onn E, Bitan DT, Weinstein O, et al. Risk of COVID-19 and its complications in patients with atopic dermatitis undergoing dupilumab treatment-a population-based cohort study. Immunol Res 2022;70:106–13.




65. Ungar B, Lavin L, Golant AK, Gontzes A, David E, Estrada YD, et al. The impact of dupilumab treatment on severe acute respiratory syndrome coronavirus 2-coronavirus disease 2019 antibody responses in patients with atopic dermatitis. Ann Allergy Asthma Immunol 2022;128:734–6.



66. Walter EB, Talaat KR, Sabharwal C, Gurtman A, Lockhart S, Paulsen GC, et al. Evaluation of the BNT162b2 Covid-19 vaccine in vhildren 5 to 11 years of age. N Engl J Med 2022;386:35–46.



67. Banerji A, Wolfson AR, Wickner PG, Cogan AS, McMahon AE, Saff R, et al. COVID-19 vaccination in patients with reported allergic reactions: updated evidence and suggested approach. J Allergy Clin Immunol Pract 2021;9:2135–8.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


