Article Contents
| Clin Exp Pediatr > Volume 67(2); 2024 |
|
Abstract
Anorectal manometry is one of the motility tests in children performed by pediatric gastroenterologist. It evaluates the motility function of anorectal tract. It is helpful for diagnosing children with constipation, rectal hypersensitivity, fecal incontinence, Hirschsprung disease, anal achalasia, and anorectal malformations. The most common indication to perform anorectal manometry is to diagnose Hirschsprung disease. It is a safe procedure. This paper discusses recent advances and reviews on anorectal motility disorders in children.
Graphical abstract
Anorectal manometry (ARM) is the investigation which can help to diagnose motility issues of anorectal tract in children. This review discusses the role of high-resolution ARM in children to diagnose and differentiate between various types of constipation and related fecal incontinence. Constipation in children can be due to defecation dyssynergia or colonic inertia. Improper toilet training and retentive behavior while defecation is responsible for defecation dyssynergia. Colonic inertia can be due to congenital enteric neuropathy e.g., Hirschsprung disease or rare enteric myopathies leading to chronic intestinal pseudo-obstruction in children. Similarly fecal incontinence can be retentive or overflow encopresis and nonretentive fecal incontinence due to neurological or spinal cord problems. All these disorders can be differentiated with the help of ARM in children.
ARM can be done as high-resolution ARM or conventional manometry. Conventional manometry catheters have fewer sensors. They are placed at wider intervals. Their output is line plot. High-resolution manometry catheters have densely placed sensors. They have output as topographic color contour or line plot. High-resolution manometry is more expensive and less time consuming as compared to conventional manometry. Catheters used for ARM are either solid state or water perfused [1]. In water perfused catheter, external transducer detect pressure changes to water flow. In solid state cat heters transducers are built inside the catheter to generate electric signal output. Water perfused catheter are cheaper and widely available. Solid state catheters are expensive and are available mostly in research and institute setting.
Noncooperative infants and young children remains a challenge to pediatric gastroenterologist performing ARM. In noncooperative children sedation can be used. It has limited functional motility analysis. ARM is best performed in awake state. In neonates, one can complete ARM while breast feeding. But again all parameters cannot be studied. Anorectal resting pressure, squeeze pressure, cough reflex, push pressure, rectal sensation, and recto anal inhibitory reflex (RAIR) can be assessed in awake children. Conscious or awake ARM requires child’s understanding and cooperation. Under sedation only resting pressure and RAIR can be elicited. Drugs used in anesthesia and level of sedation do affect readings [2]. Muscle relaxant should be avoided while doing ARM. Ketamine do not affect anorectal metrics and can be used in children where conscious ARM is not possible [3,4].
The important indication of doing ARM is to rule out Hirschsprung disease. Table 1 highlights important indications of ARM. RAIR is absent in Hirschsprung disease and internal anal sphincter achalasia. ARM can be used in anorectal malformation with defecation problems. ARM is used prior and after surgery to assess motor function [5]. In children having fecal incontinence with or without neurogenic problems, ARM is useful. ARM can be used to differentiate types of defecation dyssynergia in patients with chronic constipation. Assessment of rectal sensation is important in chronic constipation, megarectum and rectal hypersensitivity. In chronic constipation, rectal sensitivity threshold is increased [6] while in rectal hypersensitivity threshold is decreased. Rectal hypersensitivity is seen in patients with inflamed anorectum [7]. Rectal hypersensitivity also correlates with visceral hypersensitivity [8]. RAIR is present in patients with spinal cord lesions [9]. Sacral agenesis children have lower external anal squeeze pressure and increased rectal sensitivity threshold [10]. Children with spinal lesion can have anal spasm. They achieve maximum relaxation of sphincter with small inflation volumes [11]. Patients with internal anal sphincter achalasia can be assessed with ARM. Selected patients of anal achalasia may benefit from Botulinium toxin injection [12].
ARM can also be used in biofeedback therapy to teach children toilet training and manage defecation dyssynergia.
Test should be performed in left lateral position. International Anorectal Physiology Working Group [13] (IAPWG) recommends standardized testing protocol (Fig. 1) and the London classification for assessment of anorectal function. It starts with initial stabilization time of 3 minutes after catheter insertion. Resting pressures are evaluated later over 60 seconds. Short squeeze pressure of 5 seconds (3 in numbers) followed by long squeeze pressure of 30 seconds are suggested. It is emphasized that there should be 30-second interval between short squeeze and 60-second interval after long squeeze to assess cough reflex. After assessment of cough reflex, push for 15 seconds (3 in numbers) with interval of 30 seconds is assessed. Rectal sensory testing follows push assessment. In assessment of rectal sensation first constant sensation volume (FCSV), desire to defecate volume (DDV), and maximum tolerated volume are assessed. RAIR should be elicited at last. If megarectum is under evaluation more volume to elicit RAIR is required. Balloon expulsion testing is not validated in children. There is no published consensus on type of catheter volume required, balloon expansion with air or water in children [14].
Informed consent needs to be taken. Age-appropriate enema should be given. Rectum should be dis-impacted prior ARM.
Anal resting pressure [1] is mean maximum anal pressure over 60-second recording period. It assesses baseline anal sphincter integrity. High resting anal pressure suggest voluntary or involuntary muscle spasm, anal stenosis or anal stricture. Low resting anal pressure suggests hypotension, anal sphincter post drug assessment, post trauma or spinal cord disorder. According to London classification [13] high resting anal pressure is classified as minor anorectal finding. It is called as anal hypertension. While lower resting anal pressure is major anorectal finding called as anal hypotension. Recently published cohort study [15] in healthy infant’s normal resting pressure values at 2 months and 6 months are 62.9 cm of water (46.26 mmHg) and 65.3 cm of water (48.03 mmHg) respectively. Banasiuk et al. [16] have published the largest pediatric series of normal children biometrics from 1 to 18 years without lower gastro intestinal tract symptoms. According to this study normal resting pressure is 83±23 mmHg.
Squeeze pressure is the maximum incremental pressure observed during the assessment. Low squeeze pressure may mean poor understanding by child, neurogenic or myogenic anal sphincter injury. Squeeze pressure assess anal sphincter contractile integrity. The mean squeeze pressure in normal children is 191±64 mmHg [16]. Low anal squeeze pressure with low anal resting pressure is classified by London IAPWG [13] group as major anorectal finding of combined anal hypotension and hypocontractility. Low resting pressure with normal anal squeeze pressure is anal hypotension with normal contractility. Normal anal resting pressure with low anal squeeze pressure is anal norm tension with hypo contractility.
Push maneuver assess the coordination in defecation (Fig. 2). Adequate push pressure with high anal sphincter pressure is type I dyssynergia. Poor push with high anal sphincter pressure is type II dyssynergia. Adequate pressure with no decrease in anal sphincter pressure is type III dyssynergia. Poor push with no decrease in anal sphincter pressure is type IV dyssynergia. London IAPWG group classified these as disorders of recto anal coordination. Adequate rectal pressure and no decrease in anal pressure is defined as abnormal expulsion with dyssynergia. Poor rectal pressure with decrease in anal pressure is abnormal expulsion with poor propulsion. Poor rectal pressure with no decrease in anal pressure is abnormal expulsion with poor propulsion and dyssynergia. All these are labeled as minor findings as per London IAPWG group.
Defecation dyssynergia is of 4 types (Table 2). All these can present as constipation. It is present in about 81% of children who are diagnosed as functional constipation [17]. While in study of Banasiuk et al. [14] al 60% of patients with constipation have defecation dyssynergia. In both studies, type IV defecation dyssynergia is the most common disorder [14,17]. Adequate intrarectal pressure of more than 40 mmHg is normal [14]. Incomplete or absent relaxation of <20% of resting anal sphincter pressure is considered abnormal in push assessment. Study by Banasiuk et al. [14] suggested higher cut off 31% of anal relaxation in children. Defecation dyssynergia is also seen in patient with anorectal malformations. Isolated puborectalis contraction may contribute to this presentation [18].
Resting, squeeze, and push pressure (Fig. 3) are important in assessment of rectal incontinence or encopresis. Fecal incontinence can be constipation-associated fecal incontinence or nonretentive fecal in continence (NRFI). NRFI is more common in boys. They usually have normal formed stools, rarely painful defecation, no nocturnal encopresis and normal colonic transit time [19]. NRFI children have decreased resting pressure, reduced squeeze pressure and higher thresholds for sensation urge and discomfort [20,21]. Pressure at rest and squeeze in functional constipation with fecal incontinence are lower than functional constipation without incontinence [22]. Children with normal ARM with incontinence have lower response to therapy as compared to abnormal ARM [23].
Impaired cough reflex suggests damage to sacral arc [1]. Cough-anal reflex is described as contraction of external anal sphincter with coughing [24]. Afferent component of cough reflex comes from muscle spindles and other sensory receptors in pelvic floor muscles, ligament, fascia, and bladder [25]. Afferent is activated by increase in abdominal pressure during cough.
RAIR is tested by rapidly inflating rectal balloon with incremental volume ranging from 5–10 mL to 60 mL (Fig. 4). The reflex is considered present when decrease in resting pressure reaches 25%. The mean rectal balloon volume required to elicit RAIR [16] in children is 15.7±10.9 cm3. BSPGHAN, British Society of Pediatric Gastroenterology, Hepatology and Nutrition [1], suggests to start with 5 mL in infants and 10 mL in older children. There is usually incremental degree of anal sphincter relaxation with increasing balloon volume. Anticholinergic, glycopyrrolate may result in false positive absence of RAIR [26]. Ketamine does not affect the RAIR. Sevoflurane and chloral hydrate do not affect RAIR [26]. Positive RAIR excludes Hirschsprung disease (Fig. 4). Negative RAIR suggests Hirschsprung disease or internal anal sphincter achalasia. Partial RAIR [1] is seen in anorectal inflammatory condition.
The sensitivity of ARM and rectal suction biopsy is equivalent [27]. The specificity of ARM is lower than rectal biopsy. The negative predictive value of ARM [27] is 100% while positive predictive value of ARM is only 56%. Hence ARM can be used to exclude Hirschsprung disease. It may reduce the number of rectal suction biopsy. Functioning RAIR is decrease in anal sphincter pressure of at least 20 mmHg following balloon dilatation [27]. Postoperative RAIR is not seen till approximately 32 months in Hirschsprung disease and is associated with variable outcomes [28].
Anal sphincter relaxation integral at 10 seconds (ASRI 10) can be used as supportive metrics to RAIR to diagnose Hirschsprung disease. ASRI 10 <7 suggests Hirschsprung disease [29]. In London IAPWG group [13], absent RAIR is defined as recto anal areflexia. It is the major finding in ARM.
Rectal sensation is assessed by inflating air at 1 mL/sec. According to London IAPWG [13], FCSV, DDV, and maximum tolerable volume are calculated. More than 2 out of 3 abnormal tests (more than normal volume required to sense) is classified under major finding of rectal hyposensitivity. One out of 3 abnormal rectal sensory tests of more than normal volume required to trigger the sensation is classified as borderline rectal hyposensitivity. Even one abnormal rectal sensory test of less than normal volume required to trigger sensation is classified as rectal hypersensitivity. The FCSV [16] in normal children 24.4±23.98 cm3; DDV is 45.9±34.55 cm3; maximum tolerate volume 91.6±50.17 cm3. Common cutoff values are described in Table 3 for diagnosing anorectal dysmotility.
Age-appropriate mean first sensation volume [16] are 34, 25, 14.7, and 22.1 for <5 years, 5–8 years, 9–12 years, and >12 years, respectively. Age-appropriate mean DDV [16] are 36, 37.2, 36. and 55 for <5 years, 5–8 years, 9–12 years, and >12 years, respectively. Age-appropriate means maximum tolerable volume are 48, 75, 88, and 127 for <5 years, 5–8 years, 9–12 years, and >12 years, respectively. For children >12 years, adult values can be used [1].
Anorectal manometry is one of the most commonly asked motility test in children. The most common indication of anorectal manometry is to establish RAIR to rule out Hirschsprung disease. It is a safe procedure. Normal values for children are now available. Both solid state and water perfused catheter can be used for ARM. ARM can help in diagnosis of anorectal motor dysfunction. It can also be used in biofeedback therapy for treatment of defecation dyssynergia in children. More studies are needed before using advanced ARM – metrics in children. London IAPWG protocol should be followed in future studies for comparative analysis.
Fig. 1.
Stepwise analysis of anorectal biometrics based on London IAPWG (International Anorectal Physiology Working Group) [13] protocol. RAIR, recto anal inhibitory reflex.
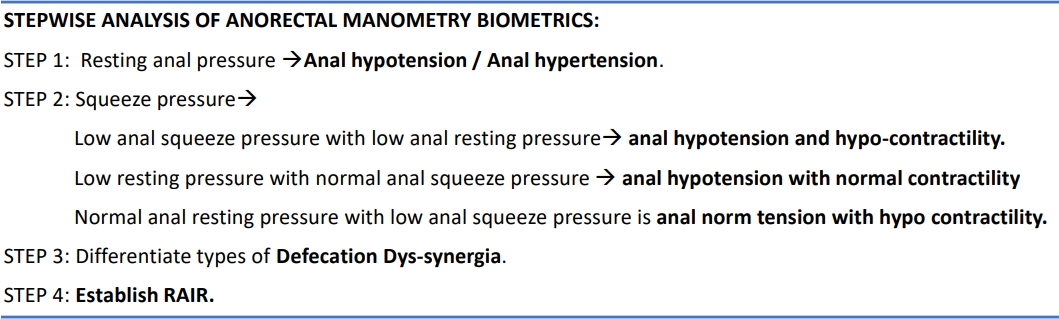
Fig. 2.
Anorectal manometry during push maneuver showing paradoxical raised anal pressure with defecation suggests type 1 defecation dyssynergia (Images taken post consent from patient and subject to copy right Superspeciality Clinics & Endoscopy Center. Nagpur. Dr Yogesh Waikar).
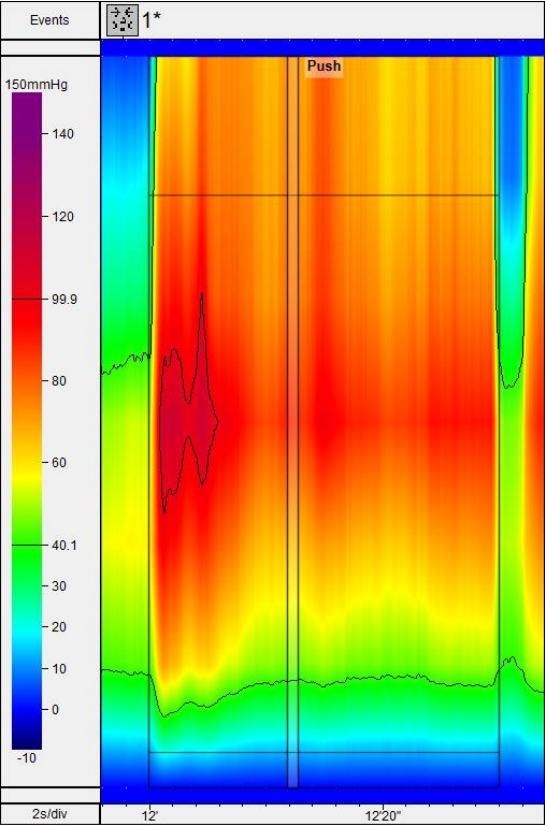
Fig. 3.
Anorectal manometry images during rest, squeeze, and push. It depicts normal topographical graph while performing anorectal manometry in 3 states which are rest, squeeze, and push. In squeeze, maneuver anal pressure increases (red-purple color in the middle). In push, maneuver rectal pressure increases showed by yellow and red lines in upper part of topographical chart. Images taken post consent from patient and subject to copyright Superspeciality Clinics & Endoscopy Center (Nagpur), Dr. Yogesh Waikar
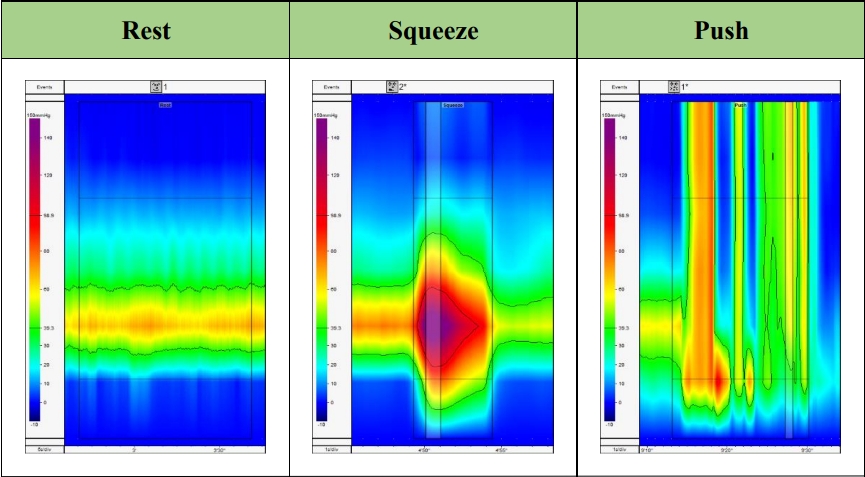
Fig. 4.
RAIR (recto anal inhibitory reflex) present rules out Hirschsprung disease. Reflex marked area shows reduction in anal pressure post rectal balloon inflation. Images taken post consent from patient and subject to copyright Superspeciality Clinics & Endoscopy Center (Nagpur), Dr. Yogesh Waikar.
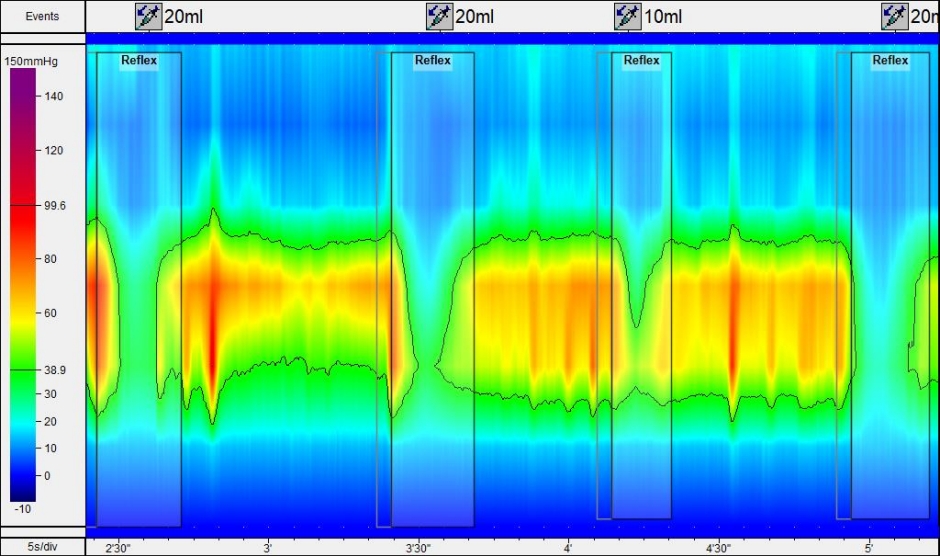
Table 1.
Indications of anorectal manometry in children
Table 2.
Types of defecation dyssynergia
| Type 1 defecation dyssynergia | Increase in intra-abdominal pressure (push) and paradoxical Increase in anal sphincter pressure (Fig. 2) |
| Type 2 defecation dyssynergia | No increase in intra-abdominal pressure (push) but with Paradoxical increase in anal sphincter pressure |
| Type 3 defecation dyssynergia | Increase in intra-abdominal pressure (push) with incomplete or absent less than 20% anal sphincter relaxation |
| Type 4 defecation dyssynergia | No increase in intra-abdominal pressure (push) & with incomplete or absent less than 20% anal sphincter relaxation |
Table 3.
Common cutoff used in anorectal biometrics
| Anorectal condition | Biometric | Value |
|---|---|---|
| Neonatal Anal hypotension [15] | Resting anal pressure | <46 mmHg |
| Pediatric anal hypotension [16] | Resting anal pressure | <63 mmHg |
| Anal hypocontractility [16] | Squeeze pressure | <127 mmHg |
| Incomplete anal relaxation [14,16] | Anal pressure on push | <20%–31% decrease in resting anal sphincter pressure on push |
| Impaired cough reflex [1] | No external anal sphincter contraction | Damage to sacral arc |
| RAIR present [1] | Resting anal pressure reduction | >25% decrease in resting anal pressure on inflation |
References
1. Athanasakos E, Cleeve S, Thapar N, Lindley K, Perring S, Cronin H, et al. Anorectal manometry in children with defecation disorders BSPGHAN Motility Working Group consensus statement. Neurogastroenterol Motil 2020;32:e13797.



2. Tran K, Kuo B, Zibaitis A, Bhattacharya S, Cote C, Belkind-Gerson J. Effect of propofol on anal sphincter pressure during anorectal manometry. J Pediatr Gastroenterol Nutr 2014;58:495–7.


3. Keshtgar AS, Choudhry MS, Kufeji D, Ward HC, Clayden GS. Anorectal manometry with and without ketamine for evaluation of defecation disorders in children. J Pediatr Surg 2015;50:438–43.


4. Yates G, Friedmacher F, Cleeve S, Athanasakos E. Anorectal manometry in pediatric settings: a systematic review of 227 studies. Neurogastroenterol Motil 2021;33:e14006.



5. Banasiuk M, Banaszkiewicz A, Piotrowski D, Albrecht P, Kamiński A, Radzikowski A. 3D high-definition manometry in evaluation of children after surgery for Hirschsprung's disease: a pilot study. Adv Med Sci 2016;61:18–22.


6. El-Shabrawi M, Hanafi HM, Abdelgawad MMAH, Hassanin F, Mahfouze AAA, Khalil AFM, et al. High-resolution anorectal manometry in children with functional constipation: a single-centre experience before and after treatment. Prz Gastroenterol 2018;13:305–12.



7. Arlander E, Löfberg R, Törkvist L, Lindforss U. Exploring anorectal manometry as a method to study the effect of locally administered ropivacaine in patients with ulcerative colitis. ISRN Gastroenterol 2013;2013:656921.




8. Simrén M, Törnblom H, Palsson OS, van Tilburg MAL, Van Oudenhove L, Tack J, et al. Visceral hypersensitivity is associated with GI symptom severity in functional GI disorders: consistent findings from five different patient cohorts. Gut 2018;67:255–62.


9. Rodriguez L, Sood M, Di Lorenzo C, Saps M. An ANMS-NASPGHAN consensus document on anorectal and colonic manometry in children. Neurogastroenterol Motil 2017;Jan;29(1): doi: 10.1111/nmo.12944. [Epub].
10. Morera C, Nurko S. Rectal manometry in patients with isolated sacral agenesis. J Pediatr Gastroenterol Nutr 2003;37:47–52.


11. Siddiqui A, Rosen R, Nurko S. Anorectal manometry may identify children with spinal cord lesions. J Pediatr Gastroenterol Nutr 2011;53:507–11.


12. Koivusalo AI, Pakarinen MP, Rintala RJ. Botox injection treatment for anal outlet obstruction in patients with internal anal sphincter achalasia and Hirschsprung's disease. Pediatr Surg Int 2009;25:873–6.



13. Carrington EV, Heinrich H, Knowles CH, Fox M, Rao S, Altomare DF, et al. The international anorectal physiology working group (IAPWG) recommendations: standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil 2020;32:e13679.




14. Banasiuk M, Dobrowolska M, Skowronska B, Konys J, Chorazyk A, Szudejko E, et al. Three-dimensional high-resolution anorectal manometry: cut-off values for diagnosis of dyssynergic defecation in children. Eur Rev Med Pharmacol Sci 2021;25:5199–207.

15. Gatzinsky C, Redfors S, Borg H, Linnér C, Sillén U, Sjöström S. High-resolution anorectal manometry-a prospective cohort study in healthy infants. J Pediatr Gastroenterol Nutr 2022;74:e57–64.


16. Banasiuk M, Banaszkiewicz A, Dziekiewicz M, Załęski A, Albrecht P. Values from three-dimensional high-resolution anorectal manometry analysis of children without lower gastrointestinal symptoms. Clin Gastroenterol Hepatol 2016;14:993–1000.e3.


17. Makosiej R, Makosiej A, Bossowski A, Kolejwa M, Wawrusiewicz-Kurylonek N, Łęgowik A, et al. Dyssynergic defecation and anal sphincter disorders in children in high-resolution anorectal manometry investigation. J Pediatr Gastroenterol Nutr 2020;71:484–90.


18. Bjørsum-Meyer T, Christensen P, Baatrup G, Jakobsen MS, Asmussen J, Qvist N. Dyssynergic patterns of defecation in constipated adolescents and young adults with anorectal malformations. Sci Rep 2020;10:19673.


19. Rajindrajith S, Devanarayana NM, Thapar N, Benninga MA. Functional fecal incontinence in children: epidemiology, pathophysiology, evaluation, and management. J Pediatr Gastroenterol Nutr 2021;72:794–801.


20. Banasiuk M, Dziekiewicz M, Dembiński Ł, Piotrowski D, Kamiński A, Banaszkiewicz A. Three-dimensional high-resolution anorectal manometry in children after surgery for anorectal disorders. Eur Rev Med Pharmacol Sci 2021;25:2981–93.


21. Banasiuk M, Dziekiewicz M, Dobrowolska M, Skowrońska B, Dembiński Ł, Banaszkiewicz A. Three-dimensional high-resolution anorectal manometry in children with non-retentive fecal incontinence. J Neurogastroenterol Motil 2022;28:303–11.



22. Alessandrella A, Turco R, Russo M, Poziello A, Miele E, Staiano A. High-resolution anorectal manometry in children with functional constipation with or without fecal incontinence. Neurogastroenterol Motil 2020;32:e13882.



23. Morera C, Nurko S, Rodriguez L. Evaluation of fecal incontinence in pediatric functional constipation: clinical utility of anorectal and colon manometry. J Pediatr Gastroenterol Nutr 2021;72:361–5.


24. Meagher AP, Lubowski DZ, King DW. The cough response of the anal sphincter. Int J Colorectal Dis 1993;8:217–9.



25. Chan CL, Ponsford S, Swash M. The anal reflex elicited by cough and sniff: validation of a neglected clinical sign. J Neurol Neurosurg Psychiatry 2004;75:1449–51.


26. Pfefferkorn MD, Croffie JM, Corkins MR, Gupta SK, Fitzgerald JF. Impact of sedation and anesthesia on the rectoanal inhibitory reflex in children. J Pediatr Gastroenterol Nutr 2004;38:324–7.


27. Meinds RJ, Trzpis M, Broens PMA. Anorectal manometry may reduce the number of rectal suction biopsy procedures needed to diagnose hirschsprung disease. J Pediatr Gastroenterol Nutr 2018;67:322–7.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


