Introduction
Since December 2019, as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) became a pandemic, the number of pregnant women infected with SARS-CoV-2 also increased [
1]. Some studies raised concerns regarding the possibility of vertical transmission while others reported that the risk is almost negligible [
2-
5]. There are limited analyses regarding coronavirus disease 2019 (COVID-19) on maternal and neonatal clinical features but outcomes are unclear [
6-
8]. Korean guidelines recommend the isolation of neonates either in a negative pressure room or in a private room at the neonatal intensive care unit (NICU) when negative pressure rooms are unavailable [
9]. However, this policy delays mother-infant bonding and makes breastfeeding difficult. The Centers for Disease Control and Prevention (CDC) and the World Health Organization recommend rooming-in for breastfeeding with no need for separation of mothers and neonates [
10,
11]. A few studies have reported adverse neonatal outcomes of COVID-19 infected mothers; however, these associations are still unclear [
7,
8,
12]. Currently, limited data with small sample sizes are available regarding the risk of perinatal infection and neonatal outcomes of infants born to COVID-19 infected mothers in Korea [
1,
13,
14]. A recent Korean National Mother-Child Cohort study on neonatal outcomes discovered a possible association of COVID-19 mothers with increased NICU admission [
15]. However, this association is not clear since the isolation policy may have affected admission. Moreover, the detailed clinical respiratory outcome was not presented in the data.
This study aimed to compare the clinical outcomes of neonates born to mothers who had COVID-19 during pregnancy with those born to mothers who did not. In addition, by providing information on the clinical outcomes of newborns, we seek to secure a basis for re-examining the current national neonatal infection response guidelines for COVID-19.
Methods
1. Setting and guidelines for COVID-19 quarantine
The management of neonates born to mothers with confirmed COVID-19 follows the guidelines for COVID-19 by the Korean Society of Pediatric Infectious Disease and the Korean CDC [
9]. At the time of delivery, amniotic fluid, and umbilical cord blood are obtained to conduct laboratory testing for SARS-CoV-2. The neonate is isolated in a single room under negative pressure at the NICU. Healthcare workers wear KF94 masks, surgical caps, face shields, gloves, and gowns. If the second SARS-CoV polymerase chain reaction (PCR) test obtained from the oropharyngeal/nasopharyngeal (OP/NP) swab at 24 and 48 hours after birth is negative, the quarantine of the neonate is discontinued. The neonate is isolated from the mother until the mother is released from quarantine. As expected, breastfeeding is impossible when mothers are quarantined. However, direct breastfeeding is recommended after quarantine.
2. Study population
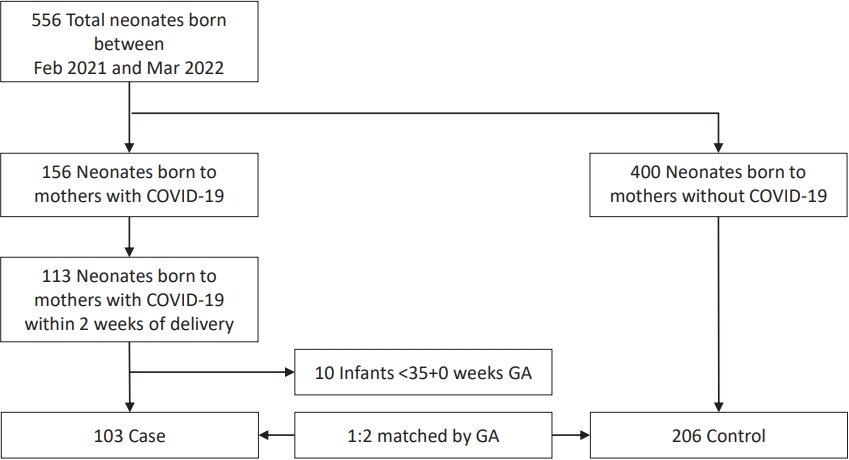
This single-center retrospective study was conducted in neonates born to mothers with COVID-19 from February 2021 to March 2022 at the National Health Insurance Service (NHIS) Ilsan Hospital, a COVID-19 designated hospital. A total of 556 neonates were born during this period, with 156 born to mothers with COVID-19 (
Fig. 1). Among the 156 neonates, 113 were born to mothers with COVID-19 within 2 weeks of delivery. For the 1:2 matched case-control analysis, neonates under 35 weeks gestational age (GA) were excluded, and 103 neonates born to infected mothers were assigned to the case group and 206 to the control group. The control group comprised neonates with matched GA born to mothers without COVID-19 at NHIS Ilsan Hospital during the same period. COVID-19 was confirmed by a positive result in the OP/NP swab reverse transcription quantitative real-time PCR (RT-PCR).
3. Study variables
The following data were collected from the NHIS Ilsan Hospital's electronic medical record database: maternal information including age, nationality, obstetric problems (hypertension and gestational diabetes mellitus [GDM], fetal distress, preterm labor, premature rupture of membranes [PROMs]), duration of fetal exposure to COVID-19 infection, mode of delivery, symptoms associated with COVID-19, use of respiratory support, SARS-CoV-2 PCR from OP/NP swabs, umbilical cord blood, amniotic fluid, and breast milk, and serum antibody IgG/M; neonatal information, including GA, birth weight, sex, plurality, Apgar score, SARS-CoV-2 PCR from OP/NP swabs and blood, and serum antibody IgG/M.
Maternal symptoms were defined as fever (≥37.5°C), cough, sputum, sore throat, shortness of breath, and anosmia. Maternal pneumonia was defined as radiographic confirmation by radiologists. Small-for-gestational-age (SGA) was defined as less than 10 percentile on the 2013 Fenton Preterm Growth Chart [
16].
Maternal and neonatal samples were tested for SARS-CoV-2 PCR using STANDARD M nCoV Real-Time Detection kit (SD BIOSENSOR Inc., Suwon, Korea) and for serum antibody IgG/M using STANDARD Q COVID-19 IgM/IgG Plus Test (SD BIOSENSOR Inc.) at the NHIS Ilsan Hospital laboratory.
4. Neonatal clinical outcomes
The neonatal outcomes include the length of hospital stay, respiratory diseases (respiratory distress syndrome [RDS], transient tachypnea of the newborn [TTN], and meconium aspiration syndrome [MAS]), and respiratory support (supplemental oxygen, noninvasive respiratory ventilation, and invasive ventilation).
RDS was defined as respiratory difficulties confirmed by chest radiography and the need for surfactant treatment. MAS was defined as a history of meconium staining and symptoms of respiratory difficulties requiring respiratory support, with abnormal chest radiograph findings. TTN was defined as symptoms of respiratory difficulties with tachypnea (>60 breaths per minute), grunting, and chest retractions, along with abnormal chest radiographic findings indicating retained lung fluid, excluding other respiratory diseases like RDS, congenital pneumonia, or meconium aspiration.
Invasive ventilation includes conventional ventilation or high-frequency oscillatory ventilation with tracheal intubation. Noninvasive ventilation includes humidified high-flow nasal cannula (HFNC), nasal continuous positive airway pressure, or synchronized nasal intermittent positive pressure ventilation. A HFNC was defined as a flow rate of >2 L/min. Oxygen therapy was defined as the use of oxygen through a nasal prong, mask, hood, or incubator.
A period of use of invasive or noninvasive ventilation counts as a day regardless of the number of hours used, and a period of use of oxygen use counts as a day if it is used for 8 or more consecutive hours.
5. Covariates
To determine the association between maternal COVID-19 infection and neonatal respiratory outcomes, we included maternal age, obstetric complications (hypertension and GDM), mode of delivery, birth weight, sex, and SGA as covariates.
6. Statistical analysis
All statistical analyses were performed using the SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA). Categorical variables were expressed as numbers (%) and continuous variables were expressed as the mean±standard deviation. Statistical significance was set at P<0.05. GA was used as a 1:2 matching variable using propensity score matching.
To compare the differences in clinical outcomes between the 2 groups, the chi-square test and Fisher exact test were used for categorical variables, and the independent 2-sample t test and paired t test were used for continuous variables.
The odds ratio (OR) and 95% confidence interval (CI) were estimated using a logistic regression model to analyze the associations between the independent variables and neonatal respiratory outcomes.
7. Ethics statement
This study was approved by the Institutional Review Board (IRB) of National Health Insurance Service Ilsan Hospital (IRB approval number: 2022-03-018-001).
Discussion
The NHIS Ilsan Hospital, a designated COVID-19 hospital, has the most experience in delivering infected mothers with COVID-19 in Korea. To our knowledge, this single-center study included the largest Korean cohort of neonates born to mothers with COVID-19. Among the 113 neonates born to 106 mothers with COVID-19, none tested positive for SARS-CoV-2; however, adverse outcomes with an increased risk of TTN were associated with maternal COVID-19 infection.
In a previous systematic review of 201 neonates, 4 (2.4%) were reported to have confirmed SARS-CoV-2 infection during the first 48 hours of life [
6]. In a retrospective cohort analysis conducted at a single center in New York, 2 of 101 neonates had indeterminate test results for SARS-CoV-2 nasopharyngeal swabs [
17]. There was no evidence of vertical or antenatal transmission of SARS-CoV-2 infection in our study, as many previous articles have shown [
2,
3].
Several studies have revealed that maternal COVID-19 infection increases the risk of adverse neonatal outcomes, but these associations remain unclear [
6,
7,
18]. This largest single-center study in Korea is comparable to a nationwide cohort study in Sweden [
7], in which 2,323 infants delivered by SARs-CoV-2 positive mothers exhibited a significant association with admission to the neonatal unit (OR, 1.47), RDS (OR, 2.4), any respiratory disorder (OR, 1.42), and hyperbilirubinemia (OR, 1.47) after matching for maternal characteristics [
7]. In England, another national cohort study restricted to full-term pregnancies (GA ≥37 weeks) reported no significant differences in neonatal adverse outcomes but a higher likelihood of longer postnatal hospital stay (21.1% compared with 12.6%; AOR, 1.61) [
8]. A recent Korean multicenter retrospective cohort study conducted in 15 hospitals included 62 newborns [
1]. They focused on the findings that the severity of the disease in pregnant women infected with SARS-CoV-2 did not affect neonatal outcomes [
1]. Our study highlighted the short-term neonatal respiratory outcomes of mothers with COVID-19. A 1:2 case-control matched analysis showed significant differences between the 2 groups in the length of stay (
P=0.020), TTN (
P<0.001), use of noninvasive ventilation (
P=0.040), and oxygen supplement (
P=0.022).
Over 91% of the study group underwent C-section. As we know, C-section has the potential to increase the risk of TTN, and infants delivered by planned C-section without labor are more likely to develop respiratory distress [
19]. At our institution, elective cesarean delivery was preferred due to strong infection control restrictions. During the early era of the epidemic in China, C-sections were performed to reduce the risk of intrapartum transmission. A meta-analysis of 1,100 pregnancies, reported a high cesarean rate of 85% [
20]. Severity of maternal infection may increase obstetric decisions to deliver, but with the low vertical transmission rate, there is no need for an elective C-section because of COVID-19 itself. Because cesarean deliveries are associated with increased neonatal morbidity, the decision to deliver by C-section should be carefully considered [
21].
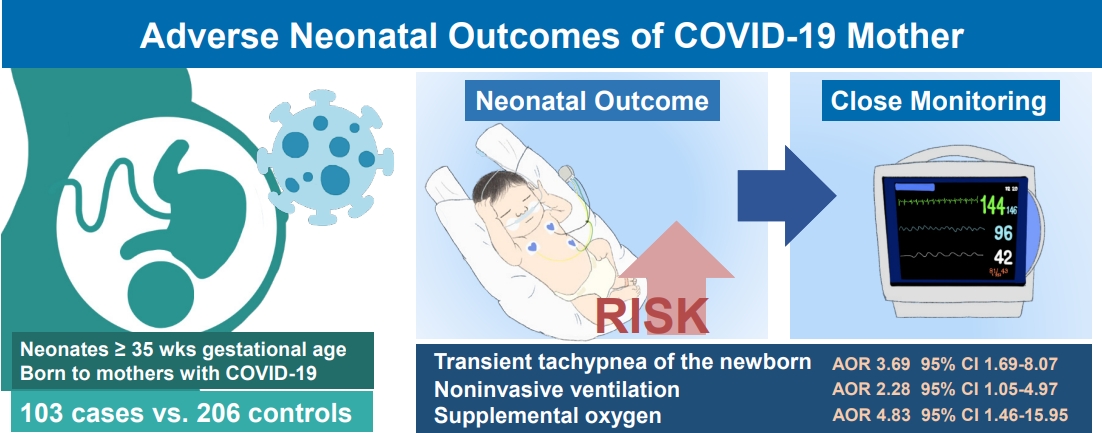
Our study found that maternal COVID-19 infection was still associated with a higher risk of TTN after controlling for other factors that may affect neonatal outcomes, including C-section. The multivariate regression analysis showed that neonates of mothers with COVID-19 were 3.69 times more likely to have TTN, 2.28 times more likely to use noninvasive ventilation, and 4.83 times more likely to require oxygen supplementation than neonates of mothers without COVID-19. Given the possibility of an increase incidence of respiratory symptoms, close monitoring of these neonates is recommended.
A possible mechanism for increased respiratory distress in infants born to SARS-CoV-2 infected mother is related to altered levels of proinflammatory cytokines in pregnant women infected with SARS-CoV-2 [
22]. Zhu et al. [
23] reported a high prevalence of respiratory distress among clinical symptoms in neonates born to mothers with COVID-19, which is attributed to the findings that elevated maternal concentrations of cytokines, such as interleukin-6, interleukin-1β, and tumor necrosis factor-alpha affect fetal development resulting in abnormalities, including bronchopulmonary dysplasia and brain damage. Potential adverse effects on newborns of SARS-CoV-2 infected mothers with hypoxemia and immunopathogenesis need to be examined further.
A previous prospective cohort study and systematic review reported that maternal COVID-19 infection may be associated with a high prevalence of preterm birth [
24,
25]. A retrospective case-control study in China found a significantly higher preterm birth rate (22.2%) in neonates born to mothers with COVID-19 than in the control group [
18]. In a cohort of 255 neonates from 11 hospitals in Massachusetts, worsening of maternal illness led to preterm delivery and caused adverse outcome of infants [
12]. In our study cohort, 3.9% were born with low birth weight, and 11.7% were born prematurely. All included pregnant women were in the third trimester and diagnosed within 2 weeks before delivery; therefore, COVID-19 infection affecting prematurity or intrauterine growth retardation could not be evaluated in this study. As our study cohort mainly comprised late preterm or full-term neonates (91 out of 103 infants were born at 37 weeks or more GA), we did not examine the association of preterm risks.
The CDC recommend COVID-19 vaccination at any point during pregnancy [
26]. In Korea, COVID-19 vaccination was initiated on October 18, 2020, but the vaccination rate was poor among pregnant women due to a lack of consensus. Only 12.1% of COVID-19 positive mothers were vaccinated, which was too small to observe a significant effect on maternal disease severity.
Maternal IgG antibodies to SARS-CoV-2 (including neutralizing anti-SARS-CoV-2 adaptive antibodies) are known to cross the placenta after infection with COVID-19 during pregnancy, with or without symptoms [
27,
28]. It has been reported that infection occurring more than 2 months prior to delivery enables efficient transfer of maternal SARS-CoV-2 IgG across the placenta in a prospective observational study [
29], but the efficiency between the timing of maternal SARS-CoV-2 and the transfer of immunity across the placenta remains unclear. Antibody tests were performed in 87 mothers and 101 infants. Due to recent (≤2 weeks of delivery) infection in the mother, IgG antibodies were detected at birth in only 15 of 101 infants and 27 of 87 mothers. The protective effect of maternal antibodies crossing the placenta in newborns requires further research based on accumulated data.
The strict isolation policy implemented at our institution may not be generalizable. Mothers were under a stringent policy in which the neonate was isolated from the mother until the mother was free from quarantine, which ranged from 10 to 7 days according to updated guidelines. Increased hospital days in the study group do not necessarily represent the actual clinical severity of infants, as the majority of NICU admissions were done as a precautionary measure to closely monitor the neonatal condition or to isolate the infant until the PCR result was confirmed negative. Hospital days was also influenced by their mothers’ discharge plans.
Moreover, according to the hospital isolation policy, expressed milk was not allowed to leave the isolation room, and all items in the isolation room had to be discarded. Temporary separation may be inevitable for mothers when symptoms are severe; however, the benefits of breastfeeding and mother-infant contact should be considered when implementing guidelines. In a retrospective cohort study at a single center in New York, no clinical evidence of perinatal transmission was identified, despite most newborns rooming-in and directly breastfeeding [
17]. In a nationwide study by the Spanish Society of Neonatology Registry, skin-to-skin contact after delivery, rooming-in with the mother, and breastfeeding have been documented in a high proportion of neonates without adverse events [
30]. Our data of zero detection of SARS-CoV-2 RNA in breast milk adds to the current suggestion that transmission of SARS-CoV-2 via breast milk is unlikely. We highly recommend breastfeeding after discharge, and it was confirmed that 57.8% of patients were breastfeeding at the one-month outpatient follow-up.
The long-term outcomes in neonates born to mothers with COVID-19 remain unknown. A recent cohort study of 18,355 offspring with SARS-CoV-2 exposure in utero, showed that infants may be at higher risk for neurodevelopmental disorders at 12 months of age [
31]. In addition to SARS-CoV-2, several reports have suggested that activation of maternal immunity due to exposure to other microbial infections in utero, may have long-term effects on the development of offspring [
32,
33].
SARS-CoV-2 recognizes and binds to the angiotensin-converting enzyme 2 (ACE2) receptor, causing severe hypoxemia. In pregnant women with SARS-CoV-2 infection, ACE2 insufficiency and placental hypoxia can have adverse effects on mothers and their fetuses [
34]. Several studies have shown that pregnant women have more susceptibility to severe illness from SARS-CoV-2 infection than non-pregnant women [
22,
33]. Therefore, pregnancy and perinatal complications, including preeclampsia, fetal death, preterm birth, intrauterine growth retardation, and respiratory distress, are likely to occur in SARS-CoV-2 infected mothers and their newborns [
34].
Through the placental pathology of SARS-CoV-2 infected pregnant women, it was confirmed that viral infection caused a variety of placental conditions, such as increases in intervillous or subvillous fibrin, thrombi in vessels, and multifocal infarctions [
34,
35]. In our study, 14 placental pathologies were reviewed, 8 of which showed intervillous infarction or thrombus presenting with hypoxia. Clinical fetal distress was not observed in our study; however, a larger sample size is required to establish an association between placental pathology and perinatal complications or long-term risks.
Matching the control group by GA to assess the risk of late preterm or term infants born to mothers with COVID-19 was a strength of this study. However, this study has some limitations. First, our results span the eras of alpha and delta variants to the omicron variant of SARS-CoV-2; but we did not examine differences between the variants. Second, the findings of our study may not be generalizable, as it was a single-center study. Thirdly, there may be a subjective bias for infants born to mothers with COVID-19 with respiratory symptoms. Finally, since the participants in our study were infected mothers within 2 weeks of delivery and newborns over 35 weeks of GA, we could not determine how SARS-CoV-2 infection in the first and second trimesters affects newborns. Further large multicenter research on the effect of maternal COVID-19 infection including long-term outcomes of neonates, is needed.
In conclusion, our study shows the possibility of an increase in the incidence of TTN in neonates born to mothers infected with COVID-19, close monitoring for respiratory symptoms after delivery is recommended.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


