Article Contents
| Clin Exp Pediatr > Volume 67(1); 2024 |
|
Abstract
Background
The use of helmet treatment for positional plagiocephaly has increased recently; however, its effect is unknown in Korea.
Purpose
This study aimed to investigate the effectiveness of helmet therapy and identify its influencing factors.
Methods
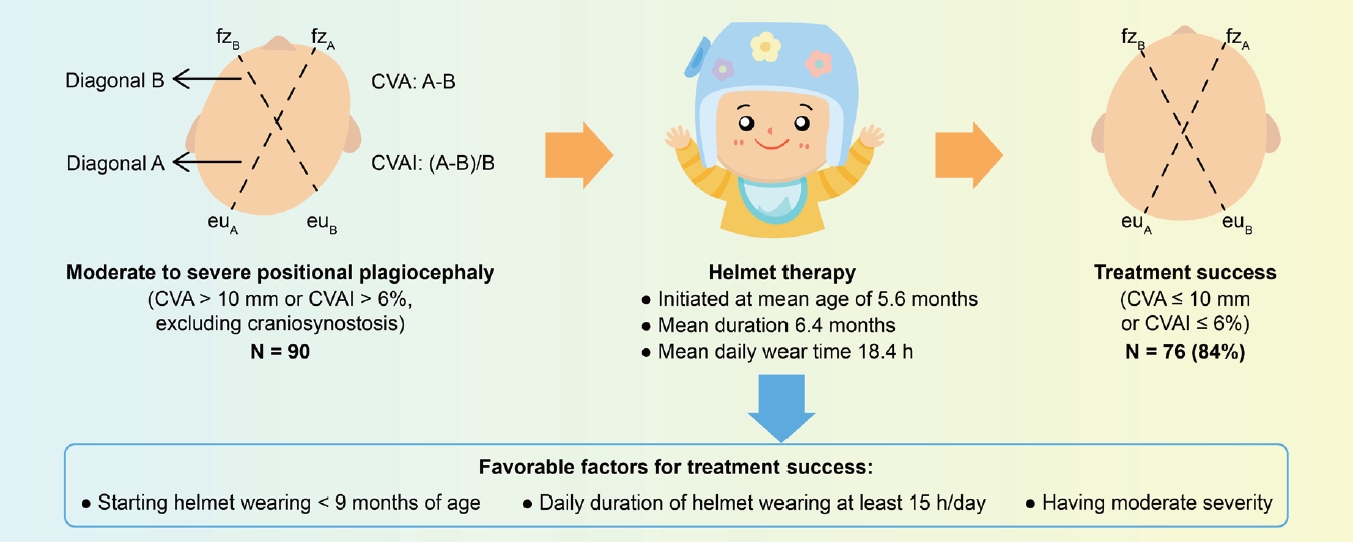
Ninety pediatric patients diagnosed with moderate to severe positional plagiocephaly received helmet therapy. Severity of moderate to severe positional plagiocephaly was defined as cranial vault asymmetry (CVA) >10 mm or CVA index (CVAI) >6%. Patients were categorized by age, severity, and daily helmet wear. Multiple regression analysis controlled for factors like sex and prematurity. Treatment success was assessed by comparing pre/post-helmet theray CVA and CVAI, considering normalization or decrease to mild plagiocephaly (CVA ≤10 mm or CVAI ≤6%).
Results
A total of 90 participants were enrolled (mean age, 5.6±1.6 months; male, 53 [58.9%]). The mean helmet therapy duration was 6.4±2.7 months, while the mean daily wear time was 18.4±2.7 hours. Among the 90 patients, 66 (73.3%) had moderate disease and 24 (26.7%) had severe disease. The mean CVA and CVAI decreased by 6.3±2.7 mm and 4.3%±1.8% after versus before treatment (P<0.001). Treatment was successful in 76 infants (84.4%). The most effective changes in CVA and CVAI were noted in those who began treatment before 9 months of age (6.2±2.5 mm and 5.0%±1.9%, P<0.001), had high compliance (6.2±2.4 mm and 4.9%±1.9%, P<0.001), and had high severity (8.0±2.3 mm and 6.6%±1.7%, P<0.001).
Graphical abstract. CVA, cranial vault asymmetry; CVAI, CVA index.
Positional plagiocephaly, also known as deformational plagiocephaly, is a condition where the skull becomes asymmetrically deformed because of external pressure, without craniosynostosis [1]. The condition may have both prenatal and postnatal causes, but is most commonly associated with infants spending extended periods in the supine position [2,3]. Severe flattening of the posterior region of the head is often accompanied by ipsilateral frontal bossing and anterior displacement of the ear (Fig. 1A). While repositioning therapy can be an effective treatment for infants under 4 months of age, helmet therapy may be considered if the deformity is severe or if repositioning is unsuccessful, after ruling out other conditions such as lambdoid synostosis (Fig. 1B) [4,5]. The effectiveness of helmet therapy is controversial, with some studies reporting significant improvement and others finding no clinically meaningful difference [6-8]. While skull deformation is commonly perceived as a cosmetic issue, studies have suggested an association between infants with positional plagiocephaly and various health concerns, such as delays in psychomotor development, jaw asymmetry, and low self-esteem [9,10]. Therefore, parents have become increasingly attentive to their infants' head shape, leading to a surge in pediatrician visits [11,12]. However, few studies have investigated the treatment of positional plagiocephaly, and there is limited evidence regarding the effectiveness of helmet therapy for infants with this condition. Therefore, the treatment for positional plagiocephaly primarily depends on clinical experience and varies greatly [6,13]. The lack of consensus among medical professionals regarding treatment options can create uncertainty for parents. This study aimed to evaluate the effectiveness of helmet therapy in infants with moderate to severe positional plagiocephaly, while also examing the influence of different initiation ages, degree of head asymmetry and daily duration of helmet wear on treatment outcomes.
This study was conducted on 90 infants with moderate to severe positional plagiocephaly who received helmet therapy between May 2018 and April 2021. Infants with mild positional plagiocephaly, craniosynostosis, congenital muscular torticollis, brachycephaly, and other congenital anomalies were excluded. Prior to helmet therapy, all infants underwent skull radiography to exclude cranial suture synostosis.
The severity of positional plagiocephaly is evaluated by measuring cranial vault asymmetry (CVA) and the CVA index (CVAI) [6,14]. CVAI facilitates a direct comparison of cranial deformities in infants with varying head sizes.
The distances between the lateral point of the ipsilateral eyebrow and the contralateral occiput were measured to calculate the CVA and CVAI. The CVA is defined as the diagonal difference obtained by subtracting the shorter cranial diagonal from the longer cranial diagonal while the CVAI is defined as CVA divided by the smaller diagonal and multiplied by 100 (Fig. 2B). In this study, the severity of plagiocephaly was defined according to the following criteria based on previous reports: normal, CVA <5 mm or CVAI <3.5%; mild, 5–10 mm or 3.5%–6%; moderate, >10–≤15 mm or >6%–≤10%; and severe, >15 mm or >10% [12,15].
Helmet therapy was initiated based on the infant's initial CVA measurement of greater than 10 mm and CVAI greater than 6%. Head deformity was evaluated using anthropometric measurements taken with a sliding caliper (Fig. 2A) and a 3-dimensional surface scanner (WillowWood Global LLC, OMEGA Scanner, Mt. Sterling, OH, USA) (Fig. 3).
The helmets utilized in the study were designed and produced by Hanuri Health Care Company (Daegu, Korea) and were customized to fit the patient's specific head condition. The helmet is typically recommended to be worn for 23 hours a day, following a break-in period of 7–14 days. Calibration of the helmet is performed every 4–8 weeks when in use. From the initial diagnosis in the physician's office to when the helmet will be put on, the process generally takes approximately 2 weeks (Fig. 4).
Based on their age at the initiation of helmet therapy, patients were grouped as follows: groups 1 (5 months or younger, n=39), group 2 (5–7 months, n=37), group 3 (7–9 months, n=11), and group 4 (over 9 months, n=3).
In addition,the severity of head asymmetry was classified as moderate (CVA >10–≤ 15 mm or CVAI >6%–≤10%, n=66) or severe (CVA >15 mm or CVAI >10%, n=24), based on the initial CVA and CVAI. Patients' compliance was classified as excellent (≥20 hours, n=1), good (15–19 hours, n=85), or poor (<15 hours, n=4), based on the amount of time per day the helmet was worn, as reported by the patient's parents. The treatment effectiveness was evaluated by comparing CVA and CVAI measurements taken before and after helmet therapy. Helmet therapy was discontinued when CVA or CVAI decreased to less than10 mm or 6%, which was defined as a successful treatment.
IBM SPSS Statistics ver. 26.0 (IBM Co., Armonk, NY, USA) was used for data analysis. To compare the treatment effects of each group, paired sample t-tests and Fisher exact test were used, with statistical significance set at P<0.05. Furthermore, a 1-way analysis of variance was performed to examine the correlation between treatment effect and helmet-wearing time, with a significance level of P<0.05. To examine the impact of these key variables on the changes in CVA and CVAI following helmet therapy, multiple linear regression analysis was conducted. Gender and prematurity were entered as control variables.
This study investigated 90 infants who completed helmet treatment after being diagnosed with moderate to severe positional plagiocephaly. Of the participants, 53 were male (58.9%) and 37 were female (41.1%). The infants began treatment at a mean age of 5.6±1.6 months and had initial mean values of 12.4±2.6 mm and 9.1%±2.1% for CVA and CVAI, respectively. On average, they wore the helmet for 6.4±2.7 months, for an average of 18.4±2.7 hours per day (Table 1).
After completing the helmet therapy, the final mean of CVA and CVAI were 6.3±2.7 mm and 4.3%±1.8%, respectively. This represented an improvement of approximately 50% from their initial values, and the difference was statistically significant (P<0.001) (Table 2).
The patients were assigned to 4 groups based on their age during the initiation of helmet therapy, and the CVA differences between the groups before and after helmet therapy were as follows: 7.0 mm (group 1), 5.6 mm (group 2), 5.3 mm (group 3), and 2.7 mm (group 4). The CVAI differences were 5.7% (group 1), 4.4% (group 2), 4.1% (group 3), and 2.0% (group 4). The change in CVA and CVAI was found to be the highest in group 1 (P<0.001 and the lowest in group 4 (P=0.003), indicating that the treatment effect was more significant in younger patients (Table 3).
Overall, 66 infants (73.3%) were classified as having moderate plagiocephaly, with the remaining 24 (26.7%) classified as severe. Normal range of the head shape was observed in 40.9% of the moderate group and 8.3% of the severe group. However, 60 infants (90.9%) of the moderate group and 16 (66.7%) of the severe group exhibited successful therapeutic effects (CVA ≤10 mm or CVAI ≤6%). The change in CVA/CVAI was greater in the severe group (8.0 mm/6.6%) than in the moderate group (5.4 mm/4.2%), with treatment periods of 7.9 and 5.8 months, respectively (Table 4).
The patients were also assigned to three compliance groups based on their helmet-wearing time, with the group wearing the helmet for more than 15 hours per day showing the most significant improvement in CVA/CVAI (6.2 mm/4.9%). Poor compliance resulted in a smaller improvement of 3.2 mm/2.9%. These findings suggest that the effectiveness of helmet therapy is related to the duration of wearing the helmet, especially if it exceeds 15 hours per day (Table 5).
An analysis was conducted on the effects of starting age (age at which helmet therapy began), compliance (daily duration of helmet wear), and risk status (based on CVA threshold of 15 mm or CVAI threshold of 10%) on the changes in CVA and CVAI following helmet therapy. After controlling for sex and prematurity, the age at which helmet therapy was started, daily wear duration, and severe initial conditions had statistically significant effects on the rate of change in CVA/CVAIthrough helmet therapy (Table 6).
Helmet therapy was shown to be an effective tool for infants with moderate to severe positional plagiocephaly. Better treatment outcomes were achieved when the treatment was started earlier than 9 months of age and the helmet was worn for more than 15 hours per day.
Positional plagiocephaly is a condition where an infant's head becomes flattened in one area because of prolonged pressure on that area of the skull. This can occur when infants spend a lot of time lying on their backs, in a car seat, or in a rocker. The incidence of positional plagiocephaly increased after the American Academy of Pediatrics initiated the "Back to Sleep" campaign in 1992, which advised parents to avoid putting infants in a prone position while sleeping to decrease the occurrence of sudden infant death syndrome [14]. Prior to the campaign, instances of positional plagiocephaly occurred in 1:300 infants, whereas after the campaign, instances increased to 1:60 infants [15,16].
Early physical and repositioning therapy is highly effective in correcting positional plagiocephaly if it is detected at an early age (within 4 months of age) [17]. Repositioning therapy typically entails maintaining an infant's head in a preferred position, while parents are counseled to enhance supervised tummy time and limit time spent in car seats and rockers [18]. In milder cases, where the diagnosis is made early, cranial deformation can be managed by stretching exercises and a regular prone position.In most severe cases, the use of a helmet may be necessary (Fig. 5) [8,12,19]. The objective of helmet therapy is to reposition the developing skull in regions where it has become flattened [20]. During the first year of life, the infant’s skull grows rapidly; thus, early intervention is considered important for more successful treatment of skull deformation [8,21]. Since it was first introduced by Clarren et al., helmet therapy has been widely applied [22,23]. Many studies have examined the effectiveness of helmet therapy; however, no definite conclusions have been reported [9,15,24,25]. In 2014, van Wijk et al. studied 84 infants and reported no differences in the change score of skull deformity between helmet therapy and natural course groups [6]. In 2015, Rowland and Das [13] conducted a study that compared the helmet therapy and no-intervention groups comprising 84 infants with moderate to severe positional plagiocephaly. They reported that improvement in skull shape was almost the same in the helmet therapy and control groups. Despite some disagreement, most studies reported that helmet therapy is effective in improving and preventing the progression of positional plagiocephaly [9-12]. According to recent reports, the effectiveness of helmet therapy is influenced primarily by the age at which the therapy is initiated and the severity of the asymmetry [19,20,26]. Moreover, it has been reported that the earlier the helmet is applied, the more rapid and complete the correction will be [6]. Some studies have suggested that helmet therapy initiated before 6 months of age is preferable [11,15]. However, infants younger than 4 months old usually lack the cervical muscle strength to tolerate the helmet [11]. In contrast, helmet therapy after 1 year of age is generally less effective because the skull thickens and cranial growth slows down [9,24,25].
The findings of our study are consistent with those of previous research, demonstrating a negative relationship between the effectiveness of helmet therapy and the age of treatment initiation [11,15]. Infants who received treatment before the age of 9 months exhibited a more significant decrease in CVA/CVAI, with a reduction of 6.0 mm/4.7%, than those who began treatment later and had a reduction of 2.7 mm/2.0%. Additionally, the success rate of helmet therapy varied notably across different age groups. Group 1 (≤5 months) had a success rate of 38.8%, group 2 (5–7 months) of 45.9%, group 3 (7–9 months) of 18.2%, and group 4 (>9 months) of 0.0%. Therefore, it is critical to initiate helmet therapy after 4 months of age, when the infant can withstand the weight of the helmet, but before 9 months of age, to obtain the best treatment outcomes. These findings are of paramount significance for clinical practice and emphasize the importance of early intervention in managing plagiocephaly [15,24].
The effectiveness of helmet therapy in correcting positional plagiocephaly is dependent on the severity of the initial head shape asymmetry, with more severe cases being less likely to achieve complete correction and with a limited extent of correction [11,12]. In this study, a full correction was almost achieved in 40.9% of the infants in the moderate group, compared with only 8.3% in the severe group, with longer treatment duration in the latter. Thus, the initial head shape asymmetry severity is a critical determinant of the success of helmet therapy, affecting the likelihood and extent of achieving complete correction. Infants with more severe cases require longer treatment duration, as evidence shows that severe cases require 7.9 months and moderate cases require 5.8 months [11,12].
Furthermore, our study observed that compliance with wearing the helmet for more than 15 hours per day was linked to a higher rate of successful treatment, whereas inadequate compliance resulted in no successful outcomes [15]. Although some common side effects, such as sweating, odor, and skin rash, were reported, the therapy was generally well-tolerated, and no severe complications, including skin ulcer, occurred. The cost of helmet therapy in South Korea is approximately United States dolloar 2500.
This study had some limitations that should be considered when interpreting the results. First, there was a selection bias as only patients with positive outcomes and without complications were included in the study, and the study lacked a well-established validated scale for measuring head deformation. Additionally, a control group was not available for comparison owing to the retrospective nature of the chart review. Second, the study focused solely on plagiocephaly and excluded brachycephaly from the analysis. Future studies can be improved by including patients with brachycephaly. Moreover, recent concerns have emerged regarding the potential adverse effects of moderate to severe positional plagiocephaly on cognitive and academic outcomes [12]. Therefore, future research should incorporate long-term evaluations of psychomotor development in infants who receive helmet therapy and parental feedback on their child's quality of life after treatment.
In conclusion, with increasing parental concerns about their baby’s head shape, the use of helmet therapy has increased recently. For proper helmet therapy, accurate anthropometric measurements of the head are crucial, and it is important to rule out conditions that require surgical treatment, such as craniosynostosis. Helmet therapy is effective for infants with moderate to severe positional plagiocephaly. The rate of change in CVA/CVAI through helmet therapy is significantly influenced by the age at which the therapy is initiated, duration of daily wear, and severity of the initial condition. Therefore, pediatricians should have a strong understanding of the indications for helmet therapy and assist parents in making informed decision regarding whether to pursue this treatment for their child.
Footnotes
Fig. 1.
Characteristic morphology of plagiocephaly (A) and differentiation from lambdoid synostosis (B) on a physical examination. Positional plagiocephaly has an overall “parallelogram” appearance with flattening of the occipital region associated with ipsilateral frontal bossing and anterior displacement of the ipsilateral ear. However, patients with lambdoid synostosis have an overall “trapezoid-shaped” head, with the ipsilateral ear positioned both interiorly and posteriorly due to changes in the skull base.
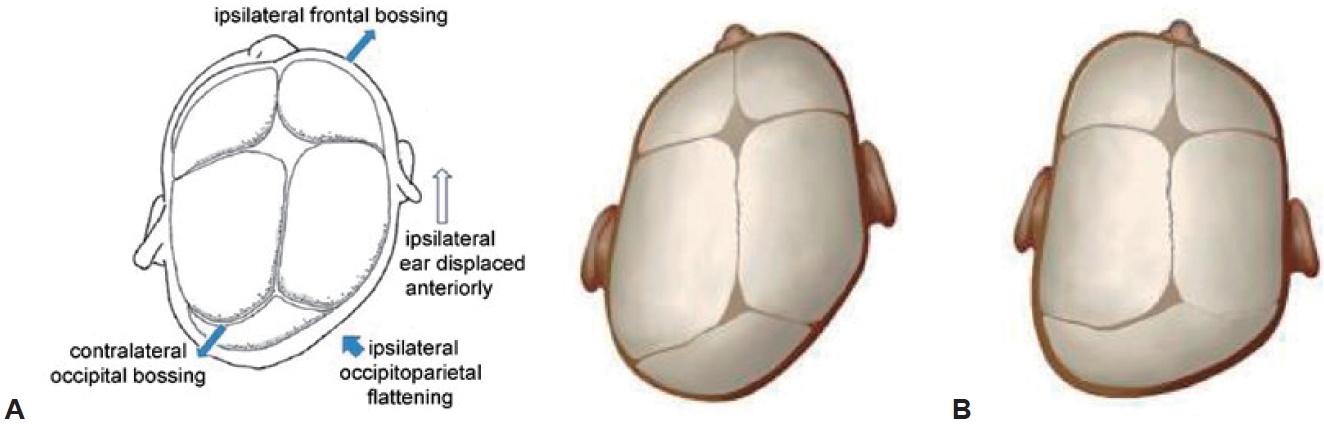
Fig. 2.
Measuring the patient with a sliding caliper (A) and diagonally (B). (A) A sliding caliper is a standard instrument used to measure the distance between 2 points on the surface of the head. Measurement accuracy is the first step in diagnosing positional plagiocephaly. (B) Diagonal measurements were recorded between the lateral side of the eyebrow and contralateral occiput. CVA (mm) = Diagonal A - Diagonal B. CVAI (%)=CVA/diagonal B×100% (Diagonal A >Diagonal B). CVA, cranial vault asymmetry; CVAI, CVA index.
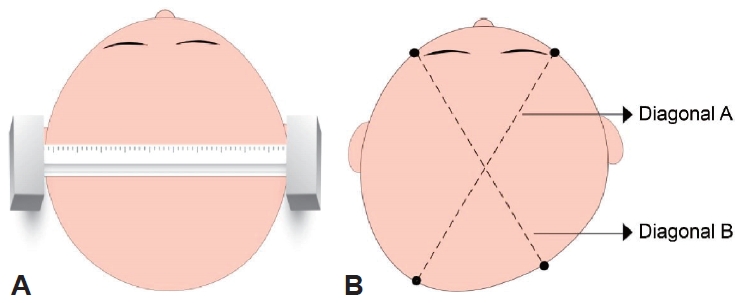
Fig. 3.
Using a 3-dimensional scanner to measure head shape. With the examiner holding the infant, 360° scans were performed. The obtained data were analyzed using analytical software to obtain 3-dimensional images and determine cranial shape.
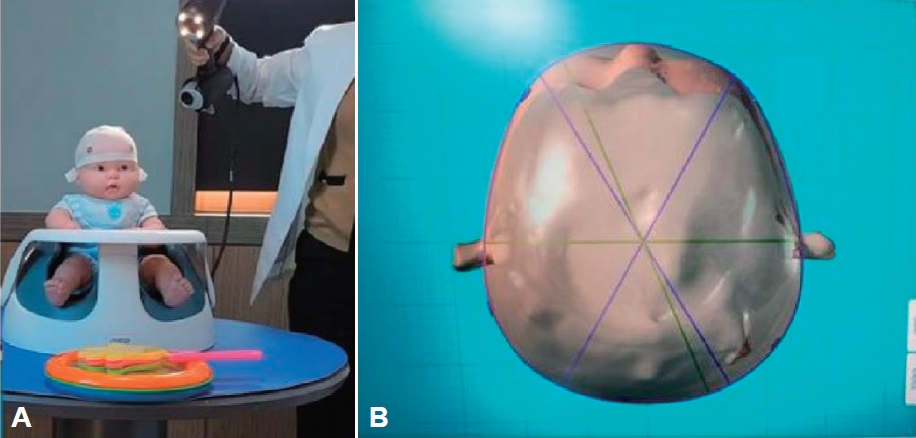
Fig. 4.
Processes from the doctor’s office to helmet wearing: After a patient is diagnosed with moderate to severe positional plagiocephaly, it takes approximately 2 weeks to begin helmet therapy. CVA, cranial vault asymmetry; CVAI, CVA index; 3D, 3-dimensional.

Fig. 5.
Treatment algorithm for positional plagiocephaly. CVA, cranial vault asymmetry; CVAI, CVA index.
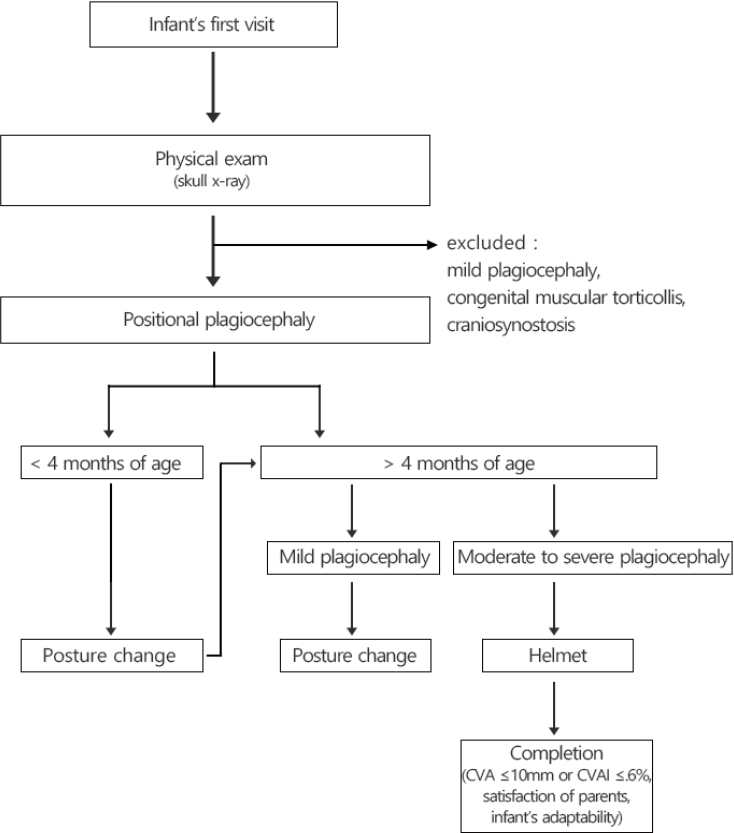
Table 1.
The patients’ initial CVA and CVAI measurements, compliance, helmet therapy duration, and age at therapy initiation
Table 2.
Effectiveness of helmet therapy based on CVA and CVAI
| Variable | Mean (range) | P value |
|---|---|---|
| Initial CVA (mm) | 12.4 (8.0–19.0) | - |
| Final CVA (mm) | 6.3 (0.1–11.8) | <0.001 |
| Initial CVAI (%) | 9.1 (6.4–15.0) | - |
| Final CVAI (%) | 4.3 (0.1–8.0) | <0.001 |
Table 3.
Effectiveness of helmet therapy according to age at therapy initiation
Table 4.
Effectiveness of helmet therapy according to initial severity
| Initial severity | No. | Mean therapy period (mo) | Treatment Successa), n (%) |
CVA (mean) |
CVAI (mean) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Initial | Final | Change | P value | Initial | Final | Change | P value | ||||
| Moderateb) | 66 | 5.8 | 60 (90.9) | 11.1 | 5.7 | 5.4 | <0.001 | 8.1 | 3.9 | 4.2 | <0.001 |
| Severec) | 24 | 7.9 | 16 (66.7) | 16.0 | 8.0 | 8.0 | <0.001 | 12.0 | 5.4 | 6.6 | <0.001 |
| Total | 90 | 6.9 | 76 (84.4) | 13.4 | 6.9 | 6.5 | <0.001 | 10.1 | 4.7 | 5.4 | <0.001 |
Table 5.
Effectiveness of helmet therapy according to helmet wearing duration
| Compliance (hr/day) | No. | Mean therapy period (mo) | Normala) (%) (after treatment), n (%) |
CVA (mean) |
CVAI (mean) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Initial | Final | change | P value | Initial | Final | change | P value | ||||
| Poor (<15) | 4 | 6.3 | 0 (0) | 13.3 | 10.1 | 3.2 | 0.124 | 10.0 | 7.1 | 2.9 | 0.091 |
| Good (15–19) | 85 | 6.4 | 33 (38.8) | 12.4 | 6.2 | 6.2 | <0.001 | 9.1 | 4.2 | 4.9 | <0.001 |
| Excellent (≥20) | 1 | 6.1 | 1 (100) | 10.5 | 3.1 | 7.4 | - | 8.0 | 2.2 | 5.8 | - |
| Total | 90 | 6.4 | 34 (37.8) | 12.1 | 6.5 | 5.6 | - | 9.0 | 4.5 | 4.5 | - |
Table 6.
Influences of key variables on changes in CVA and CVAI following helmet therapy
| Variable |
Regression model 1 (dependent variable: CVA [mm]) |
Regression model 2 (dependent variable: CVAI [%]) |
||||
|---|---|---|---|---|---|---|
| B | β | t-value | B | β | t-value | |
| Control variable | ||||||
| Sex | -0.086 | -0.017 | 0.019 | 0.005 | 0.067 | -0.220 |
| Prematurity | -1.425* | -0.201 | -0.664 | 0.408 | -1.628 | -2.580 |
| Independent variable | ||||||
| Helmet starting age (mo) | -0.483** | -0.300 | -0.382*** | -0.306 | -4.100 | -3.835 |
| Compliance (hr/day) | 0.323*** | 0.347 | 0.269*** | 0.371 | 5.402 | 4.459 |
| Initial severity (CVA>15 mm) | 2.956*** | 0.452 | 2.254*** | 0.513 | 7.086 | 5.985 |
| Constant | 5.517 | 3.808 | ||||
| R2 (Adj. R2) | 0.529 (0.501) | 0.584 (0.560) | ||||
| F | 18.893*** | 23.618*** | ||||
References
1. Rogers GF. Deformational plagiocephaly, brachycephaly, and scaphocephaly. Part I: terminology, diagnosis, and etiopathogenesis. J Craniofac Surg 2011;22:9–16.

2. Freudlsperger C, Bodem JP, Kargus S, Castrillon-Oberndorfer G, Hoffman J, Engel M. The incidence of complications associated with molding helmet therapy: an avoidable risk in the treatment of positional head deformities? J Craniofac Surg 2015;26:e299–302.

3. Gump WC, Mutchnick IS, Moriarty TM. Complications associated with molding helmet therapy for positional plagiocephaly: a review. Neurosurg Focus 2013;35:E3.

4. Di Chiara A, La Rosa E, Ramieri V, Vellone V, Cascone P. Treatment of deformational plagiocephaly with physiotherapy. J Craniofac Surg 2019;30:2008–13.


5. Vles JS, Colla C, Weber JW, Beuls E, Wilmink J, Kingma H. Helmet versus nonhelmet treatment in nonsynostotic positional posterior plagiocephaly. J Craniofac Surg 2000;11:572–4.


6. van Wijk RM, van Vlimmeren LA, Groothuis-Oudshoorn CG, Van der Ploeg CP, Ijzerman MJ, Boere-Boonekamp MM. Helmet therapy in infants with positional skull deformation: randomised controlled trial. BMJ 2014;348:g2741.



7. van Wijk RM, Boere-Boonekamp MM, Groothuis-Oudshoorn CG, van Vlimmeren LA, IJzerman MJ. Helmet therapy Assessment in infants with Deformed Skulls (HEADS): protocol for a randomised controlled trial. Trials 2012;13:108.


8. González-Santos J, González-Bernal JJ, De-la-Fuente Anuncibay R, Soto-Cámara R, Cubo E, Aguilar-Parra JM, et al. Infant cranial deformity: cranial helmet therapy or physiotherapy? Int J Environ Res Public Health 2020;17:2612.



9. Noto T, Nagano N, Kato R, Hashimoto S, Saito K, Miyabayashi H, et al. Natural-course evaluation of infants with positional severe plagiocephaly using a three-dimensional scanner in Japan: comparison with those who received cranial helmet therapy. J Clin Med 2021;10:3531.



10. Kim HY, Chung YK, Kim YO. Effectiveness of helmet cranial remodeling in older infants with positional plagiocephaly. Arch Craniofac Surg 2014;15:47–52.



11. de Ribaupierre S, Vernet O, Rilliet B, Cavin B, Kalina D, Leyvraz P. Posterior positional plagiocephaly treated with cranial remodeling orthosis. Swiss Med Wkly 2007;137:368–72.



12. Takamatsu A, Hikosaka M, Kaneko T, Mikami M, Kaneko A. Evaluation of the molding helmet therapy for Japanese infants with deformational plagiocephaly. JMA J 2021;4:50–60.


13. Rowland K, Das N. PURLs: helmets for positional skull deformities: a good idea, or not? J Fam Pract 2015;64:44–6.


14. Argenta L, David L, Thompson J. Clinical classification of positional plagiocephaly. J Craniofac Surg 2004;15:368–72.


15. Argenta LC, David LR, Wilson JA, Bell WO. An increase in infant cranial deformity with supine sleeping position. J Craniofac Surg 1996;7:5–11.


16. Pelligra R, Doman G, Leisman G. A reassessment of the SIDS back to sleep campaign. Sci World J 2005;5:550–7.




17. Yoo HS, Rah DK, Kim YO. Outcome analysis of cranial molding therapy in nonsynostotic plagiocephaly. Arch Plast Surg 2012;39:338–44.



18. Ellwood J, Draper-Rodi J, Carnes D. The effectiveness and safety of conservative interventions for positional plagiocephaly and congenital muscular torticollis: a synthesis of systematic reviews and guidance. Chiropr Man Therap 2020;28:31.




19. Dorhage KWW, Beck-Broichsitter BE, von Grabe V, Sonntag A, Becker ST, Wiltfang J. Therapy effects of head orthoses in positional plagiocephaly. J Craniomaxillofac Surg 2016;44:1508–14.


20. Morrison CS, Chariker M. Positional plagiocephaly: pathogenesis, diagnosis, and management. J Ky Med Assoc 2006;104:136–40.

21. Jung BK, Yun IS. Diagnosis and treatment of positional plagiocephaly. Arch Craniofac Surg 2020;21:80–6.




22. Clarren SK, Smith DW, Hanson JW. Helmet treatment for plagiocephaly and congenital muscular torticollis. J Pediatr 1979;94:43–6.


23. Kim DG, Lee JS, Lee JW, Yang JD, Chung HY, Cho BC, et al. The effects of helmet therapy relative to the size of the anterior fontanelle in nonsynostotic plagiocephaly: a retrospective study. J Clin Med 2019;8:1977.



24. Kim MJ, Kang MK, Deslivia MF, Kim YO, Choi JW. Applicative factors of helmet molding therapy in late-diagnosed positional plagiocephaly. J Korean Med Sci 2020;35:e295.









 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


