Article Contents
| Clin Exp Pediatr > Volume 67(9); 2024 |
|
Abstract
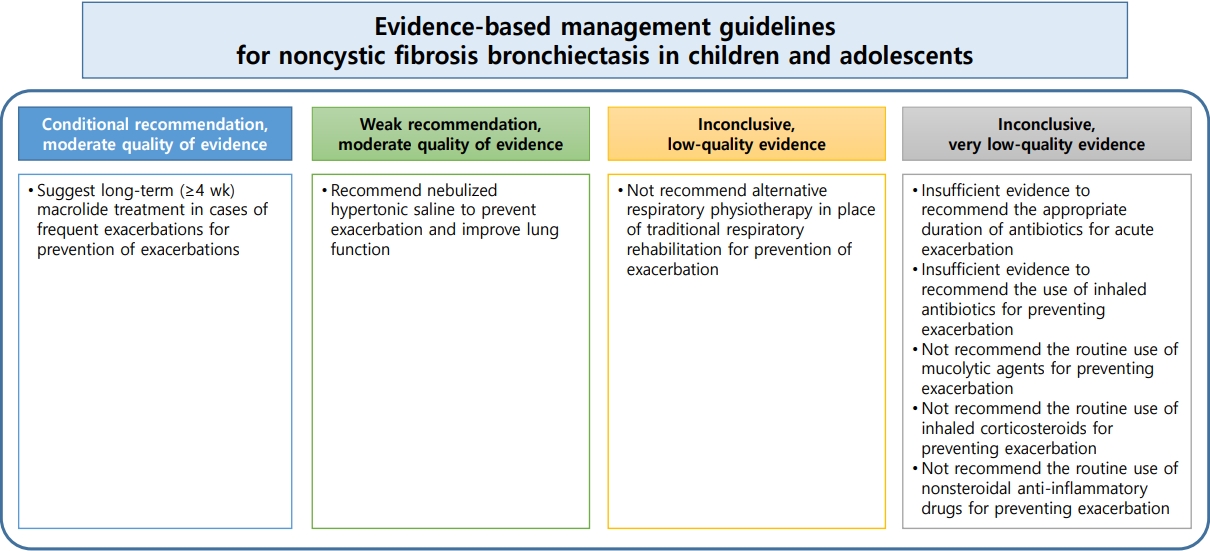
Noncystic fibrosis bronchiectasis is a chronic respiratory disease that carries high socioeconomic and medical burdens and is caused by diverse respiratory illnesses. To improve clinical outcomes, early recognition, active treatment of exacerbations, and prevention of further exacerbations are essential. However, evidence for the treatment and prevention of acute exacerbation of noncystic fibrosis bronchiectasis, especially in children, is lacking. Therefore, the evidence- and consensus-based guidelines for medical and nonmedical treatment strategies for noncystic fibrosis bronchiectasis in children and adolescents were developed by the Korean Academy of Pediatric Allergy and Respiratory Disease using the methods recommended by the Grading of Recommendations Assessment, Development, and Evaluation working group with evidence published through July 2, 2020. This guideline encompasses evidence-based treatment recommendations as well as expert opinions, addressing crucial aspects of the treatment and management of non-cystic fibrosis bronchiectasis in children. This includes considerations for antibiotics and airway clearance strategies, particularly in areas where evidence may be limited. Large, well-designed, and controlled studies are required to accumulate further evidence of management strategies for noncystic fibrosis bronchiectasis in children and adolescents.
Graphical abstract
Bronchiectasis is a chronic lung disease characterized by a persistent wet cough combined with abnormal bronchial dilatation caused by diverse respiratory and genetic disorders [1,2]. Owing to its chronic clinical course and recurrent exacerbations, a considerable disease burden has been reported in patients with bronchiectasis and their family members. Noncystic fibrosis bronchiectasis is sometimes underestimated, partially due to the lack of recognition and information about the condition. However, clinical research on noncystic fibrosis bronchiectasis has been increasing with respect to the burden of the disease, its effects on quality of life, and concerns regarding its appropriate management [3].
Consensus is lacking on appropriate management strategies, except for antibiotic use, during acute exacerbations in patients with noncystic fibrosis bronchiectasis, especially children. The heterogeneous features and rarity of noncystic fibrosis bronchiectasis, especially in children, have led to difficulty developing management guidelines and prevention strategies. Nonetheless, the early recognition and proper management of noncystic fibrosis bronchiectasis in children are essential for improving clinical outcomes and reducing disease burden. Management strategies based on the available evidence from studies that focused only on children and adolescents with noncystic fibrosis bronchiectasis are limited. Most evidence guiding the management of noncystic fibrosis bronchiectasis in children and adolescents was extrapolated from studies performed in children with cystic fibrosis bronchiectasis and adults with noncystic fibrosis or cystic fibrosis bronchiectasis. These guidelines, developed by the Guideline Development Committee of the Korean Academy of Pediatric Allergy and Respiratory Disease, aim to encourage an evidence-based approach to the management of noncystic fibrosis bronchiectasis in children and adolescents (Table 1).
The definition of bronchiectasis varies slightly among studies. However, to improve clinical outcomes and aid therapeutic development for bronchiectasis, a consensus on the definition is required. The gold standard of the diagnosis of bronchiectasis is high-resolution computed tomography of the chest, more ideally performed during a clinically stable state [4]. In a recently published international consensus recommendation, the radiologic definition of bronchiectasis in adults included an inner airway–arterial diameter ratio of ≥1.5, with the highest score for each graded criterion, followed by an outer airway–arterial diameter ratio of ≥1.5 and a lack of tapering and visibility of the peripheral airways [5]. However, a bronchoarterial ratio >0.80 is considered abnormal in children [6]. Therefore, the definition of bronchiectasis in children includes a bronchoarterial ratio >0.80 with compatible clinical symptoms, including persistent or recurrent(>3) episodes of a wet or productive cough and crackles with or without digital clubbing (Table 2) [7]. Symptoms can be intermittent when patients with bronchiectasis are clinically stable.
Numerous definitions of bronchiectasis exacerbations exist. An acute exacerbation of bronchiectasis is defined based on a deterioration in three or more of the following key symptoms: cough, sputum volume or sputum purulence, breathlessness or exercise intolerance, fatigue or malaise, and hemoptysis lasting at least 48 hours [8]. A severe exacerbation of bronchiectasis is defined as the presence of any of the following symptoms or signs: tachypnea, acute respiratory failure, exacerbated chronic respiratory failure, a significant decline in arterial oxygen saturation or respiratory function or hypercapnia, fever >38˚C, or hemoptysis [9].
The global prevalence and common causes of bronchiectasis differ among geographic regions, age, and depth of investigation. Cystic fibrosis is among the most common causes of bronchiectasis in Western countries, whereas noncystic fibrosis bronchiectasis is common in Asia and developing countries [1,7]. The prevalence of postinfection, as one of the most common causes of bronchiectasis in children and adolescents, varies among studies [10].In a study highlighting the causes of bronchiectasis in Korean children and adolescents, the most common cause was pre-existing respiratory infections (55.3%), followed by post-infectious bronchiolitis obliterans (14.3%), pulmonary tuberculosis (12.3%), combined heart diseases (5.6%), primary ciliary dyskinesia (4.5%), primary immunodeficiency (3.3%), recurrent aspiration with or without gastroesophageal reflux (3.0%), neuromuscular diseases (2.8%), congenital lung diseases (2.8%), cystic fibrosis (1.4%), and interstitial lung diseases (1.4%) [1]. In an estimated 37% of patients with bronchiectasis, the causes of bronchiectasis were not identified, while cystic fibrosis was the cause in an estimated 1.4% (5 of 358) of Korean children and adolescents with bronchiectasis [1]. In-depth investigations are needed to identify the disease underlying bronchiectasis to improve the disease management and prognosis.
The exact mechanisms of noncystic fibrosis bronchiectasis, especially in children, have not been identified despite considerable efforts owing to the difficulty in obtaining lower airway specimens. Airway inflammation in non-cystic fibrosis bronchiectasis caused by various underlying diseases may have distinct features related to the underlying disease [11]. However, dysregulated airway inflammation in response to an altered airway microbiome and respiratory pathogens may partially explain the pathophysiology regardless of the underlying cause [12].
The diverse airway inflammatory phenotypes, including neutrophilic inflammation and less commonly eosinophilic inflammation, contribute to the development, prognosis, and treatment response of noncystic fibrosis bronchiectasis in children and adolescents [13-15]. In addition to airway inflammation, increased systemic inflammation, reflected in tumor necrosis factor-α (TNF-α), interferon-γ, perforin, and granzyme levels, has been observed in children and adolescents with bronchiectasis [16]. This suggests that low-grade systemic inflammation is involved in bronchiectasis.
Pediatric pulmonary specialists from the Korean Academy of Pediatric Allergy and Respiratory Disease Society formed the Guideline Development Committee. Committee members participated in discussions and arrived at a consensus to formulate the key questions to be addressed in the guidelines. Eight key questions were identified using the Population, Intervention, Comparison, and Outcome (PICO) framework. The members also participated in a literature search, data extraction, evidence synthesis, and recommendation development. Preventing bronchiectasis exacerbations and treatment efficacy are important outcomes. This evidence- and consensus-based guideline was developed using methods recommended by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group [17].
A systematic literature search of the PubMed, Embase, and Cochrane Library databases was conducted to answer eight key questions. Articles published through July 2, 2020, were considered for inclusion. To identify papers published in Korean, Chinese, and Japanese, the KoreaMed, Igaku Chuo Zasshi, and Chinese National Knowledge Infrastructure databases were also searched.
Three experts systematically reviewed the selected studies against each key question. The literature was independently selected by 2 experts; if a difference was noted in the selection results, the final studies were included through an agreement process involving discussion and arbitration by a third expert.
The Cochrane Association for Randomized Comparative Clinical Trials was used to evaluate the quality of the selected studies. For the synthesis of evidence, a meta-analysis was performed of study type (e.g., randomized controlled trials [RCTs] or case-control studies), participants’ characteristics, interventions, and results from each selected study, and the GRADE approach was used to evaluate the quality of the evidence.
Recommendation: We recommend offering long-term macrolide antibiotics to children and adolescents with non-cystic fibrosis bronchiectasis who have frequent exacerbations (conditional recommendation, moderate quality of evidence).
Summary of evidence: In addition to their antibacterial effects, macrolide antibiotics have immuneregulatory effects, including regulating pro- and anti-inflammatory immune responses [18]. Long-term macrolides have been praised for their role in preventing acute exacerbations of noncystic fibrosis bronchiectasis in children and adolescents. Moreover, controlling acute exacerbations is key to the management of these patients. We identified four double-blinded RCTs that investigated the use of macrolides for more than 4 weeks for the management of noncystic fibrosis bronchiectasis in children and adolescents [19-22].
Although each study investigated the effects of different macrolides (azithromycin 30 mg/kg once weekly [20]; clarithromycin 15 mg/kg once daily [21]; erythromycin 125 mg once daily for patients weighing ≤15 kg and 250 mg once daily for those weighing >15 kg [22]; and roxithromycin 4 mg/kg twice daily [19]) across the different study period (24 months [20], 3 months [21], 52 weeks [22], and 12 weeks [19], respectively), the meta-analysis of these four studies [19-22] demonstrated the potential beneficial role of long-term macrolide treatment in managing noncystic fibrosis bronchiectasis in children and adolescents. One study involving the use of roxithromycin in children with noncystic fibrosis bronchiectasis demonstrated that a 12-week treatment course improved airway hyperresponsiveness, sputum purulence score, and sputum leucocyte score [19]. An acute exacerbation of bronchiectasis occurred in 2 patients in the placebo group versus zero patients in the roxithromycin treatment group [19].
Another study assessing the impact of clarithromycin in children with bronchiectasis observed improved inflammatory parameters in bronchoalveolar lavage and sputum samples. However, the study did not measure clinical improvements, including exacerbations of bronchiectasis [21]. A meta-analysis of three RCTs [19,20,22] of the effects of long-term macrolide treatment on the frequency of acute exacerbations of bronchiectasis reported that long-term macrolide treatment can effectively reduce the frequency of exacerbations (odds ratio [OR], 0.30; 95% confidence interval [CI], 0.10–0.87) [23]. The mean number of exacerbations of bronchiectasis per patient during the macrolide treatment period decreased without serious or other adverse events [23]. Moreover, long-term macrolide use improved the sputum purulence score, although the antibiotic use did not affect the pulmonary function index and cytokine levels such as TNF-α and interleukin-8 (IL-8) in sputum and bronchoalveolar lavage samples [21].
Remark: One study that investigated the ability of long-term macrolides to prevent exacerbations of noncystic fibrosis bronchiectasis in children and adolescents demonstrated an increased incidence of antibiotic resistance (azithromycin-resistant Streptococcus pneumoniae: OR, 13.20; 95% CI, 1.61–108.19; azithromycin-resistant Staphylococcus aureus: OR, 4.16; 95% CI, 1.06–16.32; azithromycin-resistant bacteria: OR, 7.13; 95% CI, 2.13–23.79) after long-term azithromycin treatment [20]. Considering the risks and benefits of long-term macrolide treatment, macrolides can be used to prevent frequent acute exacerbations of noncystic fibrosis bronchiectasis in children and adolescents.
Recommendation: Insufficient evidence is available to recommend the appropriate duration of antibiotic administration for acute exacerbations of noncystic fibrosis bronchiectasis in children and adolescents (inconclusive, very low quality evidence).
Summary of evidence: No RCTs have examined the effects of short-versus long-term antibiotic use on acute exacerbations of noncystic fibrosis bronchiectasis in children and adolescents. A study reported that 10 experts reached consensus on antibiotic treatment for 10–14 days for acute exacerbations of noncystic fibrosis bronchiectasis [24]. The consensus was defined as >70% agreement among experts, although firm evidence was lacking [24]. In the future, establishing the appropriate duration of antibiotic use for managing exacerbations of noncystic fibrosis bronchiectasis in children and adolescents will be necessary.
Remark: For the treatment of the exacerbation of nonsevere bronchiectasis in children, amoxicillin–clavulanate or azithromycin can be administered [25]. However, appropriate antibiotics should be selected considering the antibiotic susceptibility of respiratory infectious pathogens in each patient.
Recommendation: Insufficient evidence exists to recommend the use of inhaled antibiotics for preventing noncystic fibrosis bronchiectasis in children and adolescents (inconclusive, very low quality of evidence).
Summary of evidence: Evidence is lacking to recommend the use of inhaled antibiotics for acute exacerbation of noncystic fibrosis bronchiectasis in children and adolescents. In adults with noncystic fibrosis bronchiectasis, a placebo-controlled, double-blinded RCT identified that inhaled tobramycin administered twice daily for 4 weeks significantly decreased the density of Pseudomonas aeruginosa in sputum samples and improved the medical conditions compared to no treatment [26]. In another multicenter, randomized, double-blinded, placebo-controlled study of 42 adults with noncystic fibrosis bronchiectasis and ciprofloxacin-sensitive P. aeruginosa, dual-release inhaled ciprofloxacin, formulated to optimize airway antibiotic delivery with a schedule of 28 days on/28 days off for 24 weeks, significantly reduced bacterial density at day 28 and delayed the time to the first pulmonary exacerbation [27]. Further investigations are necessary to verify the effects of inhaled antibiotics treatment for acute exacerbations of noncystic fibrosis bronchiectasis in children and adolescents.
Remark: Inhaled antibiotics can prevent exacerbations of noncystic fibrosis bronchiectasis. Furthermore, nebulized amikacin or tobramycin can also be safely used to prevent such exacerbations [28]. The availability of inhaled antibiotics varies among countries and may be limited by high costs.
Recommendation: We do not recommend the routine use of mucolytic agents for preventing exacerbations of noncystic fibrosis bronchiectasis in children and adolescents (inconclusive, very low-quality evidence).
Summary of evidence: None of the RCTs were relevant to the PICO question. In a study of 88 adults with bronchiectasis, bromhexine combined with antibiotics improved expectoration and reduced sputum quantity, exhibiting no differences in adverse effects between the placebo and bromhexine groups [29]. In a short-term (15-day) prospective study of older patients with bronchiectasis, significant improvements in pulmonary function, including forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC), with mucus density, mucus purulence, and produced mucus volume, were observed in those receiving oral erdosteine and chest physiotherapy compared with those receiving chest physiotherapy alone [30]. In 2 RCTs of adults with noncystic fibrosis bronchiectasis, recombinant human DNase usage failed to demonstrate significant benefits in pulmonary functions compared with placebo [31,32].
Remark: No studies have evaluated the effectiveness of mucolytic agent use in preventing exacerbations of noncystic fibrosis bronchiectasis in children and adolescents. The limited evidence on the effects of mucolytic agents for noncystic fibrosis bronchiectasis in children and adolescents was obtained from a small number of studies in adults with bronchiectasis. Therefore, whether mucolytic agents can prevent exacerbations of noncystic fibrosis bronchiectasis in children and adolescents remains unclear.We agree with the conditional recommendation of mucolytic agent usage as an add-on therapy for preventing the deterioration of sputum-related or repeated respiratory infections in children and adolescents with noncystic fibrosis bronchiectasis considering the short-term benefits of mucolytic agent usage in addition to other treatments in adults with bronchiectasis.
Recommendation: We do not recommend the routine use of ICS for preventing exacerbations of noncystic fibrosis bronchiectasis in children and adolescents (inconclusive, very low quality of evidence).
Summary of evidence: Only one observational study has investigated the use of ICS for treating noncystic fibrosis bronchiectasis in children (n=27) [14]. No significant differences were noted in the symptom score (4 vs. 3, P=0.27), oxygen saturation (95% vs. 97%, P=0.06), lung function (FEV1% predicted: 82% vs. 83%, P=0.73), the neutrophil ratio in sputum (29.9% vs. 46.8%, P=0.20), TNF-α in sputum (58 pg⁄mL vs. 44.5 pg⁄mL, P=0.55), and IL-8 (2.7 ng⁄mL vs. 2.4 ng⁄mL, P=0.82) before start of treatment and 12 weeks after completion of treatment. However, bronchial hyperreactivity significantly increased (37% vs. 63%,P=0.016), and neutrophil apoptosis in the sputum significantly reduced (42.8% vs. 20.2%, P=0.03) beyond 12 weeks after continuing ICS in 27 children with noncystic fibrosis bronchiectasis who had used ICS for at least 6 months.
Remark: Whether ICS treatment can prevent exacerbations of bronchiectasis in children and adolescents remains unclear. However, we agree with the conditional recommendation for the use of ICS in children and adolescents with noncystic fibrosis bronchiectasis and bronchial hyperreactivity.
Recommendation: We do not recommend the routine use of nonsteroidal anti-inflammatory drugs (NSAIDs) to prevent exacerbations of noncystic fibrosis bronchiectasis in children and adolescents (inconclusive, very low quality of evidence).
Summary of evidence: NSAIDs have dose-dependent antibacterial effects against gram-negative bacteria including P. aeruginosa [33] as well as anti-inflammatory properties [34]. In one observational study of 25 adults with chronic lung disease, including eight with bronchiectasis, those treated with inhaled indomethacin (1.2 µg/mL 3 times/day) for 14 days demonstrated a reduced amount of sputum, from 189±19 g/day to 95±21 g/day (P<0.001), and from 7.1 ±0.5 to 4.5±0.4 (P<0.01) according to Borg`s ratio scale, a self-reported tool to measure the intensity of perceived effort, without adverse effects, such as hypotension and bronchoconstriction [35]. However, no improvement was observed in FEV1 and vital capacity [35]. In another RCT of children and adolescents with cystic fibrosis, high-dose ibuprofen (40–60 mg/kg/day) reduced the predicted decline rate of FVC% and hospitalization length [36].
Remark: The effectiveness of NSAIDs in preventing exacerbations of noncystic fibrosis bronchiectasis in children and adolescents remains unclear. The long-term use of high-dose ibuprofen can increase the risk of gastrointestinal disorders and bleeding. Therefore, careful consideration of the risks and benefits of NSAID use is necessary. Additionally, the drug should be used only in selected patients with repeated drug-resistant bacterial infections and excessive airway inflammation.
Recommendation: We recommend the use of nebulized hypertonic saline to prevent exacerbation of bronchiectasis in children and adolescents with improved lung function (weak recommendation, moderate quality of evidence).
Summary of evidence: Hyperosmolar agents can enhance mucociliary clearance by altering mucus viscosity, thereby increasing airway clearance [37,38]. One study demonstrated that nebulized hypertonic saline (7%) is more beneficial in terms of expectorated sputum weight and ease of expectoration than isotonic saline nebulization (0.7%) in patients with stable bronchiectasis [39]. A total of 52 children and adolescents with noncystic fibrosis bronchiectasis were randomized to receive 200 µg of inhaled salbutamol, followed by 3% hypertonic saline nebulization or 200 µg of inhaled salbutamol (control group) for 8 weeks prior to chest physiotherapy [40]. After a 4-week washout period, they were crossed over to the opposite arms in the second phase. The 3% hypertonic saline nebulization arm in both groups displayed statistically significant improvements in FEV1 and FVC compared with the control arm. The mean number of exacerbations was significantly lower in the 3% hypertonic saline nebulization arm versus the control arm (0.42±0.64 vs. 1.30±1.05, P=0.01) in phase I. However, this difference was not significant in phase II (0.65±0.74 vs. 1.03±0.77, P=0.074).
Remark: In one RCT of infants with cystic fibrosis, the inhalation of 6% hypertonic saline was well tolerated, and no significant differences were noted in the number of adverse events between the control(inhalation of 0.9% isotonic saline) and trial (inhalation of 6% hypertonic saline) groups [41]. The lung clearance index and weight gain were significantly improved in the nebulized hypertonic saline versus the control group [41]. However, no significant differences were noted in the pulmonary exacerbation and chest magnetic resonance imaging scores between the control and trial groups [41]. Moreover, the inhalation of hypertonic saline may cause discomfort by overstimulating the cough reflex and may cause bronchospasm [42,43]. Therefore, the nebulized saline should be used with caution in children with bronchial hyperreactivity and infants with small airway diameters.
Recommendation: We do not recommend an alternative airway clearance technique over conventional respiratory rehabilitation to prevent exacerbations of noncystic fibrosis bronchiectasis in children and adolescents (inconclusive, low-quality evidence).
Summary of evidence: The promotion of airway clearance in noncystic fibrosis bronchiectasis is necessary to increase mucus transport and prevent the exacerbation and progression of bronchiectasis [44]. Current evidence indicates that airway clearance therapy can lead to short-term improvements in mucus transport compared to not employing any airway clearance techniques [45]. To improve airway clearance, alternative techniques and traditional chest physiotherapy can be used. Traditional chest physiotherapy requires the assistance of another person, such as a caregiver, and includes vibration, percussion, and postural drainage, whereas alternative airway clearance techniques, such as positive expiratory pressure devices, can be self-administered.
No RCT to date has compared alternative respiratory physiotherapy with traditional respiratory rehabilitation therapy. In one observational study of eight adults and adolescents with noncystic fibrosis bronchiectasis, lung function was significantly improved by 6.8% (P<0.01) in patients receiving individually tailored professional physiotherapy [46]. One demonstrated that positive expiratory pressure was better able to decrease frequency in pulmonary exacerbations and extend the time to the first pulmonary exacerbation than high-frequency chest wall oscillation in children and adults with cystic fibrosis [47].
Another RCT including six children with cystic fibrosis and 6 children with bronchiectasis of unknown origin demonstrated that positive expiratory pressure significantly improved lung volume, whereas postural drainage and percussion did not [48]. However, positive expiratory pressure and postural drainage and percussion did not improve pulmonary function [48]. These findings were maintained when patients with cystic fibrosis and those with bronchiectasis of unknown origin were considered a group [48]. A controlled randomized crossover study demonstrated that both conventional pulmonary rehabilitations, including postural drainage, percussion, and vibration, and high-frequency chest wall oscillation significantly increased pulmonary functions with no differences between the 2 pulmonary rehabilitation methods [49]. In the 2 RCTs of children and adolescents with chronic lung disease, including primary ciliary dyskinesia, a high-frequency chest wall oscillator effectively improved lung function versus traditional respiratory rehabilitation [49,50].
Remark: Individualized pulmonary rehabilitation, such as high-frequency chest wall oscillators and the Acapella device, can be applied to prevent exacerbations of noncystic fibrosis bronchiectasis in children and adolescents considering the pathophysiology of the underlying airway inflammation.
Current evidence is limited for preventing acute exacerbations of bronchiectasis, especially in children and adolescents with noncystic fibrosis bronchiectasis. The present management guidelines for noncystic fibrosis bronchiectasis in children and adolescents, which were developed based on the GRADE approach with eight PICO questions to improve clinical outcomes, provide optimal management strategies with weighted benefits and risks for each recommendation. These guidelines will help improve the clinical outcomes of children and adolescents with noncystic fibrosis bronchiectasis. However, large RCTs are required to improve the evidence base for each management strategy.
Acknowledgments
The guidelines for noncystic fibrosis bronchiectasis in children and adolescents were developed with support from the Korean Academy of Pediatric Allergy and Respiratory Diseases. These guidelines align with those for noncystic fibrosis bronchiectasis in children and adolescents published by the Korean Academy of Pediatric Allergy and Respiratory Disease. Additionally, the guidelines have been approved for publication by the Korean Academy of Pediatric Allergy and Respiratory Disease. The authors thank all members of the Clinical Guideline Development Committee of the Korean Academy of Pediatric Allergy and Respiratory Diseases. We also thank Miyoung Choi (National Evidence-Based Healthcare Collaborating Agency, Seoul, Republic of Korea) for providing helpful comments about the data analysis.
Table 1.
Summary of Population, Intervention, Comparison, and Outcome framework used to formulate the guideline questions and recommendations
Table 2.
Diagnosing bronchiectasis in children and adults
References
1. Lee E, Shim JY, Kim HY, Suh DI, Choi YJ, Han MY, et al. Clinical characteristics and etiologies of bronchiectasis in Korean children: a multicenter retrospective study. Respir Med 2019;150:8-14.


2. Chang AB, Grimwood K, Boyd J, Fortescue R, Powell Z, Kantar A. Management of children and adolescents with bronchiectasis: summary of the ERS clinical practice guideline. Breathe (Sheff) 2021;17:210105.



3. Marchant JM, Cook AL, Roberts J, Yerkovich ST, Goyal V, Arnold D, et al. Burden of care for children with bronchiectasis from parents/carers perspective. J Clin Med 2021;10:5856.



5. Aliberti S, Goeminne PC, O'Donnell AE, Aksamit TR, Al-Jahdali H, Barker AF, et al. Criteria and definitions for the radiological and clinical diagnosis of bronchiectasis in adults for use in clinical trials: international consensus recommendations. Lancet Respir Med 2022;10:298-306.


6. Kapur N, Masel JP, Watson D, Masters IB, Chang AB. Bronchoarterial ratio on high-resolution CT scan of the chest in children without pulmonary pathology: need to redefine bronchial dilatation. Chest 2011;139:1445-50.


7. Chang AB, Bush A, Grimwood K. Bronchiectasis in children: diagnosis and treatment. Lancet 2018;392:866-79.


8. Hill AT, Haworth CS, Aliberti S, Barker A, Blasi F, Boersma W, et al. Pulmonary exacerbation in adults with bronchiectasis: a consensus definition for clinical research. Eur Respir J 2017;49:1700051.


9. Martinez-Garcia MA, Olveira C, Maiz L, Giron RMf, Prados C, de la Rosa D, et al. Bronchiectasis: a complex, heterogeneous disease. Arch Bronconeumol (Engl Ed) 2019;55:427-33.


10. McCallum GB, Binks MJ. The epidemiology of chronic suppurative lung disease and bronchiectasis in children and adolescents. Front Pediatr 2017;5:27.



11. Wijers CD, Chmiel JF, Gaston BM. Bacterial infections in patients with primary ciliary dyskinesia: Comparison with cystic fibrosis. Chron Respir Dis 2017;14:392-406.




12. Richardson H, Dicker AJ, Barclay H, Chalmers JD. The microbiome in bronchiectasis. Eur Respir Rev 2019;28:190048.



13. Lee E, Hong SJ. Pharmacotherapeutic strategies for treating bronchiectasis in pediatric patients. Expert Opin Pharmacother 2019;20:1025-36.


14. Guran T, Ersu R, Karadag B, Karakoc F, Demirel GY, Hekim N, et al. Withdrawal of inhaled steroids in children with noncystic fibrosis bronchiectasis. J Clin Pharm Ther 2008;33:603-11.


15. Pizzutto SJ, Grimwood K, Bauert P, Schutz KL, Yerkovich ST, Upham JW, et al. Bronchoscopy contributes to the clinical management of indigenous children newly diagnosed with bronchiectasis. Pediatr Pulmonol 2013;48:67-73.


16. Hodge G, Upham JW, Chang AB, Baines KJ, Yerkovich ST, Pizzutto SJ, et al. Increased Peripheral Blood Pro-Inflammatory/Cytotoxic Lymphocytes in Children with Bronchiectasis. PLoS One 2015;10:e0133695.



17. Schünemann H, Bro ek J, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendation [Internet]. Version 3.2. [updated 2013 Oct; cited 2023 Jun 28]. Available from: https://gdt.gradepro.org/app/handbook/handbook.html.
18. López-Boado YS, Rubin BK. Macrolides as immunomodulatory medications for the therapy of chronic lung diseases. Curr Opin Pharmacol 2008;8:286-91.


19. Koh YY, Lee MH, Sun YH, Sung KW, Chae JH. Effect of roxithromycin on airway responsiveness in children with bronchiectasis: a double-blind, placebo-controlled study. Eur Respir J 1997;10:994-9.


20. Valery PC, Morris PS, Byrnes CA, Grimwood K, Torzillo PJ, Bauert PA, et al. Long-term azithromycin for Indigenous children with noncystic-fibrosis bronchiectasis or chronic suppurative lung disease (Bronchiectasis Intervention Study): a multicentre, double-blind, randomised controlled trial. Lancet Respir Med 2013;1:610-20.


21. Yalçin E, Kiper N, Ozçelik U, Do ru D, Firat P, Sahin A, et al. Effects of claritromycin on inflammatory parameters and clinical conditions in children with bronchiectasis. J Clin Pharm Ther 2006;31:49-55.


22. Masekela R, Anderson R, Gongxeka H, Steel H, Becker P, Green R. Lack of efficacy of an immunomodulatory macrolide in childhood HIV related bronchiectasis: a randomised, placebo-controlled trial. J Antivir Antiretrovir 2013;5:44-9.
23. Lee E, Sol IS, Kim JD, Yang HJ, Min TK, Jang GC, et al. Long-term macrolide treatment for noncystic fibrosis bronchiectasis in children: a meta-analysis. Sci Rep 2021;11:24287.




24. Judson MA, Chaudhry H, Compa DR, O'Donnell AE. A Delphi study of pharmacotherapy for noncystic fibrosis bronchiectasis. Am J Med Sci 2014;348:387-93.


25. Goyal V, Grimwood K, Byrnes CA, Morris PS, Masters IB, Ware RS, et al. Amoxicillin-clavulanate versus azithromycin for respiratory exacerbations in children with bronchiectasis (BEST-2): a multicentre, double-blind, non-inferiority, randomised controlled trial. Lancet 2018;392:1197-206.



26. Barker AF, Couch L, Fiel SB, Gotfried MH, Ilowite J, Meyer KC, et al. Tobramycin solution for inhalation reduces sputum Pseudomonas aeruginosa density in bronchiectasis. Am J Respir Crit Care Med 2000;162:481-5.


27. Serisier DJ, Bilton D, De Soyza A, Thompson PJ, Kolbe J, Greville HW, et al. Inhaled, dual release liposomal ciprofloxacin in noncystic fibrosis bronchiectasis (ORBIT-2): a randomised, double-blind, placebo-controlled trial. Thorax 2013;68:812-7.



28. Ailiyaer Y, Wang X, Zhang Y, Li C, Li T, Qi Q, et al. A prospective trial of nebulized amikacin in the treatment of bronchiectasis exacerbation. Respiration 2018;95:327-33.



29. Olivieri D, Ciaccia A, Marangio E, Marsico S, Todisco T, Del Vita M. Role of bromhexine in exacerbations of bronchiectasis. Double-blind randomized multicenter study versus placebo. Respiration 1991;58:117-21.



30. Crisafulli E, Coletti O, Costi S, Zanasi E, Lorenzi C, Lucic S, et al. Effectiveness of erdosteine in elderly patients with bronchiectasis and hypersecretion: a 15-day, prospective, parallel, open-label, pilot study. Clin Ther 2007;29:2001-9.


31. Wills PJ, Wodehouse T, Corkery K, Mallon K, Wilson R, Cole PJ. Short-term recombinant human DNase in bronchiectasis. Effect on clinical state and in vitro sputum transportability. Am J Respir Crit Care Med 1996;154:413-7.


32. O'Donnell AE, Barker AF, Ilowite JS, Fick RB. Treatment of idiopathic bronchiectasis with aerosolized recombinant human DNase I. rhDNase Study Group. Chest 1998;113:1329-34.


33. Shah PN, Marshall-Batty KR, Smolen JA, Tagaev JA, Chen Q, Rodesney CA, et al. Antimicrobial activity of ibuprofen against cystic fibrosis-associated gram-negative pathogens. Antimicrob Agents Chemother 2018;62:e01574-17.




34. Pizzutto SJ, Upham JW, Yerkovich ST, Chang AB. Inhaled non-steroid anti-inflammatories for children and adults with bronchiectasis. Cochrane Database Syst Rev 2016;2016:CD007525.



35. Tamaoki J, Chiyotani A, Kobayashi K, Sakai N, Kanemura T, Takizawa T. Effect of indomethacin on bronchorrhea in patients with chronic bronchitis, diffuse panbronchiolitis, or bronchiectasis. Am Rev Respir Dis 1992;145:548-52.


36. Lands LC, Milner R, Cantin AM, Manson D, Corey M. High-dose ibuprofen in cystic fibrosis: Canadian safety and effectiveness trial. J Pediatr 2007;151:249-54.


37. Nicolson CH, Stirling RG, Borg BM, Button BM, Wilson JW, Holland AE. The long term effect of inhaled hypertonic saline 6% in noncystic fibrosis bronchiectasis. Respir Med 2012;106:661-7.


38. Kellett F, Robert NM. Nebulised 7% hypertonic saline improves lung function and quality of life in bronchiectasis. Respir Med 2011;105:1831-5.


39. Kellett F, Redfern J, Niven RM. Evaluation of nebulised hypertonic saline (7%) as an adjunct to physiotherapy in patients with stable bronchiectasis. Respir Med 2005;99:27-31.


40. Anuradha K, Gunathilaka PKG, Wickramasinghe VP. Effectiveness of hypertonic saline nebulization in airway clearance in children with noncystic fibrosis bronchiectasis: a randomized control trial. Pediatr Pulmonol 2021;56:509-15.


41. Stahl M, Wielpütz MO, Ricklefs I, Dopfer C, Barth S, Schlegtendal A, et al. Preventive inhalation of hypertonic saline in infants with cystic fibrosis (PRESIS). A Randomized, double-blind, controlled study. Am J Respir Crit Care Med 2019;199:1238-48.


42. Clarke SW, Thomson ML, Pavia D. Effect of mucolytic and expectorant drugs on tracheobronchial clearance in chronic bronchitis. Eur J Respir Dis Suppl 1980;110:179-91.

43. Büchele G, Rzehak P, Weinmayr G, Keil U, Leupold W, von Mutius E, et al. Assessing bronchial responsiveness to hypertonic saline using the stepwise protocol of Phase Two of the International Study of Asthma and Allergies in Childhood (ISAAC II). Pediatr Pulmonol 2007;42:131-40.


44. Lee AL, Burge AT, Holland AE. Airway clearance techniques for bronchiectasis. Cochrane Database Syst Rev 2015;2015:CD008351.



45. Warnock L, Gates A. Airway clearance techniques compared to no airway clearance techniques for cystic fibrosis. Cochrane Database Syst Rev 2023;4:CD001401.



46. Dagan A, Vilozni D, Sokol G, Onn A, Efrati O. Effect of professional physiotherapy on patients with non CF bronchiectasis–a preliminary study. Pneumologie 2016;70:A39.

47. McIlwaine MP, Alarie N, Davidson GF, Lands LC, Ratjen F, Milner R, et al. Long-term multicentre randomised controlled study of high frequency chest wall oscillation versus positive expiratory pressure mask in cystic fibrosis. Thorax 2013;68:746-51.


48. Santamaria F, Celentano L, Buonpensiero P, Sarnelli P, Caterino M, Raia V. Positive expiratory pressure treatment: efficacy in pulmonary diseases. J Pediatr 1998;133:717-8.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


