Article Contents
| Clin Exp Pediatr > Volume 68(4); 2025 |
|
Abstract
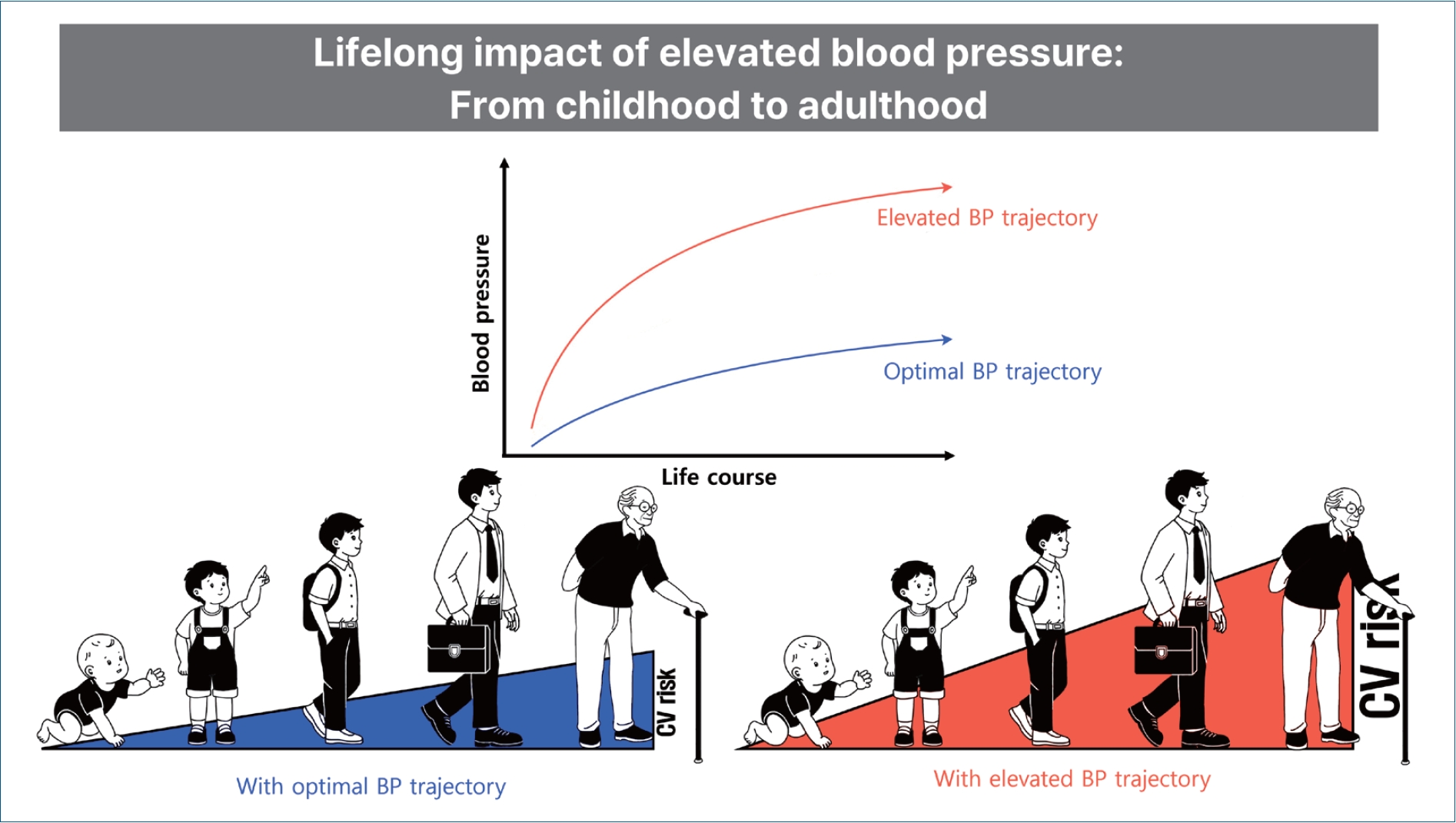
Elevated blood pressure (BP) during childhood and adolescence is increasingly being recognized as a precursor to adult hypertension and cardiovascular disease (CVD). This review examines the existing evidence of the relationship between early BP elevations and long-term cardiovascular (CV) outcomes. Previous studies demonstrated a moderate association between childhood BP and adult hypertension, with early BP elevations contributing to subclinical CV changes such as left ventricular hypertrophy and increased carotid intima-media thickness as well as major premature CVD events in adulthood. However, evidence also indicates that BP normalization before adulthood may mitigate these risks, suggesting a critical interventional window before irreversible CV changes occur. Multiple modifiable and nonmodifiable factors contribute to early-life BP elevations, including genetic predisposition, a high sodium intake, obesity, sedentary behavior, and sleep disturbances. Although establishing a direct causal association between childhood BP and adult hypertension or CVD remains challenging owing to the need for longterm follow-up and large sample sizes, further research is essential to addressing the existing knowledge gaps in pediatric hypertension prevention, detection, impact, and treatment. This review highlights the importance of preventing BP elevations early in life to reduce the longterm burden of hypertension and CVD. Promoting healthy behaviors, such as maintaining a healthy weight, reducing one's sodium intake, engaging in physical activity, and ensuring adequate sleep, is essential for managing BP at an early age. These efforts reduce individual CV risk and help alleviate the broader future public health burden of hypertension and CVD.
Graphical abstract. BP, blood pressure.
The prevalence of hypertension remains high, with 54% of adults diagnosed with hypertension worldwide. Of them, an estimated 3%–5% and 10%–14% developed hypertension and elevated blood pressure (BP), respectively, prior to reaching adulthood [1-7]. Pediatric hypertension can develop secondary to an underlying disease or primary hypertension. Although secondary hypertension is more prevalent and often more severe in children than adults, preventable BP elevation and its cumulative effect remain critical across all hypertension types, even in the general population with normal BP [6]. The increasing trend in pediatric hypertension is concerning given that hypertension is among the leading causes of cardiovascular disease (CVD) [8-11]. A recent study evaluating trends in metabolic diseases among individuals under 40 years of age reported that hypertension had the highest age-standardized mortality rate [12]. Also, among young adults aged 20–39 years, those with an elevated BP exhibited a greater risk of premature CVD than their normotensive counterparts: hazard ratio (HR), 1.14 (95% confidence interval [CI], 1.09–1.18) for elevated BP, 1.67 (1.61– 1.72) for stage 1 systolic and diastolic hypertension (SDH), and 3.13 (3.03–3.23) for stage 2 SDH. In particular, early and long-term exposure to an elevated BP is expected to contribute to targeted organ damage and CVD in young adult populations [13]. However, due to the higher prevalence of hypertension with advancing age, most previous studies focused on older adults [14-16].
The increasing burden of hypertension in the young population can cause an increased disease burden now and in the future; however, direct evidence of an elevated BP and hypertension in children and adolescents remains limited. Therefore, understanding the potential impact of an early elevated BP and its associated risk factors is crucial for reducing individual risks and preventing future public health burdens [17-20]. This review aimed to examine the existing body of evidence linking elevated BP in childhood, primarily primary BP elevation or hypertension, with progression to adult hypertension and CVD as well as identify the risk factors contributing to early-life BP elevation.
A large body of literature has reported a continuous relationship between BP and cardiovascular (CV) risk in adults [21]. Although hypertension is traditionally defined by arbitrary cutoff values such as ≥140/90 mmHg based on the magnitude of the risk of CVD, evidence of the continuous relationship between BP and CV risk has prompted efforts to address the risk for individuals below this cutoff. For instance, the 2017 American College of Cardiology/American Heart Association guideline lowered the threshold to ≥130/80 mmHg [17].
However, the definition of elevated BP and hypertension in children and adolescents is complex. Children exhibit considerably lower BP than adults [22]. An individual's BP naturally increases with age and height, requiring differentiation from an abnormal elevation [2]. Moreover, evidence of the long-term risk of target organ damage associated with an elevated BP during childhood remains limited. These limitations hinder the determination of arbitrary cutoffs in children, leading to the definition of pediatric hypertension based on the percentiles of age-, sex-, and height-specific BP distributions in healthy children [2,23]. Pediatric hypertension is identified when BP is markedly elevated, for instance, above the 95th percentile, although this may not adequately address the cumulative CV risk in children with an elevated BP below the 95th percentile [24]. Therefore, various criteria and definitions for elevated BP levels and hypertension in children have been employed based on available evidence.
The 2017 American Academy of Pediatrics (AAP) guidelines define normal BP, elevated BP, stage 1 hypertension, and stage 2 hypertension as screening and management criteria for an elevated BP in children and adolescents [2]. Based on BP distributions in healthy normal-weight children, those aged 1–12 years whose BP levels exceeded the age-, sex-, and height-specific 90th percentiles were classified as having an elevated BP. For adolescents aged 13 and older, the cutoffs are 120–129/<80 mmHg for elevated BP and ≥130/80 mmHg for hypertension. The reference values for older adolescents, which align with those for adults, are supported by robust evidence linking BP to CV risk in adults and young adults [2]. The European Society of Hypertension and Hypertension Canada used repeated BP measurements above the 95th percentile [25]. Additionally, the 2019 Japanese Society of Hypertension Guidelines for the Management of Hypertension established 6 reference values based on age and sex [26]. Hypertension is defined at values of ≥120/70 mmHg for preschool children, with the reference values increasing as children grow, and reaching ≥140/70 mmHg for high schoolers, converging with adult hypertension cutoffs.
The criteria for pediatric hypertension in Korea were aligned with the AAP guidelines as reflected in the 2017 recommendations of the Korean Society of Hypertension [27]. The BP percentile for individuals is calculated by considering age-, sex-, and height-specific percentiles along with the measured BP for children and adolescents; it is then classified based on this BP percentile [27].
Increasing evidence suggests that adult hypertension may originate early in life (Table 1). A meta-analysis of longitudinal studies estimated that a one-standard-deviation increase in childhood BP was associated with a higher likelihood of adult hypertension with an odds ratio (OR) of 1.71 (95% CI, 1.50–1.95) for systolic BP (SBP) and an OR of 1.57 (95% CI, 1.37–1.81) for diastolic BP (DBP) [28]. An elevated BP in childhood defined using BP percentiles had an OR of 2.02 (95% CI, 1.62–2.53), while using static BP cutoff yielded an OR of 3.22 (95% CI, 1.90-5.48) [28]. Another study measured baseline BP values among adolescents aged 16–19 years, categorizing them into optimal, normal, and high-normal BP groups according to European guidelines, and subsequently assessed the development of adult hypertension [29]. As a result, the ORs for adult hypertension were 1.30 (95% CI, 1.22–1.39) for the normal BP group and 1.79 (95% CI, 1.67–1.93) for the high-normal BP group compared to the optimal group [29]. Several studies investigated BP tracking and identified distinct trajectories from childhood to adulthood. One study conducted group-based trajectory modeling using BP measurements at the ages of 7, 11, 18, 26, 32, and 38 years in a birth cohort of 975 individuals [30]. Four distinct trajectory groups were identified: normal (22%), high-normal (43%), prehypertensive (32%), and hypertensive (4%) [30]. Individuals in the hypertensive group exhibited an elevated BP during childhood that persisted into adulthood [30].
BP tracking from childhood to young adulthood demonstrates a relatively clear association. For instance, among adolescents with a mean age of 14.2 years, every 10-mmHg increase in SBP and DBP was associated with a 4% increased risk of developing hypertension in their 20s [31]. In contrast, BP tracking from childhood to midadulthood is limited since it requires an extended follow-up period and large sample size [22]. Despite the scarcity of such studies, one tracked the BP of 211 participants from childhood (3–18 years) to middle age (30–50 years) [32]. BP was measured every 10 years from the age 18 years. The BP levels during the early school years and early puberty were strong predictors of hypertension at 50 years of age [32]. Additionally, the International Childhood Cardiovascular Cohort Consortium study found that the prevalence of hypertension in middle-aged adults was 19% among individuals who maintained a normal BP throughout childhood and adolescence and 80% among those with a persistently elevated BP [33]. Interestingly, participants whose BP was elevated during childhood but normalized during adolescence had a lower prevalence of adult hypertension than those with a persistently elevated BP [33]. Most studies reported that BP tracking from childhood to adulthood shows a moderate correlation with that in adulthood [34,35]. A meta-analysis estimated an overall moderate correlation coefficient; as baseline age decreased or the follow-up period lengthened among studies, this BP-tracking correlation tended to weaken [34]. Taken together, not all individuals with an elevated BP during childhood develop hypertension in adulthood, highlighting the potential benefits of early detection and intervention.
Hypertension is a well-known risk factor for CVD. The Northern Manhattan Study estimated that the population attributable risk of hypertension for CVD was 24.3% (95% CI, 13.2–35.4) [36]. Although the prevalence of hypertension and CVD is considerably lower in younger populations than in other age groups, the evidence linking elevated BP to CVD risk in young adults is equally robust. Compared to normotensive young adults aged 20–39 years, the HR for CVD development was 1.14 (95% CI, 1.09–1.18) for those with an elevated BP, 1.67 (95% CI, 1.61–1.72) for those with stage 1 SDH and 3.13 (95% CI, 3.03–3.23) for those with stage 2 SDH [37].
The observed CVD risk associated with hypertension in adults appears to extend to children and adolescents, although evidence remains limited owing to the challenges posed by extended follow-up (Table 2). A longitudinal study following late adolescents aged 18–20 years found an association between elevated BP and premature CVD before 55 years of age with an HR of 1.09 (95% CI, 1.04–1.15) [8]. Another long-term study spanning up to 50 years confirmed that, among individuals with a persistently elevated BP from adolescence, one in 10 will experience myocardial infarction, heart failure, ischemic stroke, intracerebral hemorrhage, or CV death before retirement [38].
Even in the absence of a major CV event, an elevated BP during childhood has a cumulative detrimental effect on CV health. A meta-analysis of 12 prospective cohort studies exhibited a significant association between an elevated BP in childhood and adolescence and 3 intermediate indicators of CVD in adulthood: high pulse wave velocity, high carotid intima-media thickness (cIMT), and left ventricular hypertrophy (LVH) [11]. A cross-sectional analysis of 130 children with a persistent BP elevation above the 90th percentile reported that 17% of young patients exhibited concentric LVH, a geometric change associated with increased CVD risk in adults [39]. Additionally, a recent United Kingdom birth cohort study reaffirmed that childhood BP was associated with cumulative cardiac damage in adulthood, and BP levels and echocardiography were assessed in 1,856 adolescents aged 17 and 24 years [40]. An elevated BP was defined as an SBP ≥130 mmHg and DBP ≥85 mmHg, while LVH was defined as a left ventricular mass indexed to height2.7 (LVMI2.7) ≥51 g/m2.7 and left ventricular diastolic dysfunction (LVDD) was defined as left ventricular diastolic function E/A <1.5. An elevated BP in adolescence was associated with worsening LVH (OR, 1.61 [95% CI, 1.43–1.80]) and worsening LVDD (OR, 1.35 [95% CI, 1.21–1.50]) in female participants [40]. The cIMT is a well-established predictor of CVD incidence [41]. A persistently elevated BP from childhood through adulthood nearly doubled the risk of high cIMT compared with consistently normal BP levels [42]. A multicenter study of high BP in pediatric patients, the Adult Hypertension Onset in Youth cohort, demonstrated a linear increase in LVMI and higher prevalence of LVH with increasing SBP. The prevalence of LVH was 13% in normotensive children, 21% in those with an SBP in the 80th–90th percentile, and 27% in those with an SBP above the 90th percentile [43].
Studies utilizing the BP trajectory model added to these findings: participants who developed a high BP in adulthood were not only likely to have an elevated BP in childhood, but they also exhibited suboptimal CV indicators [30,44]. Based on BP data of patients aged 7–38 years, 4 distinct trajectories were identified (normal, high-normal, prehypertensive, and hypertensive) that showed progressive worsening of CV risk factors at 38 years of age, with the hypertensive group displaying the poorest outcomes [30]. The observed risk factors include waist/hip ratio, total cholesterol, low high-density lipoprotein cholesterol, glycated hemoglobin, and triglyceride levels [30]. Another trajectory study assessed subclinical CVD risk based on SBP trajectories throughout childhood. Over a follow-up period of up to 23 years, from baseline (age 5–16 years) into young adulthood, low-, moderate-, and high-increasing groups were identified. A progressive worsening of cIMT was observed across these groups, with values of 0.50, 0.52, and 0.55 mm, respectively [44]. Similarly, the mean LVMI values were 65.41, 72.02, and 79.23 g/m2, respectively [44].
Previous studies also suggested that elevated levels in childhood, followed by normalization, were not significantly associated with increased subclinical atherosclerosis or arterial stiffness [42,45]. However, it remains unclear whether this reduction was due to active interventions following the recognition of BP elevation. Although further research is needed to clarify and quantify the causal relationship between childhood BP and adult CV outcomes, these studies indicated the long-term and cumulative effects of persistent BP elevations throughout childhood and adolescence on the development of hypertension and CVD later in life.
Physiologically, BP increases with age and height throughout childhood, with the greatest increase occurring during adolescence [46]. However, this natural increase does not occur uniformly across all children; some may experience a steeper increase, potentially predisposing them to heightened CV risk later in life. Previous studies demonstrated early-life predictors associated with hypertension in adulthood, including perinatal factors such as a low birth weight and maternal history of pregnancy hypertension; genetic factors such as a family history of hypertension; and sociodemographic factors such as male sex and specific ethnic groups (e.g., Black or African American populations) [30].
In addition to these predictors, various modifiable risk factors contribute to the excessive increase in BP from childhood to adulthood. For instance, a high sodium intake has been identified as a significant risk factor [47,48]. A meta-analysis of 18 studies with high-quality sodium intake data found that each gram of sodium intake per day was associated with a 0.8-mmHg increase in SBP and a 0.7-mmHg increase in DBP [47]. Another study using the National Health and Nutrition Examination Survey reported that a sodium intake of >3,450 mg was associated with elevated BP (OR, 1.36 [95% CI, 1.04–1.77]) compared to ≤2,300 mg per 2,000 calories [48]. Notably, a pioneering study in the 1960s compared BP levels by age between 2 indigenous Amazonian tribes [49,50]. The Mundurucus tribe, influenced by Western dietary practices and salt incorporation into its diet, exhibited a pronounced age-related increase in BP as observed in most acculturated societies. In contrast, the Carajás tribe, which remains unacculturated and uses plant ash instead of salt, maintained low BP levels throughout adulthood [49]. These findings underscore the cumulative impact of a high sodium intake on BP elevations despite limitations such as an insufficient control of confounders. They also suggested that the natural distribution of BP in the absence of excessive salt exposure may shift rightward compared with the distribution observed in contemporary societies, while previous studies were largely conducted in acculturated populations. In this context, the 2017 AAP guidelines recommend the Dietary Approaches to Stop Hypertension (DASH) diet as an initial intervention for children with an elevated BP [2]. A randomized controlled trial found that youth aged 11–18 years in the 6-month DASH diet intervention group exhibited a significant reduction in SBP (2.7 mmHg) and improvement in flow mediated dilation (2.5%) compared to the routine care group [51].
The increasing prevalence of insufficient physical activity and sedentary lifestyles has contributed to a higher prevalence of both obesity and early elevated BP in childhood and adolescence [52-55]. A systematic review reported that high-intensity interval training interventions are associated with small but significant reductions in SBP and DBP [56]. Also, school-based interventions were proven effective; compared to the traditional curriculum, high-intensity interval training during the first 20 minutes of school physical education classes held 2 days a week resulted in a significant decrease in SBP and vascular stiffness at the 3-month assessment [57].
Obesity is a strong risk factor for elevated BP in both children and adolescents. A national case-control study found that a one-unit increase in body mass index (BMI) was associated with a 0.56-mmHg increase in SBP and a 0.54-mmHg increase in DBP in obese children [55]. Moreover, an increase in age- and sex-adjusted BMI was associated with elevated SBP and DBP in both obese and nonobese children [55]. A longitudinal UK cohort study that followed 1,856 adolescents for 7 years also reported that an elevated DBP was 1.41 times more likely to worsen LVH, while an elevated SBP was 1.30 times more likely to increase left ventricular filling pressure in overweight and obese participants than in normotensive groups [40]. However, the heightened risk of obesity in childhood seems modifiable: Compared to participants who maintained a normal weight throughout childhood and young adulthood, the relative risk of adult hypertension was 3.79 (95% CI, 2.49–5.64) for overweight participants during both periods [58]. It is noteworthy that individuals who were overweight in childhood but normal weight in young adulthood did not show a significant increase in risk (relative risk, 1.05 [95% CI, 0.33–3.40]) [58].
Additionally, sleep disturbances in childhood, including poor sleep quality, sleep interruptions, and short sleep duration (≤8 hr/night), are also associated with higher BP levels, especially in adolescents [59]. Obstructive sleep apnea is a pathological sleep condition common in children with obesity-related hypertension [60]. Other risk factors, such as a low socioeconomic status (e.g., poverty) and multiple adverse childhood experiences, are outlined in Table 3.
Elevated BP and hypertension in children have received relatively insufficient attention owing to the low prevalence of primary hypertension and CVD and the inherent difficulties conducting long-term studies to assess their impact in pediatric populations. However, emerging evidence suggests that hypertension and CVD develop early in life.
Although BP naturally increases with age during childhood and adolescence, the rate and pattern of this increase vary, with some individuals maintaining an optimal BP and others experiencing a steeper rise. The effect of an elevated BP during childhood may not be immediately apparent. However, without timely and appropriate intervention, elevated BP trajectories can persist into adulthood, substantially increasing one's CV risk (Fig. 1). Numerous studies, both direct and indirect, have demonstrated that a high BP during childhood significantly increases the risk of hypertension in adulthood. Prolonged exposure to a high BP during childhood leads to cumulative subclinical changes that potentially result in irreversible cardiac structural alterations or major premature CV events. While future efforts to establish evidence that guides consensus—such as the necessity of regular BP screening and determining optimal timing and target BP for pharmacological treatment in children—remain under debate, the benefits of maintaining optimal BP throughout childhood and addressing elevated BP through lifestyle modifications are already evident. Promoting healthy behaviors in children and adolescents, such as maintaining a healthy body weight, reducing sodium intake, engaging in regular physical activity, abstaining from smoking, and ensuring adequate sleep, is crucial for managing BP from an early age and fostering lifelong habits that support CV health. These efforts are essential for reducing individual risk and efficiently mitigating the future burden on public healthcare systems given the substantial burden of hypertension and CVD.
Footnotes
Fig. 1.
Schematic illustration of various blood pressure trajectories (A) and the corresponding progression of cardiovascular risk (B) throughout the lifespan. Chidren who experience high (a), moderate (b), or low elevations (c) in blood pressure (A) are subsequently at high (a), moderate (b), or low risk (c) of developing hypertension, subclinical target organ damage, and cardiovascular disease (B), respectively. The green arrows represent the impact of preventive efforts, with earlier interventions exerting a more substantial influence on blood pressure trajectories and cardiovascular risk progression than later interventions.
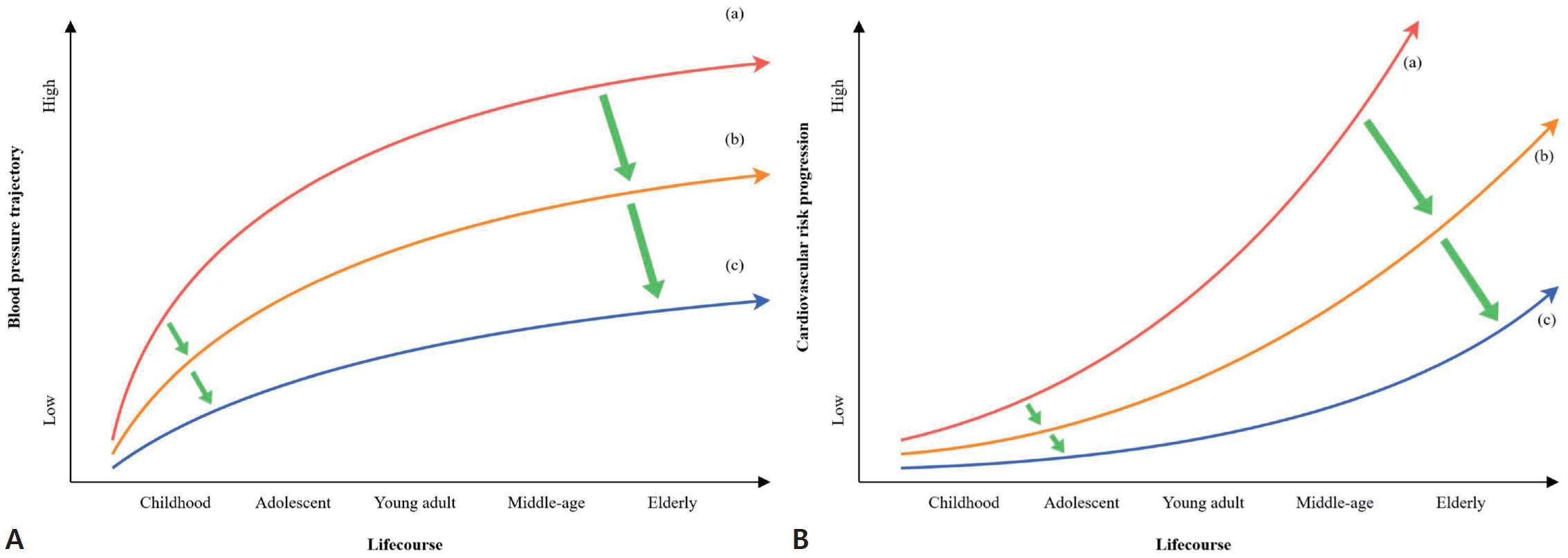
Table 1.
Characteristics of studies of association between childhood BP and adult BP
| Study | Study period | Data source | No. of participants | Participants at baseline | Childhood BP definition | Adult BP definition |
|---|---|---|---|---|---|---|
| Israeli et al. [29] 2007 | 1976–1996 | Israeli Defense Forces Staff Periodic Examination Center | 18,513 | 16.5–19 Yr | BP category by European clas sification guidelinesa) | Hypertension: SBP >140 mmHg, DBP >90 mmHg |
| Juhola et al. [42] 2012 | 1980, 2001, and2007 | The Cardiovascular Risk in Young Finns Study | 2,625 | 6 Age cohorts (3, 6, 9, 12, 15, and 18 years old) | Elevated BP: ≥90th percentile according to age-, sex-, and height-specific BP | Hypertension: SBP/DBP ≥130/85 mmHg or use of antihypertensive medication |
| Mills et al. [17] 2015 | 1985, 2004–2006 | The Childhood Determinants of Adult Health Study | 798 | 7–15 Yr | Elevated BP: ≥95th percentile according to age-, sex- and height-specific BP | Elevated BP: SBP/DBP ≥120/80 mmHg |
| Hypertension: SBP/DBP ≥140/90 mmHg or taking antihypertensive medication | ||||||
| Kalantari et al. [31] 2017 | 1999–2001, and 2008–2011 | Tehran Lipid and Glucose Study | 1,579 | 10–19 Yr | Hypertension BP: ≥95th per centile according to age-, gender- and height-specific BP | Hypertension: SBP/DBP ≥140/90 mmHg or use of antihypertensive medication |
| Sarganas et al. [61] 2018 | 2003–2006, and 2009–2012 | The German Health Interview and Examination Survey for Children and Adolescents | 526 | 11–17 Yr | Elevated BP: ≥95th percentile according to age-, sex- and height-specific BP | Hypertension: SBP/DBP ≥140/90 mmHg |
| Urbina et al. [33] 2019 | 1970s to 1980s | The International Childhood Cardiovascular Cohort Consortium Study | 5,035 | 10–19 Yr | High BP: ≥90th percentile or SBP ≥120 mmHg | Normal SBP <120 mmHg; High SBP ≥120 mmHg |
| Du et al. [62] 2019 | 1973–2016 | Bogalusa Heart Study | 3,940 | 3–18 Yr | Elevated BP: ≥90th percentile according to age-, sex- and height-specific BP | Hypertension: SBP/DBP≥140/90 mmHg or use of antihypertensive medication |
| Yang et al. [28] 2020 | Articles published up to November 2019 | 11 articles | 181 to 26,980 | 3–18 Yr | (1) Age-, sex- and height- specific BP percentile values | (1) Hypertension: SBP/DBP ≥140/90 mmHg, SBP/DBP ≥130/85 mmHg or use of antihypertensive medication |
| (2) Arbitrary BP cutoffs | ||||||
| (3) A continuous variable (used a 1 SD increase in BP) | (2) Elevated BP: SBP/DBP ≥120/80 mmHg or use of antihypertensive medication |
Table 2.
Characteristics of studies of association between childhood BP and adult CVD
| Study | Study period | Data source | No. of participants | Participants at baseline | Childhood BP definition | Adult BP definition |
|---|---|---|---|---|---|---|
| Falkstedt et al. [8] 2008 | 1971–2004 | A nationwide survey of the Swedish military conscription | 47,873 | 18–20 Yr of male adolescents | Continuous or categorical variables (SBP: <115, 115 to <125, 125 to <135, and ≥135; DBP: <65, 65 to <75, 75 to <85, and ≥85) | Coronary heart disease, acute myocardial infarction, and stroke |
| Theodore et al. [30] 2015 | 38 Yr from 1972–1973 | The Dunedin Multidisciplinary Health and Development Study | 975 | 7, 11, 18, 26, 32, and 38 yr | 4 Groups based on BP levels (normal,, high-normal, prehypertensive,, and hypertensive) | Nonfasting total cholesterol, high-density lipoprotein cholesterol level, triglyceride level, and glycohemoglobin at the age of 38 years |
| Xi et al. [20] 2017 | 1973–1988, and 2000–2010 | The Bogalusa Heart Study | 1,225 | 6–17 Yr | Elevated BP: ≥95th percentile according to age-, sex- and height-specific BP | cIMT, PWV, and LVH |
| Koskinen et al. [63] 2019 | Different by each 6 co hort dataa) | The International Childhood Cardiovascular Cohort Consortium Study | 5,925 | 3–18 Yr | Fixed cutoffs | cIMT, PWV, and LVH |
| Rietz et al. [38] 2023 | 1969–1997 | A nationwide survey of the Swedish military conscription | 1,366,519 | 18.3 Yr (mean) | BP category by the ACC/AHA guidelinesb) | Cardiovascular death or first hospitalization for myocardial infarction, heart failure, ischemic stroke, or intracerebral hemorrhage |
| Agbaje [40] 2023 | 1991–1992, 2008–2010, and 2015–2017 | Avon Longitudinal Study of Parents and Children | 14,901 | 17 Yr | Elevated BP/hypertension: ≥130/≥85 mmHg | LVMI, RWT, LVDF, and LVFP |
| Kartiosuo et al. [64] 2024 | 1970s and 1990s | The International Childhood Cardiovascular Cohort Consortium | 10,634 | 13.3 Yr (mean) | Levels of SBP as continuous variable | Myocardial infarction, stroke, transient ischemic attack, ischemic heart failure, angina, peripheral artery disease, abdominal aortic aneurysm, carotid intervention, and coronary revascularization |
afPWV, aorta-femoral pulse wave velocity; BP, blood pressure; cIMT, carotid intima-media thickness; CVD, cardiovascular disease; DBP, diastolic blood pressure; LVDF, left ventricular diastolic dysfunction; LVFP, left ventricular filling pressure; LVH, left ventricular hypertrophy; LVMI, left ventricular mass index; RWT, relative wall thickness; SBP, systolic blood pressure.
Table 3.
Early-life predictors and modifiable risk factors of high blood pressure
References
1. Organization WH. Global report on hypertension: the race against a silent killer. Geneva (Switzerland): World Health Organization, 2023.
2. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 2017;140:e20171904.

3. Hardy ST, Sakhuja S, Jaeger BC, Urbina EM, Suglia SF, Feig DI, et al. Trends in blood pressure and hypertension among US children and adolescents, 1999-2018. JAMA Netw Open 2021;4:e213917.



4. Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr 2019;173:1154-63.



5. Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA 2007;298:874-9.


6. Bell CS, Samuel JP, Samuels JA. Prevalence of hypertension in children. Hypertension 2019;73:148-52.



7. Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the <em>Lancet</em> Commission on hypertension. Lancet 2016;388:2665-712.

8. Falkstedt D, Koupil I, Hemmingsson T. Blood pressure in late adolescence and early incidence of coronary heart disease and stroke in the Swedish 1969 conscription cohort. J Hypertens 2008;26:1313-20.


9. Morrison JA, Glueck CJ, Wang P. Childhood risk factors predict cardiovascular disease, impaired fasting glucose plus type 2 diabetes mellitus, and high blood pressure 26 years later at a mean age of 38 years: the Princeton-lipid research clinics follow-up study. Metabolism 2012;61:531-41.



10. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159-219.


11. Yang L, Magnussen CG, Yang L, Bovet P, Xi B. Elevated blood pressure in childhood or adolescence and cardiovascular outcomes in adulthood: a systematic review. Hypertension 2020;75:948-55.


12. Chong B, Kong G, Shankar K, Chew HSJ, Lin C, Goh R, et al. The global syndemic of metabolic diseases in the young adult population: a consortium of trends and projections from the Global Burden of Disease 2000–2019. Metabolism 2023;141:155402.


13. Murthy VL, Abbasi SA, Siddique J, Colangelo LA, Reis J, Venkatesh BA, et al. Transitions in metabolic risk and long-term cardiovascular health: Coronary Artery Risk Development in Young Adults (CARDIA) Study. J Am Heart Assoc 2016;5:e003934.



14. Yang Q, Chang A, Ritchey MD, Loustalot F. Antihypertensive medication adherence and risk of cardiovascular disease among older adults: a population-based cohort study. J Am Heart Assoc 2017;6:e006056.



15. Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am 2009;93:753-69.



16. Gast A, Mathes T. Medication adherence influencing factors-an (updated) overview of systematic reviews. Syst Rev 2019;8:112.




17. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016;134:441-50.



18. Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287-323.


19. McKinnon RA, Orleans CT, Kumanyika SK, Haire-Joshu D, Krebs-Smith SM, Finkelstein EA, et al. Considerations for an obesity policy research agenda. Am J Prev Med 2009;36:351-7.



20. Xi B, Zhang T, Li S, Harville E, Bazzano L, He J, et al. Can Pediatric hypertension criteria be simplified? a prediction analysis of subclinical cardiovascular outcomes from the bogalusa heart study. Hypertension 2017;69:691-6.



21. Whelton PK, Carey RM. The 2017 American College of Cardiology/American Heart Association Clinical Practice Guideline for High Blood Pressure in adults. JAMA Cardiology 2018;3:352-3.


22. Azegami T, Uchida K, Tokumura M, Mori M. Blood pressure tracking from childhood to adulthood. Front Pediatr 2021;9:785356.



23. Meng Y, Mynard JP, Smith KJ, Juonala M, Urbina EM, Niiranen T, et al. Pediatric blood pressure and cardiovascular health in adulthood. Curr Hypertens Rep 2024;26:431-50.




24. Ewald DR, Haldeman LA. Risk factors in adolescent hypertension. Glob Pediatr Health 2016;3:2333794x15625159.




25. Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens 2016;34:1887-920.


26. Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res 2019;42:1235-481.

28. Yang L, Sun J, Zhao M, Liang Y, Bovet P, Xi B. Elevated blood pressure in childhood and hypertension risk in adulthood: a systematic review and meta-analysis. J Hypertens 2020;38:2346-55.


29. Israeli E, Korzets Z, Tekes-Manova D, Tirosh A, Schochat T, Bernheim J, et al. Blood-pressure categories in adolescence predict development of hypertension in accordance with the European guidelines. Am J Hypertens 2007;20:705-9.


30. Theodore RF, Broadbent J, Nagin D, Ambler A, Hogan S, Ramrakha S, et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension 2015;66:1108-15.



31. Kalantari S, Khalili D, Asgari S, Fahimfar N, Hadaegh F, Tohidi M, et al. Predictors of early adulthood hypertension during adolescence: a population-based cohort study. BMC Public Health 2017;17:915.




32. Nelson MJ, Ragland DR, Syme SL. Longitudinal prediction of adult blood pressure from juvenile blood pressure levels. Am J Epidemiol 1992;136:633-45.


33. Urbina EM, Khoury PR, Bazzano L, Burns TL, Daniels S, Dwyer T, et al. Relation of blood pressure in childhood to self-reported hypertension in adulthood. Hypertension 2019;73:1224-30.



34. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 2008;117:3171-80.



35. Toschke AM, Kohl L, Mansmann U, von Kries R. Meta-analysis of blood pressure tracking from childhood to adulthood and implications for the design of intervention trials. Acta Paediatr 2010;99:24-9.


36. Willey JZ, Moon YP, Kahn E, Rodriguez CJ, Rundek T, Cheung K, et al. Population attributable risks of hypertension and diabetes for cardiovascular disease and stroke in the Northern Manhattan Study. J Am Heart Assoc 2014;3:e001106.



37. Lee H, Yano Y, Cho SMJ, Park JH, Park S, Lloyd-Jones DM, et al. Cardiovascular risk of isolated systolic or diastolic hypertension in young adults. Circulation 2020;141:1778-86.


38. Rietz H, Pennlert J, Nordström P, Brunström M. Blood pressure level in late adolescence and risk for cardiovascular events: a cohort study. Ann Intern Med 2023;176:1289-98.


39. Daniels SR, Loggie JMH, Khoury P, Kimball TR. Left ventricular geometry and severe left ventricular hypertrophy in children and adolescents with essential hypertension. Circulation 1998;97:1907-11.


40. Agbaje AO. Elevated blood pressure and worsening cardiac damage during adolescence. J Pediatr 2023;257:113374.


41. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation 2007;115:459-67.


42. Juhola J, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation 2013;128:217-24.



43. Urbina EM, Mendizábal B, Becker RC, Daniels SR, Falkner BE, Hamdani G, et al. Association of blood pressure level with left ventricular mass in adolescents. Hypertension 2019;74:590-6.


44. Hao G, Wang X, Treiber FA, Harshfield G, Kapuku G, Su S. Blood pressure trajectories from childhood to young adulthood associated with cardiovascular risk: results from the 23-year longitudinal georgia stress and heart study. Hypertension 2017;69:435-42.



45. Aatola H, Koivistoinen T, Tuominen H, Juonala M, Lehtimäki T, Viikari JSA, et al. Influence of child and adult elevated blood pressure on adult arterial stiffness: the cardiovascular risk in young finns study. Hypertension 2017;70:531-6.


46. Wójcik M, Starzyk JB, Drożdż M, Drożdż D. Effects of puberty on blood pressure trajectories - underlying processes. Curr Hypertens Rep 2023;25:117-25.




47. Leyvraz M, Chatelan A, da Costa BR, Taffé P, Paradis G, Bovet P, et al. Sodium intake and blood pressure in children and adolescents: a systematic review and meta-analysis of experimental and observational studies. Int J Epidemiol 2018;47:1796-810.


48. Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure. Hypertension 2013;62:247-54.



49. Lowenstein F. Blood-pressure in relation to age and sex in the tropics and subtropics: a review of the literature and an investigation in two tribes of Brazil Indians. Lancet 1961;277:389-92.
50. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension 2020;75:285-92.



51. Couch SC, Saelens BE, Khoury PR, Dart KB, Hinn K, Mitsnefes MM, et al. Dietary approaches to stop hypertension dietary intervention improves blood pressure and vascular health in youth with elevated blood pressure. Hypertension 2021;77:241-51.



53. Di Bonito P, Pacifico L, Licenziati MR, Maffeis C, Morandi A, Manco M, et al. Elevated blood pressure, cardiometabolic risk and target organ damage in youth with overweight and obesity. Nutr Metab Cardiovasc Dis 2020;30:1840-7.


54. Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res 2005;13:163-9.



55. He Q, Ding ZY, Fong DY, Karlberg J. Blood pressure is associated with body mass index in both normal and obese children. Hypertension 2000;36:165-70.


56. Eddolls WTB, McNarry MA, Stratton G, Winn CON, Mackintosh KA. High-intensity interval training interventions in children and adolescents: a systematic review. Sports Med 2017;47:2363-74.




57. Ketelhut S, Kircher E, Ketelhut SR, Wehlan E, Ketelhut K. Effectiveness of multi-activity, high-intensity interval training in school-aged children. Int J Sports Med 2020;41:227-32.


58. Hou Y, Wang M, Yang L, Zhao M, Yan Y, Xi B. Weight status change from childhood to early adulthood and the risk of adult hypertension. J Hypertens 2019;37:1239-43.


59. Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Sleep quality and elevated blood pressure in adolescents. Circulation 2008;118:1034-40.



60. Chuang HH, Hsu JF, Wang CY, Chuang LP, Chen MC, Chen NH, et al. Hypertension in children with obstructive sleep apnea syndrome-age, weight status, and disease severity. Int J Environ Res Public Health 2021;18:9602.



61. Sarganas G, Schaffrath Rosario A, Niessner C, Woll A, Neuhauser HK. Tracking of blood pressure in children and adolescents in Germany in the context of risk factors for hypertension. Int J Hypertens 2018;2018:8429891.




62. Du T, Fernandez C, Barshop R, Fonseca V, Chen W, Bazzano LA. Variabilities in childhood cardiovascular risk factors and incident diabetes in adulthood: the bogalusa heart study. Diabetes Care 2019;42:1816-23.









 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


