< Previous Next >
Article Contents
| Korean J Pediatr > Volume 56(4); 2013 |
Abstract
Lung torsion is a very rare event that has been reported in only 9 cases in the pediatric literature but has not yet been reported in Korean infants. We present a case of lung torsion after tracheoesophageal fistula repair in an infant. Bloody secretion from the endotracheal tube and chest radiographs and computed tomographic scan results indicated lung torsion. Emergency exploration indicated 180┬░ torsion of the right upper lobe (RUL) and right middle lobe (RML). After detorsion of both lobes, some improvement in the RUL color was observed, but the color change in the RML could not be determined. Although viability of the RML could not be proven, pexy was performed for both the lobes. Despite reoperation, clinical signs and symptoms did not improve. The bronchoscopy revealed a patent airway in the RUL but not in the RML. Finally, the RML was surgically removed. The patient was discharged on the 42nd day after birth.
Lung torsion is a very rare event that has been reported in only 9 cases in the pediatric literature1-8); it has not yet been reported in Korean infants. Its etiology appeared to be threefold: secondary to trauma, spontaneous, and after thoracic surgery. We experienced a case of lung torsion following esophageal atresia with tracheoesophageal fistula (TEF) repair that required repeated detorsion and lobectomy surgeries. We describe the clinical features and methods for management with a brief review of the literature.
A 30-year-old pregnant woman was transferred to our institution at 32 weeks' gestation due to polyhydramnios. At 41 weeks of gestation, a 3.7 kg boy was delivered by misoprostol induction. After birth, the baby had mild respiratory distress and copious secretions. An attempt to pass a nasogastric tube failed, and chest radiographs showed a pouch in front of the first thoracic vertebra. The baby was diagnosed with esophageal atresia with distal TEF and underwent esophagoesophagostomy and fistula ligation on the first day of birth. The posterolateral thoracotomy using a transpleural approach was performed. The pleura dissection was carried superiorly to the apex of the chest and inferiorly for a couple of intercostal spaces. Pulmonary lobes were retracted to expose the esophagus as usual manner. During the operation, abnormal anatomic features were not found, except for esophageal atresia with distal TEF. A chest tube was placed in the thoracic cavity.
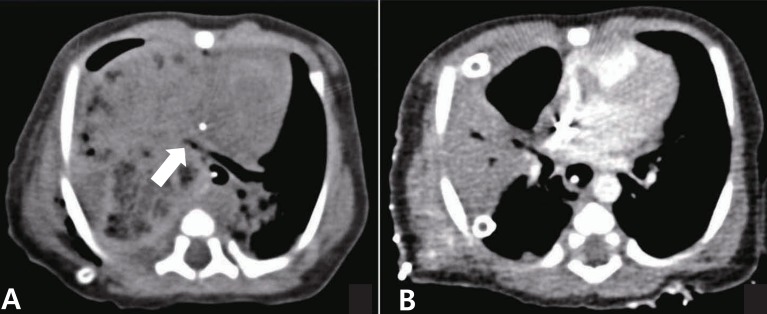
On the first postoperative day, the patient had aggravated respiratory distress with tachypnea and bloody secretions from the endotracheal tube. Chest radiographs showed opacification of the right upper lobe (RUL) (Fig. 1A). Despite repeated efforts of endotracheal suctioning and physiotherapy, serial chest radiographs on the second postoperative day revealed rapidly progressed consolidation with volume expansion of the right hemithorax (Fig. 1B). A computed tomographic (CT) scan was performed and showed abrupt narrowing of the right upper lobar bronchus and no visible right middle lobar bronchus, with extensive consolidation (Fig. 2A). Immediately, the baby underwent an emergency operation on day 3 from birth. Intraoperative findings revealed 180┬░ torsion of the RUL and right middle lobe (RML) in a clockwise direction. Both lobes appeared dark red and were engorged. After detorsion of both lobes, there was some immediate improvement in the color of the RUL, but improvement was uncertain in the RML (Fig. 3). Although viability of the RML could not be proven, pexy of both lobes was performed.
In spite of emergency rethoracotomy, respiratory distress signs and symptoms did not improve. Chest radiographs showed persistent opacification of the right hemithorax. A CT scan on the seventh day after reoperation showed consolidation in the RML (Fig. 2B). Bronchoscopy was performed and revealed a patent airway for the RUL but not for the RML. On the eighth day of second operation, the third operation was performed. Intraoperative findings revealed that the pexy of both lobes were secure, and the RUL had improved with regards to color, congestion and edema. On the other hand, RML appeared dark red and was still congested without any improvements from before. The RML was surgically removed. After the third surgery, respiratory distress signs and symptoms and radiologic examinations were improved. The baby was discharged on the 42nd day after birth. On follow-up at 6 months of age, the baby's growth and development were normal, and radiologic findings were improved, except for evidence of resection of the RML (Fig. 1C).
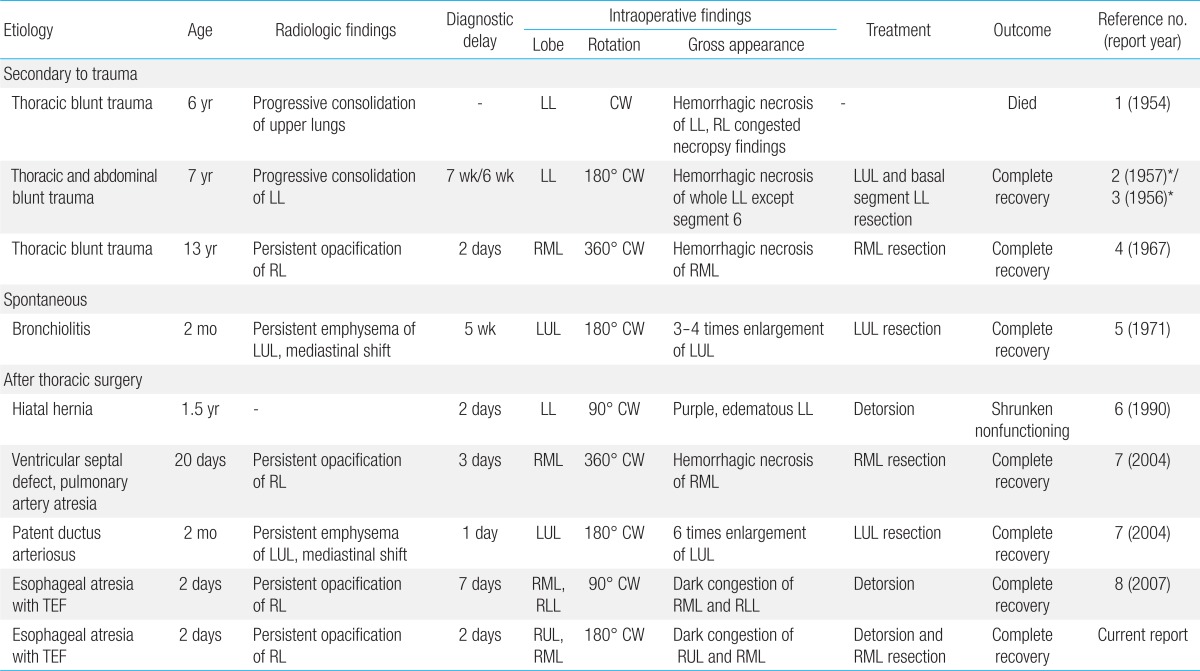
In adults, the overall incidence of lung torsion is reported to be 0.089% to 0.3% and is equally rare after thoracic surgery9,10). Its etiology appears to be threefold: secondary to trauma, after thoracic surgery, and spontaneously11). Predisposing factors of lung torsion have been known to include an airless lobe, a long and free lobar pedicle, the absence of a parenchymal bridge between contiguous lobes, pneumothorax or pleural effusion, and the transection of the inferior pulmonary ligament12). Since rotation of the bronchovascular pedicle results in airway obstruction and vascular compromise, lung torsion is a lifethreatening condition and often requires removal of the affected lobe. Adults diagnosed with lung torsion have a high mortality rate of 12-16%9). In children, lung torsion is an extremely rare event that has been reported in only 9 cases in the pediatric literature (Table 1)1-8). Lung torsion usually occurs in children who have undergone thoracic surgery or have experienced blunt trauma. One child died among the previously reported 9 cases1).
A high index of suspicion is necessary for an early diagnosis. A patient with fever, tachycardia, tachypnea, elevated white blood count, dullness to percussion and reduced breath sounds on examination, malaise, or reduced movements should raise suspicion for lung torsion2,4,9). However, there are no unique symptoms of lung torsion. The arterial blood gas analysis and oxygen saturation are usually normal, secondary to complete shunting of blood from the twisted lobe or segments13).
More specifically, radiological signs on chest radiographs may provide further confirmation of the presence of a rapidly progressing consolidated lobe, displacement of hilar structures, positional alteration of the pulmonary vasculature, bronchial cutoff or distortion, and lobar air trapping12). Chest CT and bronchoscopy are useful for diagnosing lung torsion. A chest CT scan may show the interruption of the bronchus at the level of torsion and abnormal vascular relationships in the torsive lung or lobe12). Bronchoscopy may reveal a compressed or occluded lobar bronchus that resembles a "fish-mouth"11). Contrast pulmonary angiography has the advantage of direct evidence of stenosis or complete obstruction of kinking vessels9). In our case, chest radiographs on the first postoperative day showed consolidation in the RUL. At this time, we did not suspect lung torsion but considered it to be postoperative hemothorax. The following day, chest radiographs revealed rapidly progressed consolidation. A CT scan showed abrupt narrowing of the right upper lobar bronchus and no visible right middle lobar bronchus, with extensive consolidation. Those findings made it possible to diagnose the lung torsion.
The conventional treatment of lung torsion is to remove the affected lobes, especially if the affected lobes clearly appear necrotic7,9). Resection vs. detorsion of a lobe or lung with doubtful viability is controversial12). Among the reported 9 cases, there were 6 patients who underwent resection of the affected lobes2-5,7). On the other hand, 2 patients underwent detorsion of the affected lobes6,8). Only 1 of 2 patients had salvaged lobes8). The other patient had a shrunken nonfunctioning lobe6).
In our case, the affected 2 lobes (RUL and RML) underwent detorsion. One lobe (RUL) was saved, and the other lobe (RML) was surgically removed on the eighth postoperative day. During the emergency exploration, the RML appeared to be less viable compared to the RUL. After detorsion of both lobes, there was some immediate improvement in the color of the RUL, but it was uncertain whether the color of the RML was improved. Although it is difficult to determine the tissue viability, it could be helpful to discern whether the color of affected lobes is improved after detorsion. During the third operation, we could confirm the lung tissue viability. The RUL had improved with regards to color, congestion and edema. On the other hand, RML appeared dark red and was still congested without any improvements from before. Persistent consolidation in the RML after detorsion probably reflected irreversible tissue necrosis. As the necrosis of lung parenchyma gradually progressed, parenchymal architecture might be destroyed and filled with inflammatory fluid. If consolidation of the affected lobe persists on CT scans, despite detorsion, it suggests a loss of tissue viability.
Some authors recommend resection of the affected lobe to avoid possible embolism14). Another argument against detorsion is the risk that necrotic tissue and inflammatory mediators flow into the systemic circulation and could potentially induce a systemic inflammatory response, resulting in multiorgan failure and death15). However, detorsion of the affected lobes did not result in sudden embolic events, septic condition, or death in the pediatric literature. Detorsion of the affected lobe would allow for better assessment of its potential viability. It is critical to closely evaluate the CT for evidence of perfusion, because this would favor a more conservative intraoperative approach8).
In summary, lung torsion is extremely rare in the pediatric age group. A high index of suspicion is important for an early diagnosis in children who have undergone thoracic surgery or have experienced blunt trauma. Contrast-enhanced CT scan is useful for diagnosing lung torsion. Surgical options of detorsion or resection are controversial. We suggest that detorsion is recommended if affected lobes have high viability during the exploration, as evidenced by this report.
References
1. Stratemeier EH, Barry JW. Torsion of the lung following thoracic trauma; a case report. Radiology 1954;62:726ŌĆō727.


4. Selmonosky CA, Flege JB Jr, Ehrenhaft JL. Torsion of a lobe of the lung due to blunt thoracic trauma. Ann Thorac Surg 1967;4:166ŌĆō170.


5. Hislop A, Reid L. New pathological findings in emphysema of childhood. 2. Overinflation of a normal lobe. Thorax 1971;26:190ŌĆō194.



6. Fu JJ, Chen CL, Wu JY. Lung torsion: survival of a patient whose hemorrhagic infarcted lung remained in situ after detorsion. J Thorac Cardiovasc Surg 1990;99:1112ŌĆō1114.


7. Alberti D, Borsellino A, Migliazza L, Brena ML, Sonzogni A, Cheli M, et al. Pulmonary torsion after cardiac surgery in two infants: review of pediatric literature. J Pediatr Surg 2004;39:1719ŌĆō1723.


8. Oliveira C, Zamakhshary M, Abdallah MR, Miller SF, Langer JC, Wales PW, et al. Lung torsion after tracheoesophageal fistula repair: a case report and review of literature. J Pediatr Surg 2007;42:E5ŌĆōE9.

9. Cable DG, Deschamps C, Allen MS, Miller DL, Nichols FC, Trastek VF, et al. Lobar torsion after pulmonary resection: presentation and outcome. J Thorac Cardiovasc Surg 2001;122:1091ŌĆō1093.


10. Larsson S, Lepore V, Dernevik L, Nilsson F, Selin K. Torsion of a lung lobe: diagnosis and treatment. Thorac Cardiovasc Surg 1988;36:281ŌĆō283.


11. Schamaun M. Postoperative pulmonary torsion: report of a case and survey of the literature including spontaneous and posttraumatic torsion. Thorac Cardiovasc Surg 1994;42:116ŌĆō121.


13. Kanaan S, Boswell WD, Hagen JA. Clinical and radiographic signs lead to early detection of lobar torsion and subsequent successful intervention. J Thorac Cardiovasc Surg 2006;132:720ŌĆō721.


Fig.┬Ā1
Chest radiographs showing (A) opacification of the right upper lobe on the first postoperative day; (B) rapidly progressing consolidation with volume expansion of the right hemithorax on the second postoperative day; and (C) opacification of the right lung at follow-up at 6 months of age.
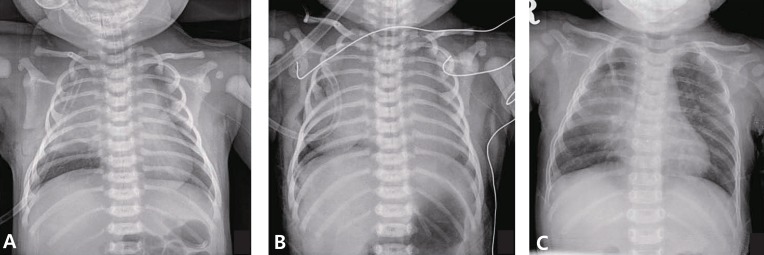
Fig.┬Ā2
Computed tomographic scans showing (A) abrupt narrowing of the right upper lobar bronchus (arrow) and no visible right middle lobar bronchus with extensive consolidation on the second postoperative day and (B) persistent consolidation of the right middle lobe on the seventh day after reoperation.




 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


