< Previous Next >
Article Contents
| Clin Exp Pediatr > Volume 57(5); 2014 |
|
Abstract
Gastrointestinal (GI) hemangiomas are relatively rare benign vascular tumors. The choice of an appropriate diagnostic method depends on patient age, anatomic location, and presenting symptoms. However, GI hemangiomas are not a common suspected cause of GI bleeding in children because of their rarity. Based on medical history, laboratory results, and imaging study findings, the patient could be treated with either medication or surgery. Herein, we report 3 cases of GI hemangioma found in the small bowel, rectum, and GI tract (multiple hemangiomas). Better knowledge and understanding of GI hemangioma could help reduce the delayed diagnosis rate and prevent inappropriate management. Although rare, GI hemangiomas should be considered in the differential diagnosis of GI bleeding.
Gastrointestinal (GI) hemangiomas are relatively rare benign vascular tumors. Although GI hemangiomas can occur anywhere along the GI tract, they most frequently occur in the small bowel, followed by the colon and rectum1). Most patients with GI hemangiomas experience GI bleeding, which may require blood transfusion, with melena and/or hematochezia. GI hemangioma is not usually a highly suspected cause of GI bleeding in children because of its rarity. Herein, we report on 3 cases of jejunal, rectal, and multiple GI hemangiomas, presenting with GI bleeding in children.
A 13-month-old boy presented with melena and nonbilious vomiting for 15 days. On arrival at our center, his heart rate was increased to 142 beats/min, but other vital signs including blood pressure and body temperature were stable. On physical examination, his abdomen was soft and flat with no pain or tenderness. The conjunctiva was mildly anemic. Laboratory findings revealed that the serum hemoglobin level, hematocrit, mean corpuscular volume (MCV), mean corpuscular hemoglobin level, and mean corpuscular hemoglobin concentration were 8.4 g/dL, 27.1%, 71.7 fL, 22.2 pg, and 31.0 g/dL, respectively. No evidence of ectopic gastric mucosa was found on 99mTc-pertechnetate scanning. The origin of the bleeding could not be traced even on the esophagogastroduodenoscopy. Abdominal ultrasonography and computed tomography (CT) showed severe segmental bowel wall thickening at the distal small bowel, suggestive of lymphoma or nonspecific ileitis (Fig. 1).
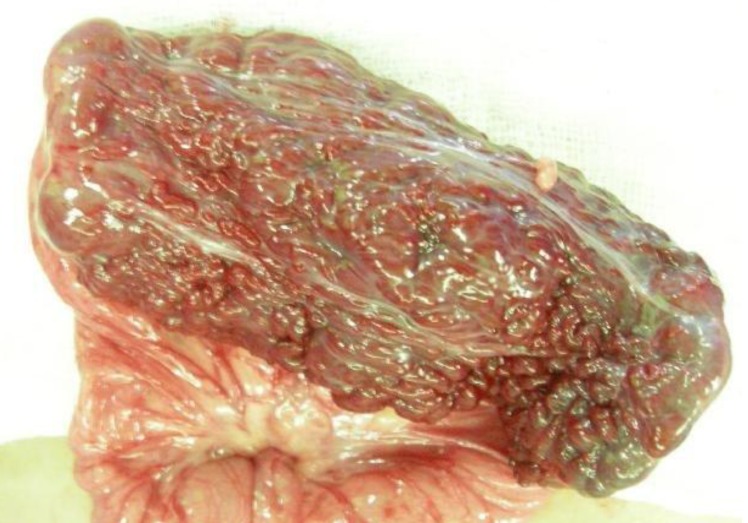
On explorative laparotomy, a 5-cm×3-cm spongy mass was detected at the jejunum (Fig. 2). Segmental resection of the jejunum, including the mass was performed. Histologic examination revealed dilatated venous malformation with calcification and thrombosis, compatible with cavernous hemangioma, involving the submucosa up to the subserosa of the jejunum (Fig. 3). The patient was discharged on the 7th postoperative day without any problems. He did not experience recurrence and had no problems in his daily life thereafter.
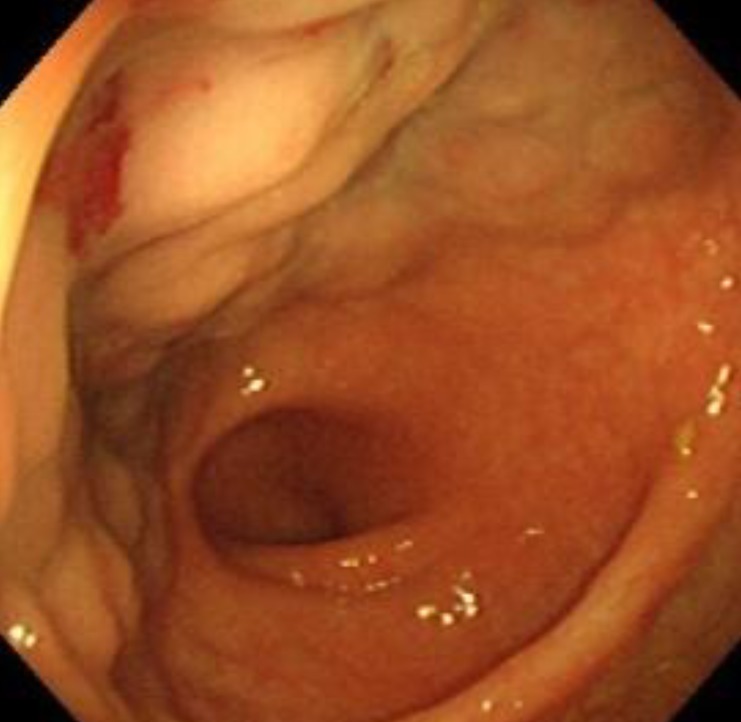
An 8-year-old boy presented with a 3-month history of hematochezia. Physical examination did not reveal any abnormalities. Laboratory findings revealed that the serum hemoglobin level, hematocrit, and MCV were 12.2 g/dL, 37.0%, and 74.9 fL, respectively. CT and colonoscopy showed a cystic loculated mass in the anterior wall of the rectum with an intraluminal and exophytic component on the left side (Fig. 4). We attempted angiography with embolization; however, angiography was not successful because there were no definite feeding arteries for the hemangioma. The patient underwent the Swenson procedure with resection of the rectal hemangioma. Pathologic examination indicated cavernous hemangioma. The patient was discharged on the 12th postoperative day without any problems. He kept fully recovered and has a good health status.
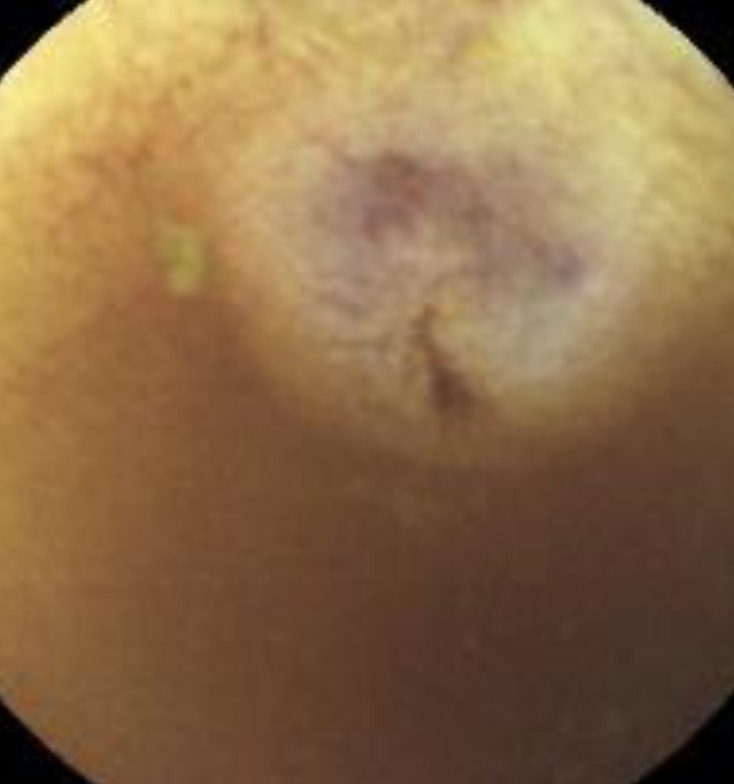
The patient was a 15-year-old girl with blue rubber bleb nevus syndrome. At the age of 7 years, she had undergone sclerotherapy to treat multiple raised, bluish-purple lesions over the trunk, limbs, and anterior chest under a suspected diagnosis of cutaneous hemangioma. At the age of 9 years, she presented with dizziness. Esophagogastroduodenoscopy revealed a gastric hemangioma, and the patient was conservatively managed. At the age of 11, she presented with melena. Capsule endoscopy showed purple vasculoectasias in the jejunum and distal ileum, raising suspicions of intestinal hemangiomas (Fig. 5). The patient underwent small bowel segmental resection and excisional biopsy with primary repair of the stomach. Surgical findings included scattered blueberry-like hemangiomas of various sizes in the stomach and small bowel (Fig. 6). Postoperative histologic examination indicated cavernous hemangioma. Four years later, the patient was readmitted for treatment of dyspnea and syncope. Capsule endoscopy was performed again, showing recurrence of multiple hemangiomas in the stomach and small bowel. The patient underwent wedge resection of the stomach and segmental resection of the small bowel. Histologic examination indicated cavernous hemangioma. No anemia or signs of intestinal bleeding were observed during the follow-up period.
Most patients with GI hemangioma present with melena and hematochezia as major complaints, both of which can be the cause of life-threatening anemia. In addition, patients may complain by various symptoms such as abdominal discomfort, abdominal pain, dizziness, nausea, vomiting, fatigue, malaise, and general weakness. GI hemangioma is most frequently found in the small bowel, and followed by the colon and rectum2). GI hemangioma may manifest as part of Maffucci syndrome, Klippel-Trénaunay syndrome, disseminated neonatal hemangiomatosis, and blue rubber bleb nevus syndrome1). GI hemangioma can be histologically classified as capillary, cavernous, and mixed types. Of these types, cavernous hemangioma is the most common. In terms of clinical manifestations, capillary hemangioma is usually solitary and tends to induce anemia by minor chronic bleeding, whereas cavernous hemangioma can result in hematemesis and melena due to acute excessive bleeding. In one of the 3 cases reported here, blue rubber bleb nevus syndrome was diagnosed, accompanied by cutaneous hemangioma and multiple GI hemangiomas. Histologically, all cases were of the cavernous type of hemangioma.
The diagnostic tools that can be used irrespective of patient age and anatomical features include imaging tests such as CT, magnetic resonance imaging, abdominal ultrasonography, scintigraphy, and angiography. Esophagogastroduodenoscopy can be used depending on anatomical features of the bleeding focus, for example, when upper GI bleeding in the stomach or duodenum is suspected. Naturally, lower GI bleeding in the colon or rectum is suspected, colonoscopy can be used. Generally, experienced pediatricians may perform esophagogastroduodenoscopy or colonoscopy without severe side effects. In addition, these procedures can be used on neonates and infants who do not have specific contraindications3). When the bleeding focus is suspected to be located in the small bowel, scintigraphy or capsule endoscopy can be performed. Scintigraphy may be useful when the bleeding focus is not detected by endoscopy or angiography. However, this method does have limitations if there is no active bleeding site or an intermittent bleeding site4). Capsule endoscopy has been reported to be useful in the diagnosis of small bowel hemangioma in young infants5). However, capsule endoscopy is not considered feasible for young infants who can barely swallow capsules and have a high risk of developing obstruction. Accordingly, the optimal diagnostic method has not yet been established for neonates and infants.
For the treatment of GI hemangioma, it is preferable that patients are observed and followed up if there are no overt symptoms or the patient has small, single lesions with mild symptoms. However, conservative treatment such as red blood cell transfusion or administration of iron supplements can be used if necessary. For medical care, corticosteroids, antiangiogenic agents, and interferon alpha can be administered. Corticosteroids have been the drug of choice for GI hemangioma for several decades. Corticosteroids are known to be suppressed the expression of vascular endothelial growth factor (VEGF)-A. interferon alpha have been reported to be an effective treatment for diffuse hemangiomatosis. Recently, enteroscopic excision was considered for cases of small hemangioma6).
Surgical intervention should be considered for the patients who do not respond to medical care. This includes patients with large lesions and comorbidities, with multiple lesions with symptoms, or with severe GI bleeding7). The surgical method is dependent on the location of the lesions. For the lesions in the stomach, wedge resection, antrectomy, subtotal gastrectomy, or total gastrectomy can be performed. For the small bowel lesions, segmental resection can be performed8). Lesions in the colon can be treated with ileocecectomy, right hemicolectomy, left hemicolectomy, or segmental resection. Finally, lesions in the rectum can be treated with low anterior resection.
In the case of blue rubber bleb nevus syndrome, a careful approach is required for selecting the appropriate surgical treatment modality because surgical outcomes may be limited and recurrence is possible9). Recent technological advances such as thermocoagulation have facilitated the management of patients with blue rubber bleb nevus syndrome. Recently, the success of pharmacologic treatment has been reported10). Corticosteroids, antiangiogenic agents, and interferon alpha can be administered for blue rubber bleb nevus syndrome. Patients with blue rubber bleb nevus syndrome have recurrent massive GI bleeding despite corticosteroids, antiangiogenic agents and interferon alpha therapy, low-dose sirolimus may be useful. Sirolimus is thought to act by blocking the VEGF-mediated pathwasys.
In conclusion, we have reported on 1 case of small bowel hemangioma, 1 case of rectal hemangioma, and 1 case of blue rubber bleb nevus syndrome. A better knowledge and understanding of GI hemangioma should help reduce the delay in diagnosis and avoid inappropriate management. Although rare, hemangioma should be considered as a differential diagnosis for cases of GI bleeding.
References
1. Magnano A, Privitera A, Calogero G, Nanfito' L, Basile G, Sanfilippo G. Solitary hemangioma of the small intestine: an unusual cause of bleeding diagnosed at capsule endoscopy. J Pediatr Surg 2005;40:e25–e27.

2. Gentry RW, Dockerty MB, Glagett OT. Vascular malformations and vascular tumors of the gastrointestinal tract. Surg Gynecol Obstet 1949;88:281–323.

3. Park JH. Role of colonoscopy in the diagnosis and treatment of pediatric lower gastrointestinal disorders. Korean J Pediatr 2010;53:824–829.



4. Howarth DM. The role of nuclear medicine in the detection of acute gastrointestinal bleeding. Semin Nucl Med 2006;36:133–146.


5. Kavin H, Berman J, Martin TL, Feldman A, Forsey-Koukol K. Successful wireless capsule endoscopy for a 2.5-year-old child: obscure gastrointestinal bleeding from mixed, juvenile, capillary hemangioma-angiomatosis of the jejunum. Pediatrics 2006;117:539–543.


6. Pohl J, Blancas JM, Cave D, Choi KY, Delvaux M, Ell C, et al. Consensus report of the 2nd International Conference on double balloon endoscopy. Endoscopy 2008;40:156–160.


7. Wang HT, Gao XH, Fu CG, Wang L, Meng RG, Liu LJ. Diagnosis and treatment of diffuse cavernous hemangioma of the rectum: report of 17 cases. World J Surg 2010;34:2477–2486.


8. Desa LA, Bridger J, Grace PA, Krausz T, Spencer J. Primary jejunoileal tumors: a review of 45 cases. World J Surg 1991;15:81–86.


Fig. 1
Abdominal computed tomography showing severe segmental bowel wall thickening at the distal small bowel loop (arrowheads).

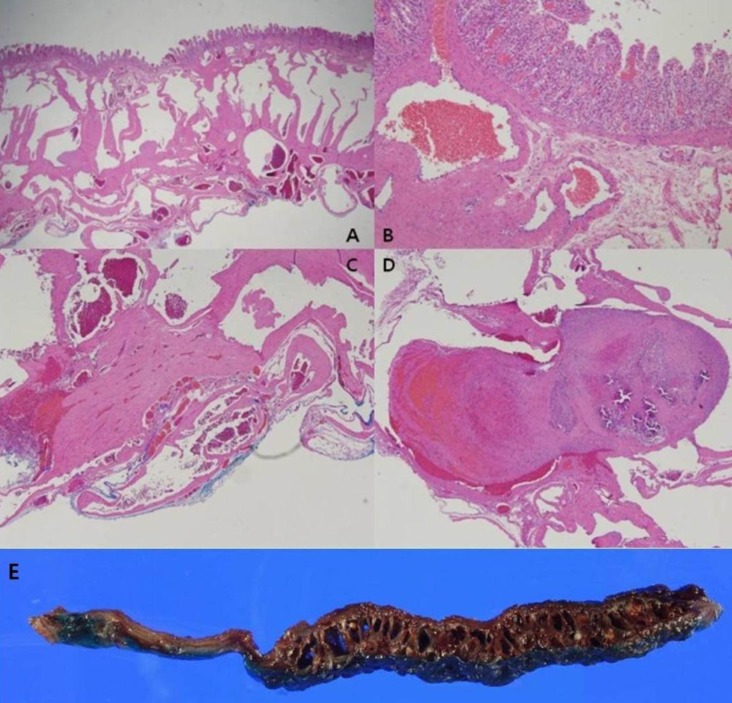
Fig. 3
Histological appearance of the hemangioma. (A) Low-power view showing a giant form arising from the large veins and forming large blood-filled sinuses (H&E, ×100); (B-D) high-power view showing dilatated venous malformation with calcification and thrombus (H&E: B, ×200; C, ×400; D, ×400); (E) surgical specimen showing a rough surface and a giant form arising from the larger submucosal vessels.




 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


