Article Contents
| Korean J Pediatr > Volume 57(8); 2014 |
|
Abstract
Purpose
The incidence of Kawasaki disease (KD) is rare in young infants (less than 3 months of age), who present with only a few symptoms that fulfill the clinical diagnostic criteria. The diagnosis for KD can therefore be delayed, leading to a high risk of cardiac complications. We examined the clinical characteristics and measured the serum levels of N-terminal pro-brain natriuretic peptide (NT-proBNP) levels of these patients for assessing its value in the early detection of KD.
Methods
We retrospectively reviewed the data of young infants diagnosed with KD from 2004 to 2012. The control group included 20 hospitalized febrile patients. Laboratory data, including NT-proBNP were obtained for each patient in both groups.
Results
Incomplete KD was observed in 21/24 patients (87.5%). The mean fever duration on admission was 1.36±1.0 days in the KD group. Common symptoms included erythema at the site of Bacille Calmette-Guerin inoculation (70.8%), skin rash (50.0%), changes of oropharyngeal mucosa (29.1%), and cervical lymphadenopathy (20.8%). The mean number of major diagnostic criteria fulfilled was 2.8±1.4. Five KD patients (20.8%) had only one symptom matching these criteria. The incidence of coronary artery complications was 12.5%. The mean serum NT-proBNP level in the acute phase, in the KD and control groups, were 4,159±3,714 pg/mL and 957±902 pg/mL, respectively, which decreased significantly in the convalescent phase.
Kawasaki disease (KD) is a multisystem vasculitis that is associated with coronary complications. Complete KD is diagnosed by a fever lasting 5 or more days and having at least four of the five following symptoms: conjunctival injection, erythematous changes of the lips and oral cavity, nonsuppurative cervical lymphadenopathy, swelling and erythema of the hands and feet and polymorphous skin rash. Incomplete KD is defined as high fever and fewer than 4 criteria which do not fulfill the diagnostic criteria of KD with or without coronary artery abnormalities1).
The highest incidence rate of KD is from 6 months to 2 years of age2). The diagnosis of infantile KD is difficult or often delayed due to vague clinical manifestations. The presentation of KD is incomplete for approximately 20 % of patients3). Moreover, in infants younger than 3 months of age, the incidence of KD is rare and only a few symptoms of clinical criteria are shown.
Many studies suggest that the serum N-terminal pro-brain natriuretic peptide (NT-proBNP) levels have become important diagnostic biomarkers of cardiovascular diseases (CVDs) in children4). The serum NT-proBNP levels have been reported as a diagnostic marker of myocardial involvement in KD4,5).
The purpose of this study was to describe clinical characteristics of KD in infants within less than 3 months of age and to evaluate the utility of serum NT-proBNP as an early diagnostic marker in young infants with incomplete KD.
We performed retrospective reviews of the medical records for 24 KD infants less than 3 months of age among all the total of 1,253 patients who were admitted to Ewha Womans University Mokdong Hospital from 2004 to 2012 and were diagnosed with KD. We included 20 febrile age matched patients who were less than 3 months of age as the febrile control group in this study.
The febrile control group less than 3 months of age consisted of patients who had a body temperature greater than 38℃ for at least 2 or 3 days. The control group was collected by screening the serum NT-proBNP level test, which is one of the test for the unknown fever.
The classical diagnostic criteria of KD by the American Heart Association were established by the existence of high fever for more than 5 days and presence of 4 or 5 features following 5 criteria: (1) changes in extremities; (2) polymorphous exanthema; (3) bilateral bulbar conjunctival injection without exudates; (4) changes in lips and oral cavity; (5) cervical lymphadenopathy (>1.5-cm diameter).
To establish the diagnosis of KD, febrile children who do not fulfill the diagnostic criteria but have several clinical characteristics compatible with those of KD were selected as patients with incomplete KD.
Laboratory tests such as complete blood count (CBC), platelet, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), total protein, albumin, NT-proBNP were compared in each group, respectively in acute phase.
All the patients with KD were treated with intravenous immunoglobulin (IVIG; 2 g/kg/day) over 10-12 hours. Laboratory tests were done at the acute period, 48-72 hours after IVIG treatment and 8 weeks afterward in patients with KD. However, the laboratory tests were performed in acute phase in the control group.
Echocardiography was performed by pediatric cardiologists to detect the presence of coronary artery lesions prior to IVIG administration. Coronary arteries were defined as abnormal if the internal lumen diameter was >3 mm in children younger than 5 years old; if the internal diameter of a segment measured ≥1.5 times that of an adjacent segment; or if the coronary lumen was clearly irregular6).
The study was carried out with the approval of the ethics committee of Ewha Womans University Mokdong Hospital Institutional Review Board and written informed consents were obtained from the parents of all the subjects.
IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used for all the statistical analysis. Clinical characteristics and laboratory data were analyzed statistically by independent t-test. A P<0.05 was considered statistically significant.
Receiver operating characteristics (ROC) curve analysis was done for the sensitivity and specificity of serum NT-proBNP level of patients with KD in acute phase.
Wilcoxon Rank Sum test and Mann-Whitney test were used to compare the serum NT-proBNP level of patients with KD and that of control. Wilcoxon signed rank test was used to compare the serum NT-proBNP level of the patients with KD in acute and subacute period.
Twenty one patients of all the 24 patients were incomplete KD. In our study, the incidence rate of the patients with KD younger than 3 months of age was 1.9% (24 of all the total of 1,253 patients with KD). The mean age of the patients with KD was 2.1 months and boys were outnumbered by girls (13:11). The mean age of the control group was 1.9 months and the male to female ratio of the control group was 11:10 (Table 1).
The mean duration of fever of the patients with KD before admission was 1.36±1.0 days. The mean duration of fever in the control group was 1.92±1.1 days. Sixty-two point five percent of the patients with KD were diagnosed as KD after 2.5±1.2 admission days. The total mean admission days to diagnosis in control group was 2.8±1.5 days. The final diagnosis of the control group includes sepsis, viral meningitis, urinary tract infection, erythema multiforme, other viral infection and bronchiolitis (Table 1).
The mean number of major diagnostic criteria was 2.8±1.4. Five patients of all the 24 patients (20.8%) had only one symptom of the diagnostic criteria (Fig. 1). The most common symptom of the diagnostic criteria was erythema at the site of BCG inoculation (70.8%), followed by skin rash (50.0%), changes of oropharyngeal mucosa (29.1%) and cervical lymphadenopathy (20.8%) (Fig. 2).
In the laboratory data, the CRP level in the KD group was significantly higher compared with the control group (7.9±5.2 mg/dL vs. 2.4±2.6 mg/dL) (Table 2).
The serum NT-pro BNP level in KD patients was significantly higher than that in the control group. The mean level of serum NT-proBNP in patients with KD in the acute phase was 4,159±3,714 pg/mL, but that in the control group was 957±902 pg/mL (P<0.05).
The area under the curve (AUC) of the serum NT-proBNP levels of patients with KD in the acute phase was 0.900 (P<0.0001). And the criterion values on the ROC curve are like this: At 1,749 pg/mL, there was a sensitivity of 84% and a specificity of 100%; at 1,488 pg/mL, there was a sensitivity of 84% and a specificity of 95%; at 1,395 pg/mL, there was a sensitivity of 84% and a specificity of 90%; at 1,300 pg/mL, there was a sensitivity of 88% and a specificity of 85%; at 1,264 pg/mL, there was a sensitivity of 88% and a specificity of 80% (Fig. 3).
The serum NT-proBNP level decreased significantly in the subacute phase of KD (232±173 pg/mL, P<0.05) (Fig. 4).
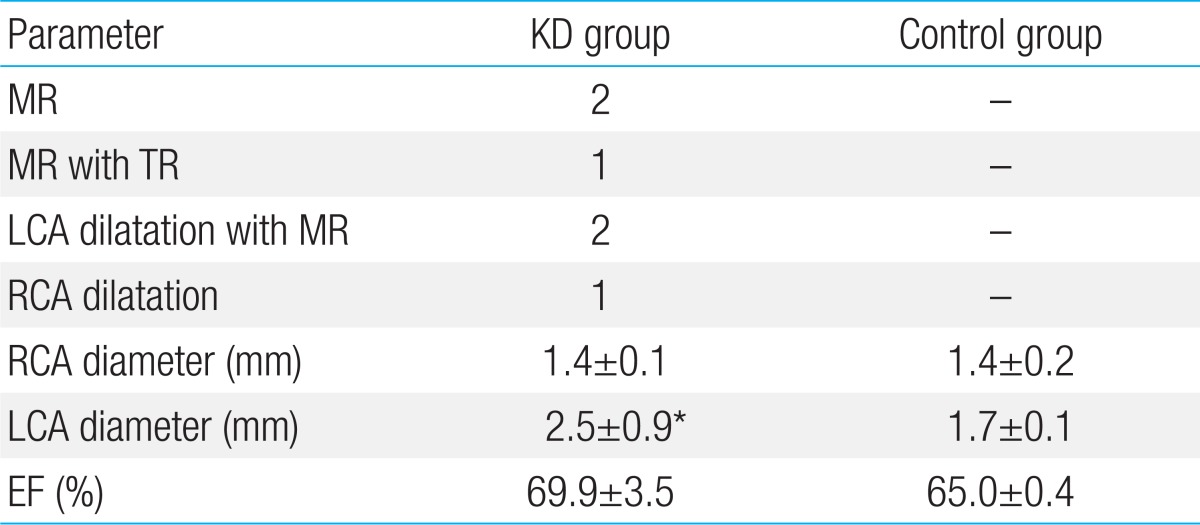
Left coronary artery (LCA) was significantly dilated in the KD group compared with the control group. There were no significant differences in ejection fraction between the two groups. The incidence of coronary artery complication in the KD group was 12.5% (Table 3).
And the abnormal echocardiographic findings of myocardial involvement including mitral regurgitation (MR) and tricuspid regurgitation (TR) were noted.
KD is diagnosed primarily in young infants usually at the age of 6 months to 2 years7). Incomplete KD should be considered in all children with unexplained fever for more than 5 days, associated with two or three of the principal clinical features of KD. Echocardiography should be considered in any infants aged 6 months with fever of 7 days, laboratory evidence of systemic inflammation and no other explanation for the febrile illness1).
The incidence rate of patients with KD younger than 3 months of age was 1.7% in Japan7) and 2.2% in Korea8). The incidence rate was similar with our data. In our study, the incidence of patients with KD was 1.9% (24/1,253).
Lee et al.8) reported that there was no significant difference in the incidence rate of coronary artery dilatation (19.9% vs. 18.7%) and coronary artery aneurysms (3.4% vs. 2.6%) between patients with KD younger than 3 months of age and the group of older than 3 months of age.
It is difficult to diagnose incomplete KD, since the diagnosis of KD depends on the clinical manifestations. KD under 3 months of age is uncommon and is more likely to be incomplete KD7). The fewer clinical manifestations in infants may result from a weak vasculitis phenomenon caused by their immature immune response, and neutralization of superantigen by maternal antibody transferred through the placenta and the cross-reaction to antibody produced by frequent active immunity9).
In this study, 21 of all the 24 patients younger than 3 months of age were incomplete KD. The mean number of major diagnostic criteria was 2.8±1.4. Five patients (20.8%) had only one symptom of the diagnostic criteria. The incidence of coronary artery complication in the KD group was 12.5%. The presence of coronary artery abnormalities may be the definite sign to diagnose the incomplete KD10). Therefore, diagnosis in the young infant group is likely to be delayed and the risk of cardiac complications can be higher than that of the older age group9). Takahashi et al.11) found a higher prevalence of coronary artery abnormalities in children younger than 3 months of age (39%) compared with that of children of 1 year age (13%). Rosenfeld et al.12) reported a higher incidence of giant coronary artery aneurysms in infants younger than 6 months of age (37%) than that in the group of the older age (5%). The most common coronary artery involvements are dilatation and aneurysm as shown in previous studies. In addition to the coronary artery involvement, the younger age group also had a higher incidence of TR and MR, which may suggest the myocardial involvement. Moreover, left ventricular myocardial dysfunction has recently been reported in KD as a complication during the acute phase of KD and demonstrated by Doppler and tissue Doppler profiles of E/E' ratio13).
No et al.14) reported that infants younger than 12 months of age had significantly higher coronary artery z scores which means coronary artery abnormalities. Moreover, they demonstrated decreased diastolic function of the left ventricle such as lower mitral inflow E/A level and a higher mitral annular E/E' level in infants than the group of older than 12 months of age.
The American Heart Association/American Academy of Pediatrics guidelines for KD recommend that IVIG treatment should be done by the tenth day of fever15). So, it is critical to predict and diagnose infantile KD with fewer clinical manifestations.
In recent studies, the serum NT-proBNP levels might be a useful marker for early diagnosis of KD in febrile infants and may be a better marker of myocardial involvement in KD. The NT-proBNP is released from the heart in response to pressure and volume overload. The NT-proBNP elevation is also associated with cytokine reactions. In the acute phase of KD, tumor necrosis factor-α and interleukin-1β are elevated, and induce secretion of NT-proBNP from the myocardium16). These cytokines are frequently associated with myocarditis and secretion of the BNP. So, the BNP elevation can be caused by inflammation or ischemia of the myocardium in the acute phase of KD17). The serum BNP and NT-proBNP level in patients with KD during the acute phase of KD were higher than those in patients with the other febrile disease4). It has been reported that the patients with incomplete diagnostic criteria for KD were less likely to exhibit elevated levels of BNP but had elevated levels of NT-proBNP4). In our study, the serum NT-proBNP level in patients with incomplete KD younger than 3 months of age in the acute phase had high sensitivity and specificity (P<0.0001) to diagnose KD. Furthermore, there was no significant relation between the number of symptom of KD and the level of NT-proBNP in this study. And the level of NT-proBNP of patients with abnormal echocardiographic findings has no significant difference compared with that of patients with normal echocardiographic finding.
There are controversies whether the serum NT-proBNP levels are stable or in decline in the period beyond the neonatal period18,19,20,21,22). A statistically significant decline is reported beyond the neonatal period. Kim et al.23) reported that there is no significant difference of the serum NT-proBNP level between children younger than 6 months of age and children 6 months to 4 years of age.
The limitation of this study is the very small number of patients younger than 3 months of age among all the KD patients and controls. And the method of selecting controls by screening the NT-proBNP test and the duration of fever also has limitations. And the control group did not have echocardiographic results and follow up laboratory test.
In conclusion, 21 of all the patients with KD younger than 3 months of age were incomplete KD patients. Serum NT-proBNP level might be a valuable biological marker for early diagnosis of the young infants with KD.
References
1. Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 2004;114:1708–1733.


3. Giannouli G, Tzoumaka-Bakoula C, Kopsidas I, Papadogeorgou P, Chrousos GP, Michos A. Epidemiology and risk factors for coronary artery abnormalities in children with complete and incomplete Kawasaki disease during a 10-year period. Pediatr Cardiol 2013;34:1476–1481.


4. Dahdah N, Siles A, Fournier A, Cousineau J, Delvin E, Saint-Cyr C, et al. Natriuretic peptide as an adjunctive diagnostic test in the acute phase of Kawasaki disease. Pediatr Cardiol 2009;30:810–817.


5. Lee H, Kim H, Kim HS, Sohn S. NT-pro BNP: a new diagnostic screening tool for Kawasaki disease. Korean J Pediatr 2006;49:539–544.

7. Yanagawa H, Nakamura Y, Yashiro M, Ojima T, Tanihara S, Oki I, et al. Results of the nationwide epidemiologic survey of Kawasaki disease in 1995 and 1996 in Japan. Pediatrics 1998;102:E65


8. Lee EJ, Park YW, Hong YM, Lee JS, Han JW. Epidemiology of Kawasaki disease in infants 3 months of age and younger. Korean J Pediatr 2012;55:202–205.



9. Chang FY, Hwang B, Chen SJ, Lee PC, Meng CC, Lu JH. Characteristics of Kawasaki disease in infants younger than six months of age. Pediatr Infect Dis J 2006;25:241–244.


10. Sonobe T, Kiyosawa N, Tsuchiya K, Aso S, Imada Y, Imai Y, et al. Prevalence of coronary artery abnormality in incomplete Kawasaki disease. Pediatr Int 2007;49:421–426.


11. Takahashi M, Mason W, Lewis AB. Regression of coronary aneurysms in patients with Kawasaki syndrome. Circulation 1987;75:387–394.


12. Rosenfeld EA, Corydon KE, Shulman ST. Kawasaki disease in infants less than one year of age. J Pediatr 1995;126:524–529.


13. Takeuchi D, Saji T, Takatsuki S, Fujiwara M. Abnormal tissue doppler images are associated with elevated plasma brain natriuretic peptide and increased oxidative stress in acute Kawasaki disease. Circ J 2007;71:357–362.


14. No SJ, Kim DO, Choi KM, Eun LY. Do predictors of incomplete Kawasaki disease exist for infants? Pediatr Cardiol 2013;34:286–290.


15. Waseem M, Pinkert H. Visual diagnosis: a febrile child who has "red eyes" and a rash. Pediatr Rev 2003;24:245–248.


16. Suzuki H, Uemura S, Tone S, Iizuka T, Koike M, Hirayama K, et al. Effects of immunoglobulin and gamma-interferon on the production of tumour necrosis factor-alpha and interleukin-1 beta by peripheral blood monocytes in the acute phase of Kawasaki disease. Eur J Pediatr 1996;155:291–296.


17. Kawamura T, Wago M, Kawaguchi H, Tahara M, Yuge M. Plasma brain natriuretic peptide concentrations in patients with Kawasaki disease. Pediatr Int 2000;42:241–248.


18. Nir A, Lindinger A, Rauh M, Bar-Oz B, Laer S, Schwachtgen L, et al. NT-pro-B-type natriuretic peptide in infants and children: reference values based on combined data from four studies. Pediatr Cardiol 2009;30:3–8.


19. Albers S, Mir TS, Haddad M, Laer S. N-Terminal pro-brain natriuretic peptide: normal ranges in the pediatric population including method comparison and interlaboratory variability. Clin Chem Lab Med 2006;44:80–85.

20. Rauh M, Koch A. Plasma N-terminal pro-B-type natriuretic peptide concentrations in a control population of infants and children. Clin Chem 2003;49:1563–1564.


21. Schwachtgen L, Herrmann M, Georg T, Schwarz P, Marx N, Lindinger A. Reference values of NT-proBNP serum concentrations in the umbilical cord blood and in healthy neonates and children. Z Kardiol 2005;94:399–404.


Fig. 1
The mean number of major diagnostic criteria fulfilled by 21 of the 24 patients enrolled in this study (87.5%), who had incomplete Kawasaki disease. The mean number of major diagnostic criteria fulfilled was 2.8±1.4. Five patients (20.8%) presented with only one symptom fulfilling the diagnostic criteria.
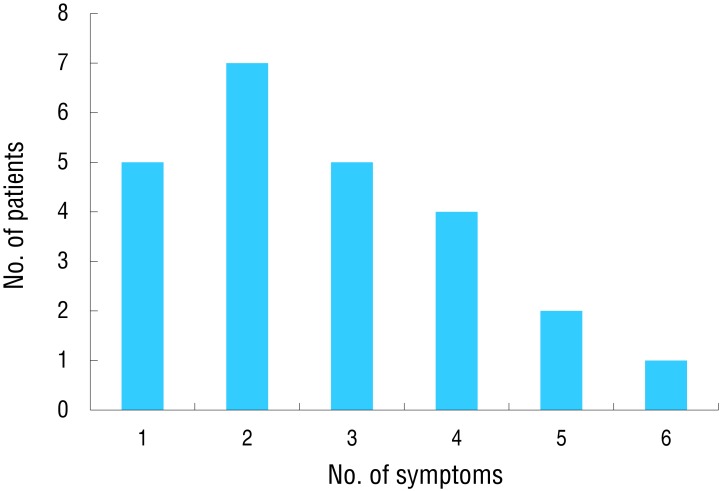
Fig. 2
Percentage of patients with specific symptoms that fulfilled the diagnostic criteria for Kawasaki disease (KD). The most common symptoms presented by KD patients were erythema at the site of Bacille Calmette-Guerin (BCG) inoculation (70.8%) and skin rash (50.0%).
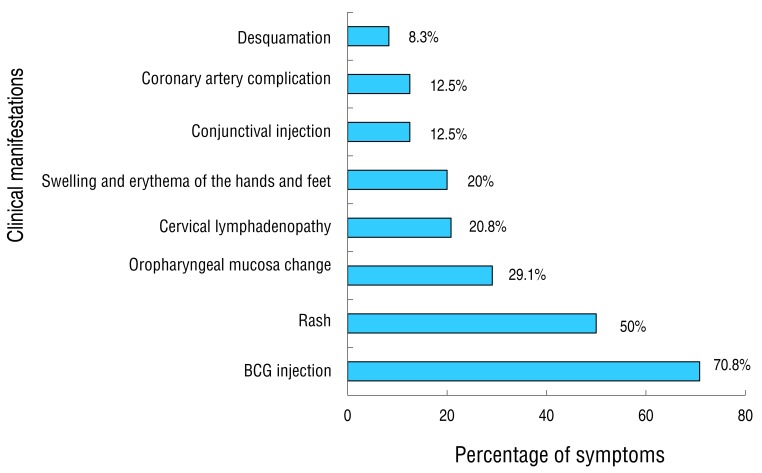
Fig. 3
Serum NT-proBNP levels measured in KD patients in the acute phase (ROC curve). A ROC curve was used to display the level of serum NT-proBNP, measured in KD patients in the acute phase. The AUC was 0.900 (P<0.0001). Level A: 1,749 pg/mL with a sensitivity of 84% and a specificity of 100%. Level B: 1,488 pg/mL with a sensitivity of 84% and a specificity of 95%. Level C: 1,395 pg/mL with a sensitivity of 84% and a specificity of 90%. Level D: 1,300 pg/mL with a sensitivity of 88% and a specificity of 85%. Level E: 1,264 pg/mL with a sensitivity of 88% and a specificity of 80%. ROC, receiver operating characteristic; AUC, area under the curve; KD, Kawasaki disease; NT-proBNP, N-terminal pro-brain natriuretic peptide.
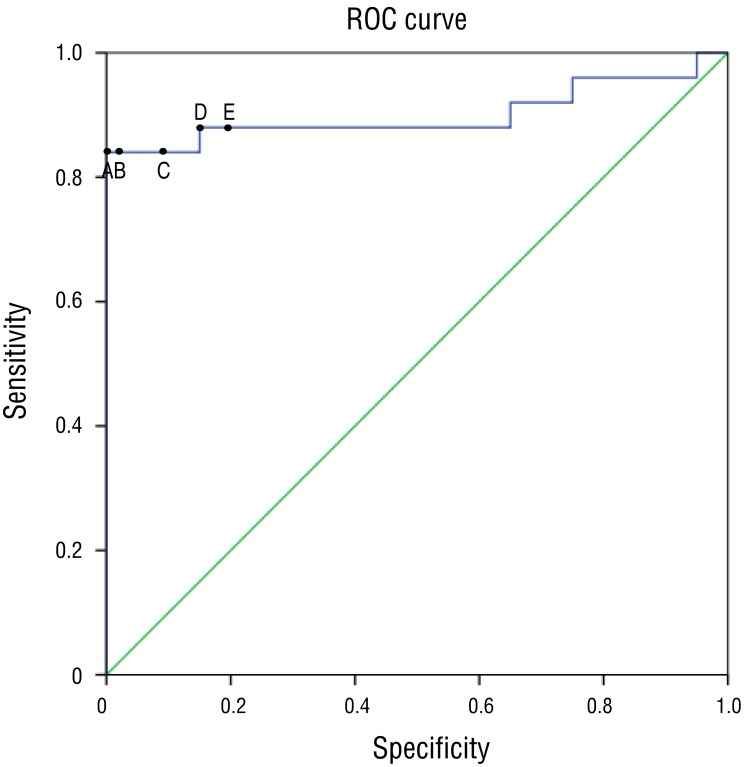
Fig. 4
Serum NT-proBNP levels in the control group, and in KD patients measured in the acute and subacute phase. Serum NT-proBNP levels in KD patients, measured in the acute phase, was 4,159±3,714 pg/mL. Serum NT-proBNP levels was 957±902 pg/mL in the control group (significantly lower, P<0.05). Serum NT-proBNP levels decreased significantly in the subacute phase of KD (232±173 pg/mL, P<0.05). KD, Kawasaki disease; NT-proBNP, N-terminal pro-brain natriuretic peptide.
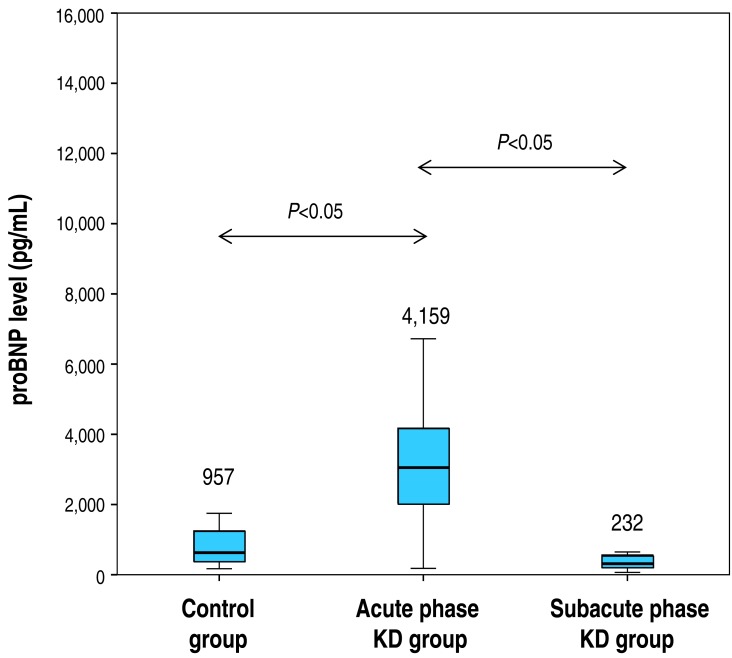
Table 1
Demographic and disease characteristic data obtained from patients with Kawasaki disease and control group patients
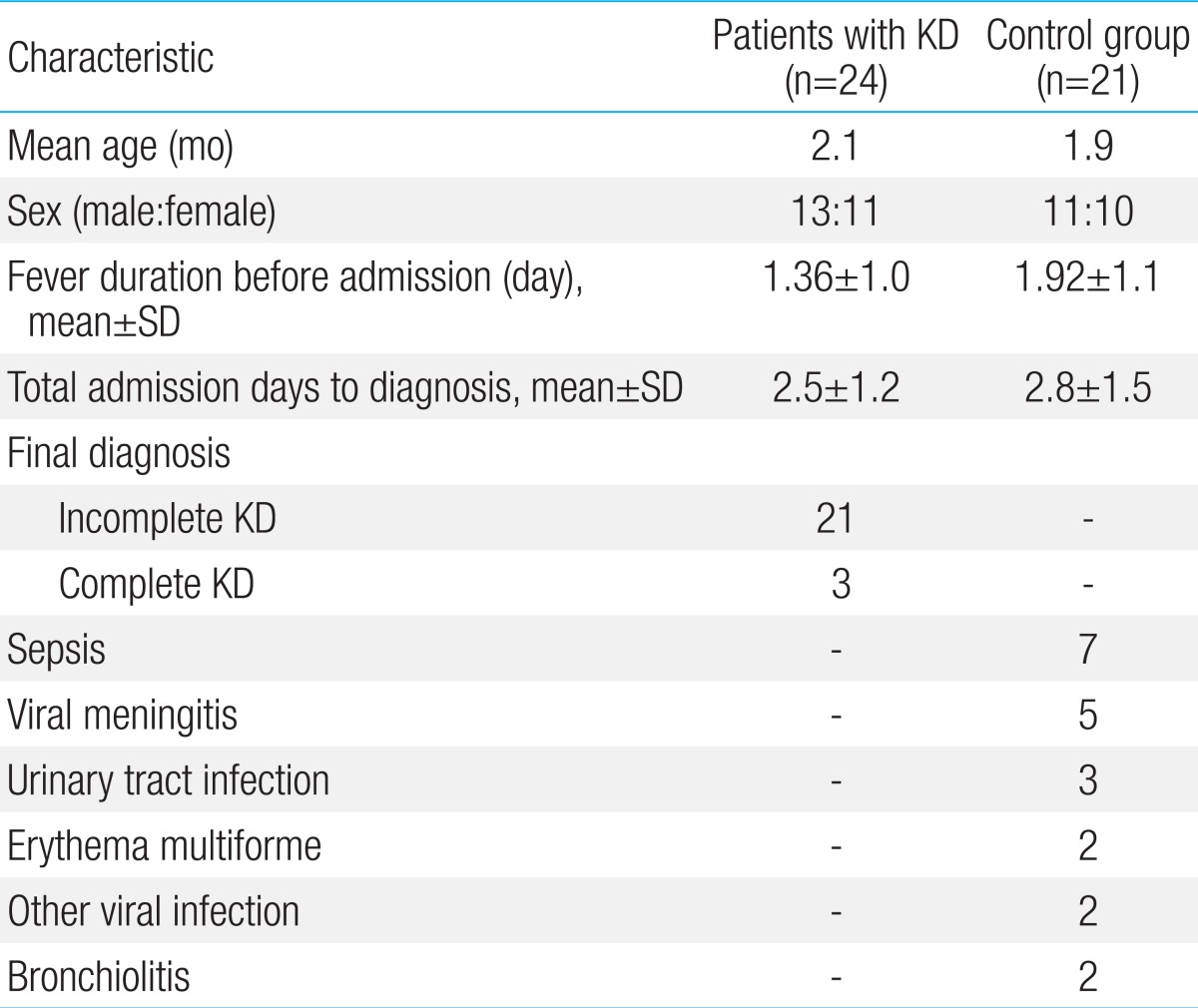
Table 2
Laboratory data obtained from patients in the Kawasaki disease and control groups

Values are presented as mean±standard deviation.
Hb, hemoglobin; Hct, hematocrit; WBC, whole blood count; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; AST, aspartate aminotransferase; ALT, alanine aminotransferase; NT-proBNP, N-terminal pro-brain natriuretic peptide
*P<0.05 significantly different from control group. †Between control and acute phase.



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


