Article Contents
| Korean J Pediatr > Volume 57(9); 2014 |
|
Abstract
Purpose
Although high morning blood pressure (BP) is known to be associated with the onset of cardiovascular events in adults, data on its effects in children with hypertension are limited. Our retrospective study aimed to define the clinical characteristics of children with morning hypertension (MH) and to determine its associated factors.
Methods
We reviewed 31 consecutive patients with hypertension, confirmed by the ambulatory blood pressure monitoring (ABPM). We divided these patients into 2 groups: the MH group (n=21, 67.7%), morning BP above the 95th percentile for age and height (2 hours on average after waking up) and the normal morning BP group (n=10, 32.3%). We compared the clinical manifestations, laboratory results, and echocardiographic findings including left ventricular hypertrophy (LVH) between the groups.
Results
The early/atrial (E/A) mitral flow velocity ratio in the MH group was significantly lower than that in the normal morning BP group. In addition, LV mass was higher in the MH group than in the normal morning BP group, although the difference was not statistically significant. The age at the time of hypertension diagnosis was significantly higher in the MH group than in the normal morning BP group (P=0.003). The incidence of hyperuricemia was significantly higher in the MH group than in the normal morning BP group.
Conclusion
Older patients and those with hyperuricemia are at higher risk for MH. The rise in BP in the morning is an important factor influencing the development of abnormal relaxation, as assessed by echocardiography. Clinical trials with longer follow-up periods and larger sample sizes are needed to clarify the clinical significance of MH.
Noninvasive techniques of ambulatory blood pressure monitoring (ABPM) make it possible to assess the blood pressure (BP) variability and to measure the early morning BP1,2). Morning hypertension (MH) defined by ABPM or home BP measurements has been reported to be associated with a significant cardiovascular event in adults3). In addition, the prognostic value as well as the baseline characteristics of adult patients with MH have been well documented. That is, the old age, male gender, a more pronounced use of diverse types of antihypertensive drugs, a more prevalent use of β-blockers and a higher clinic BP are major factors that are responsible for the difference in the BP between the morning and evening4). It has also been shown that the morning BP surge on the ABPM is associated with the old age, elevated fasting blood glucose levels and a higher 24-hour systolic BP5).
Levels of BP were higher beginning in childhood, changed adversely through adulthood, and associated with condition of prehypertension and hypertension in adulthood. However, little is known about the baseline characteristics of children and adolescents with MH. In addition, there is a paucity of evidence supporting the association of high morning BP and the target organ damage in children and adolescents with hypertension. Given the above background, we evaluated the baseline characteristics of 31 hypertensive patients for whom we performed the ABPM and then analyzed its correlation with echocardiography and laboratory findings.
We performed a retrospective pooled analysis of the data collected from Eulji University Hospital and Chungnam National University Hospital during a period ranging from March of 2006 to March from 2013. We excluded the patients with secondary hypertension, arrhythmias, a history of heart failure or coronary artery disease, renal insufficiency or chronic inflammatory diseases. The current study was approved by the Institutional Review Board of Eulji University Hospital and Chungnam National University Hospital.
The office BP was measured with the patients in a sitting position after a period of quiet for 5 minutes. The definition of casual hypertension used in this study followed the normative BP references for Korean children and adolescents6).
ABPM was performed according to the standard institutional policy and procedure using (GEMS IT Cardiosoft V4.2, Freiburg, Germany). The patients filled out a 24-hour diary to report daily activities and rest, including the sleep period. We defined the MH as the morning BP (two hours on average after waking up) above the 95th percentile for age and height. We compared the clinic BP, 24-hour systolic and diastolic BP, night dip and the heart rates between the two groups.
We recorded fasting serum laboratories including glucose, insulin and complete lipid panels. Based on commonly used gender-based cutoffs, we defined hyperuricemia as serum levels of uric acid of ≥6 mg/dL in women and ≥7 mg/dL in men7). In addition, we defined dyslipidemia as serum triglyceride of ≥110 mg/dL or high-density lipoprotein (HDL) of ≤40 mg/dL8).
Echocardiography was performed using the Vivid 7 scanner (GE Vingmed Ultrasound, Horten, Norway) and a transducer probe of 3 or 5 MHz in frequency in the initial evaluation. The echocardiographic examination was used to evaluate the valve regurgitation, quantitative cardiac contractile function and the presence of left ventricular mass index (LVMI). As described by de Simone et al.9), we used the height (m2.7) to express the LVMI. Thus, we attempted to standardize the LVM for body size. In addition, we defined the left ventricular hypertrophy (LVH) as LVMI>51 g/m2.7, as recommended by the working group. We calculated the relative wall thickness (RWT) of the LV as twice the posterior wall thickness divided by the end-diastolic LV dimension10).
All the data was expressed as median unless otherwise stated. We compared the categorical variables between the two groups using a two-tailed Fisher exact test. We used the Mann-Whitney test to analyze the continuous variables. In addition, we performed the Spearman rank correlation analysis to identify the correlation between the variables.
We performed a pooled analysis in a total of 31 patients (children and adolescents) for whom we measured the casual BP, ABPM, echocardiography and fasting laboratory values. Our clinical series of patients comprise 26 boys and 5 girls, whose mean age at diagnosis was 14.4 years (range, 10-19 years). In addition, they were followed up during a mean period of 11.8 months.
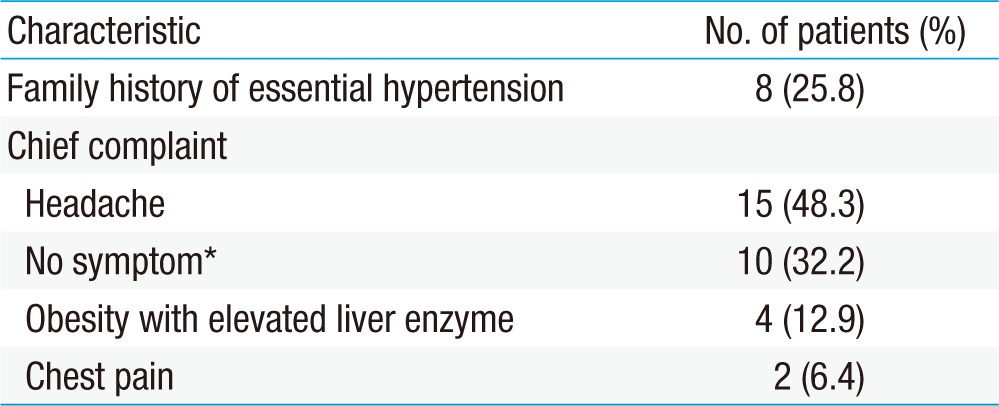
The most common chief complaint was headache in 15 patients (48.3%). This was followed by subclinical hypertension that had been detected from the regular school medical check-up, and it was seen in 10 patients (32.2%). Moreover, there were eight patients (26%) with a family history of parental hypertension for which the medication was needed (7 in MH group vs 1 in normal morning BP group) (Table 1).
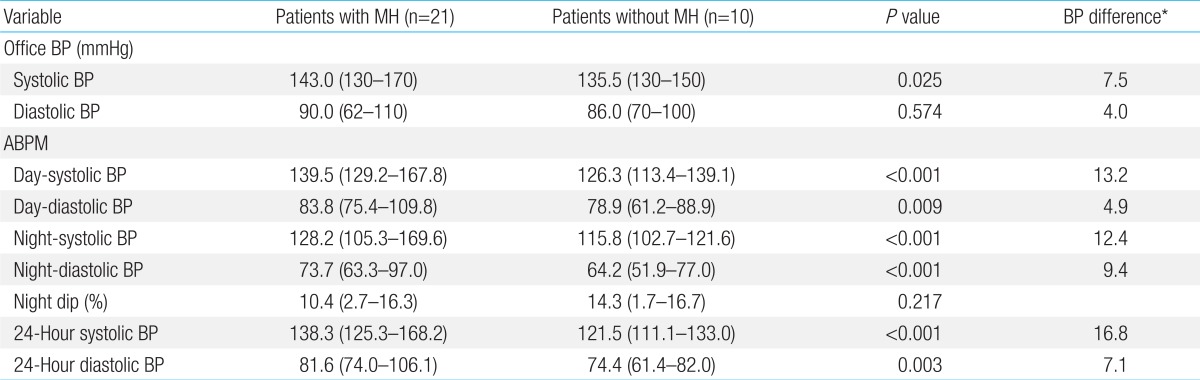
MH group had a significantly high systolic and diastolic BP in night-time compared to normal morning BP group (P<0.001). However, in casual BP, only systolic BP was significantly higher in the MH group (P=0.001). Twenty-four-hour systolic and diastolic BP was significantly higher in the MH group (P<0.001 for systolic BP, P=0.003 for diastolic BP). No statistical difference was found in night dips between the two groups (Table 2).
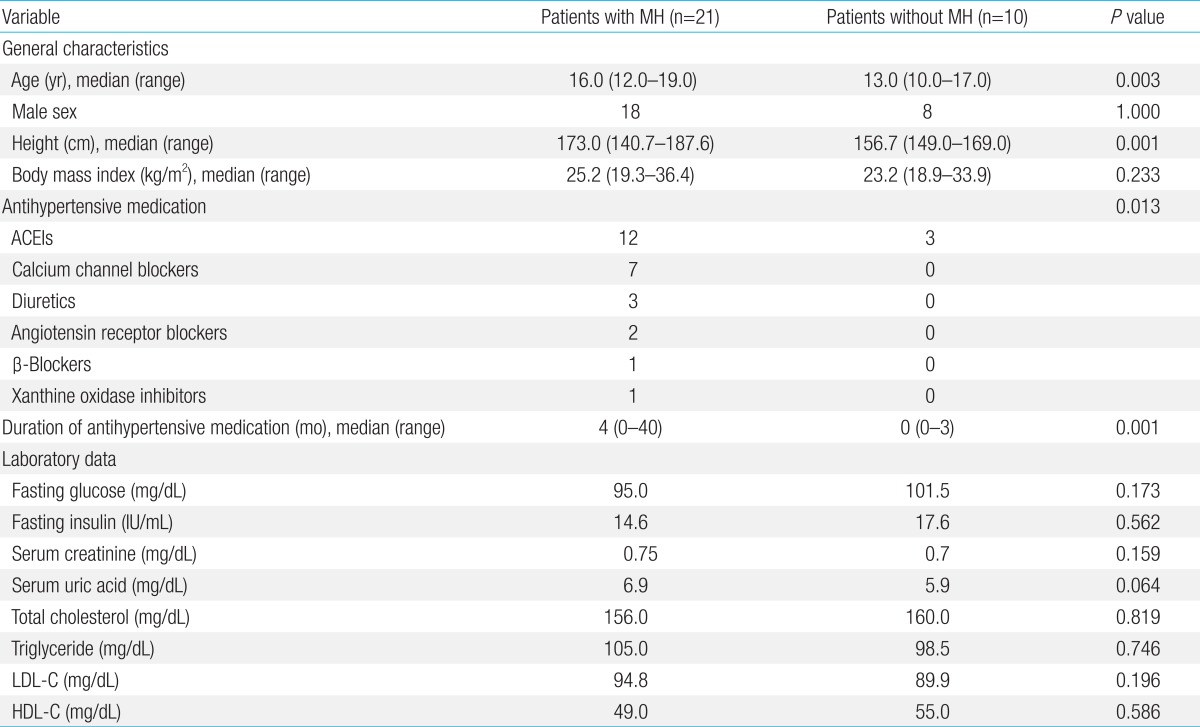
We measured the serum levels of uric acid in 28 patients; this showed that hyperuricemia was seen in 47.6% of the patients of the MH group and 20% of those of the normal morning BP group. The median serum level of uric acid was higher in the MH group (6.9 mg/dL vs. 5.9 mg/dL, P=0.064), but which did not reach a statistical significance. However, the proportion of the patients with hyperuricemia was significantly higher in the MH group as compared with the normal morning BP group (P=0.037). Blood glucose levels were measured in 100% of the patients. The median glucose level was 95 mg/dL in the MH group and 101.5 mg/dL in the normal morning BP group (P=0.173). In addition, the median insulin level was 14.6 IU/mL in the MH group and 17.6 IU/mL in the normal morning BP group (P=0.562). Serum triglyceride levels were measured in 30 patients; this showed that hypertriglyceridemia was seen in 40% of total patients. The median triglyceride level was 105 mg/dL in the MH group and 98.5 mg/dL in the normal morning BP group (P=0.746). The HDL was measured in 26 patients; this showed that there were only two patients with serum HDL levels of <40 mg/dL (Table 3).
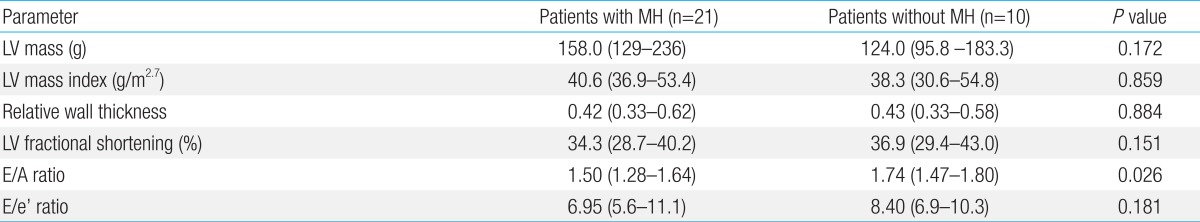
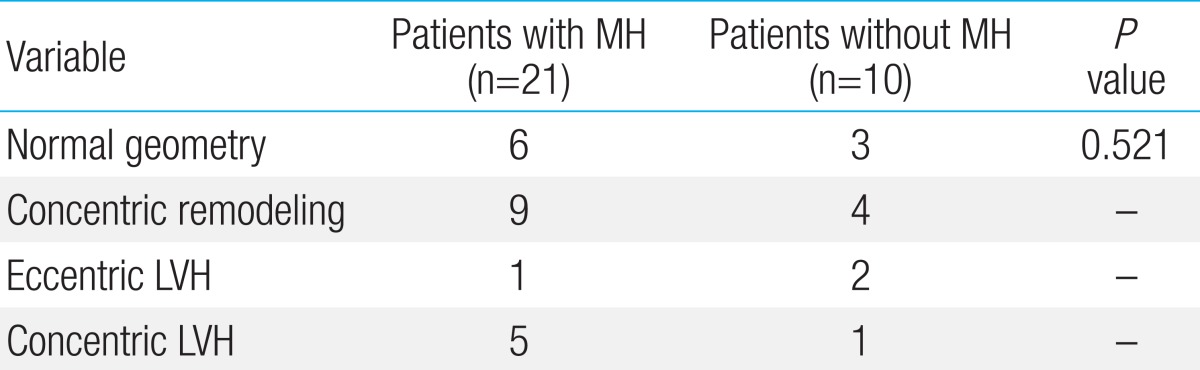
The early/atrial (E/A) mitral flow velocity ratio was significantly lower in the MH group as compared with the normal morning BP group (1.5 vs. 1.74, P=0.026). But there were no significant differences in the fractional shortening and the early transmitral flow velocity (E)/the early diastolic velocity of mitral valve annulus (e') ratio between the two groups. LVM (gm) was higher in the MH group as compared with the normal morning BP group, but which did not reach a statistical significance (P=0.172). There were no significant differences in the LVMI and RWT between the two groups (Table 4). We also compared the distribution of the LV geometric patterns between the two groups. This showed that the concentric LVH was more prevalent in the MH group (23.8%) as compared with the normal morning BP group (10%), which did not reach a statistical significance (Table 5).
The MH group were more likely to take antihypertensive medication than the normal morning BP group (P=0.013). That is, the proportion of the patients taking antihypertensive medication was 80.9% (17/21) in the MH group and 30.0% (3/10) in the normal morning BP group. With regard to the antihypertensive drug class prescribed, there were 15 patients who used angiotensin converting enzyme (ACE) inhibitors, seven who did calcium channel blockers and three on diuretics (Table 3). If BP still was not controlled, a second agent was added in 8 patients. The median duration of antihypertensive medication was 4 months in the MH group and this was statistically significant longer compared with the normal morning BP group (P=0.001).
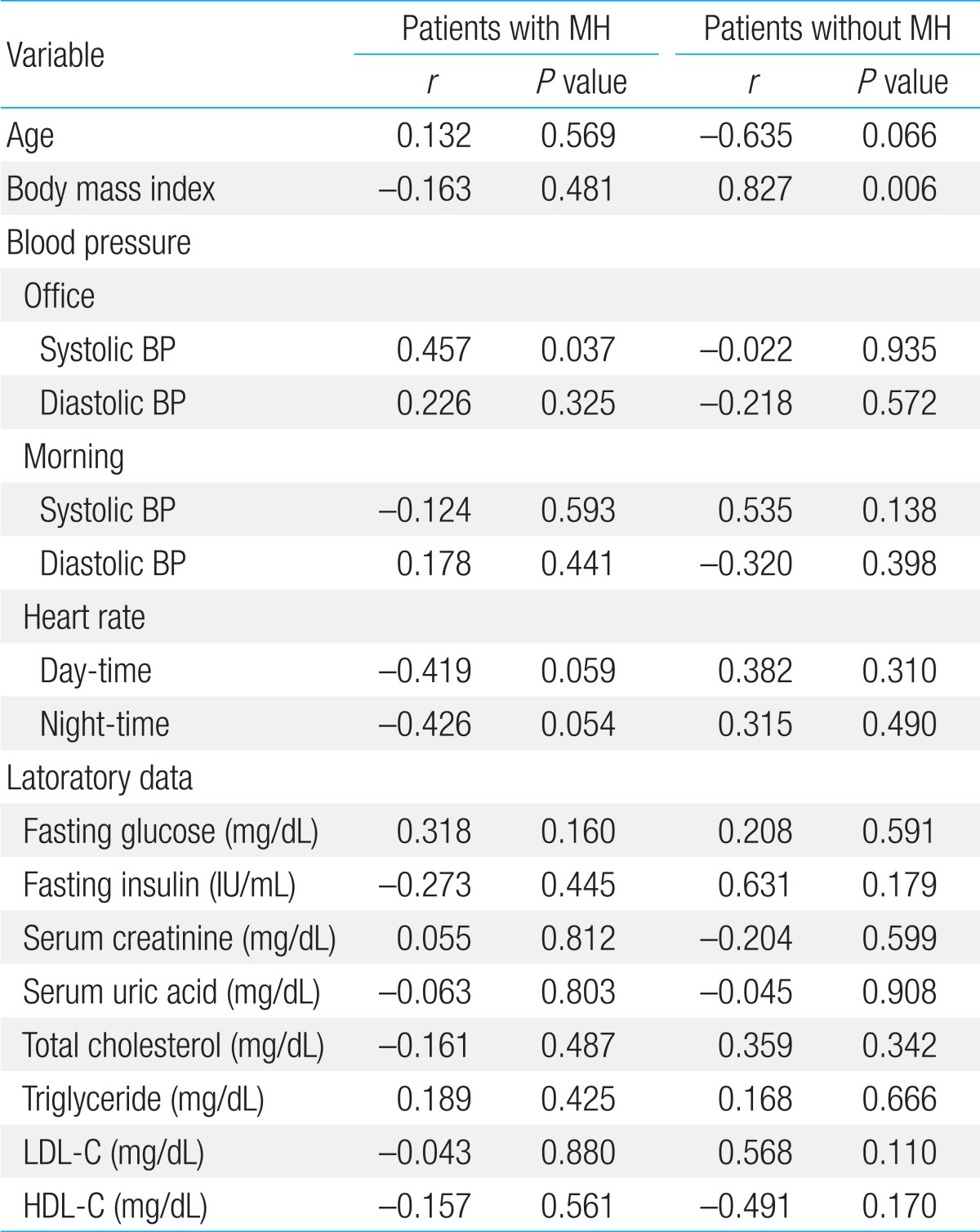
There was a significant correlation between the LVMI and the casual systolic BP in the MH group (r=0.457, P=0.037). The LVMI also had a significant correlation with the body mass index (BMI) in patients without MH (r=0.827, P=0.006). In addition, the LVMI also had a significant correlation with the age and body mass index (BMI) in patients without MH (age: r=-0.635; P=0.066; BMI: r=0.827, P=0.006). But there were no significant correlations between the LVMI and the laboratory findings in both groups (Table 6).
ABPM allows a better understanding of BP fluctuations over 24 hours than simple clinic measurements. The ambulatory BP is usually several mmHg lower than office pressure13). The ambulatory BP level is also increased during the period from night to early morning. The renin-angiotensin-aldosterone system is activated in the early morning before arousal, with increased production of renin and angiotensin II, as a result of activation of the sympathetic nervous system. In the healthy individual, this is a physiological adjustment to compensate for the change from a horizontal to a vertical position and consequent increased cardiovascular demand. It is subject to change depending on various psychological and physical stress conditions14). In normal individuals, the BP at night drops by 10%-20% when compared with mean daytime readings. A high percentage of patients with essential hypertension show "dipping" whereas all those with secondary hypertension do not15). In our study, decreased nocturnal dipping was observed in MH group compared to normal morning BP group (10.4% vs. 14.3%, P=0.217), although there was no statistical significance.
There are two types of MH: the nocturnal hypertension and the morning BP surge. The nocturnal hypertension (nondipper) is characterized by the persistent high BP from night-time to morning. The morning BP surge is associated with the extreme dipping status of nocturnal BP16). If MH is defined as a morning-evening systolic or diastolic BP difference exceeding 10 mmHg17), the nocturnal hypertension type could be missed. Therefore, we defined the MH as a condition in which the BP is above the 95th percentile for age and height in the morning (two hours on average after waking up). It has been reported that the morning rise of BP may be a predictor of hypertensive target organ damage irrespective of the actual morning BP level18,19). To date, however, few reports have described the significance of MH in children and adolescents.
In the current study, we demonstrated that the median age was significantly higher in the MH group as compared with the normal morning BP group. The median serum level of uric acid was higher in MH group, but which did not reach a statistical significance. However, the proportion of the patients with hyperuricemia was significantly higher in the MH group as compared with the normal morning BP group. Animal experimental studies have provided evidence that supports the role of serum levels of uric acid in patients with hypertension. Raising uric acid levels in rats resulted in increased BP and development of microvascular disease in the kidneys20). Elevated fasting blood glucose may be a prerequisite for hyperuricemia in susceptible children who develop abdominal fatness. In the current study, however, there was no significant correlation between hyperuricemia and elevated fasting blood glucose levels.
The LV geometry as well as the increased LVM is a key indicator for the cardiovascular risk stratification. Our results showed that the E/A ratio was an independent factor that is associated with the MH, thus suggesting that the abnormal relaxation may be an early consequence of cardiac overload due to a morning rise in BP. This is also in agreement with previous reports that the morning rise in systolic BP has a significant correlation with the E/A ratio, but does not with the LV fractional shortening21). In addition, the LV diastolic function is a significant predictor for the cardiovascular events, irrespective of the LV mass, in initially untreated hypertensive patients22).
LVH has been shown to increase the risk to hypertensive adults23). It can be easily measured in children and adolescents and has become a surrogate marker for hypertensive end-organ damage in children. However, LVH is not specific to hypertensive disease. This is because it is also associated with a number of other conditions unrelated to the BP (e.g., obesity)24). In our study, there was no significant difference of the BMI in both groups (25.2 kg/m2 vs. 23.2 kg/m2, P=0.233).
At the present, it is up to clinical practitioners to make a choice of antihypertensive treatments in children and adolescents. Pharmacologic treatments should be started for patients with stage 2 hypertension, those with stage 1 or symptomatic hypertension who had a persistent presence of LVH and those with stage 1 hypertension whose BP is unresponsive to the lifestyle change25). In our study, the number of patients with stage 2 hypertension was fourteen in the MH group and zero in the normal morning BP group. There were three patients with stage 1 and symptomatic hypertension in each group. It has been reported that β-blockers are less effective in decreasing the LVMI as compared with renin-angiotensin system inhibitors or Ca antagonists; this is also seen even after the adjustment of the differences in the BP among the treatment groups26). In the current study, ACE inhibitors were the most commonly used agents. It has been reported that both ACE inhibitors and angiotensin receptor antagonists are greatly effective in reducing the LVH27).
Hyperuricemia reduction may play a role in BP control. In the current study, there was a 17-year-old male patient who received allopurinol at a dose of 200 mg/day added on ACE inhibitors for four weeks. In this patient, the initial uric acid levels were 8.3 mg/dL and the morning BP was 142/86 mmHg. The patient showed decreased uric acid and BP level after treatment with no adverse effects of allopurinol. To date, only one clinical trial has been conducted to assess the effects of allopurinol in lowering the BP in children; it is a randomized, double-blind, placebo-controlled, crossover trial conducted in 30 adolescents with newly diagnosed primary hypertension (serum uric acid levels≥6 mg/dL) who were treated with either allopurinol 400 mg/day or placebo for 4 weeks28). The antihypertensive effects of allopurinol are based on the significant decrease in both the systemic vascular resistance and serum renin levels after the treatment.
In the current study, there was no significant difference of LVMI between the two groups. This can be explained by relatively early age of diagnosis of hypertension in our study. In contrast, the degree of LVH was higher due to high BP variability in the morning hypertensive adults29). The vascular hypertrophy induced by exaggerated and steep BP variations may thus lead to an impaired distensibility of the large arteries, resulting in the increased cardiac overload and favoring LVH30). The severity of sleep apnea is also associated with LVH. Of note, our results showed that the casual systolic BP measurements also had a predictive value for the LVH. However, casual BP measurements alone continue to be a less specific indicator for hypertensive end-organ damage; this is the case with patients with milder disease31).
Once-daily antihypertensive regimens are now widely used to treat patients with hypertension, particularly including those whose clinic BP is well-controlled. In these patients, the morning BP is frequently maintained high before the medication. Shibuya et al.32) suggested that the morning BP rise is a key factor that may affect the occurrence of LVH in hypertensive patients on antihypertensive medication.
There are two limitations of the current study as following: first, the current study was conducted under retrospective design. Therefore, we failed to determine whether the current antihypertensive treatment regimens are also effective in promoting the LVH regression. At a follow-up, seven patients underwent repeated ABPM and echocardiography; second, we enrolled a small number of patients with a male predilection. We could not determine whether our results are also applicable to different geographic populations.
In conclusion, MH is more likely to seen among patients who are older and is related to hyperuricemia. Further randomized prospective study is necessary to clarify the usefulness of antihypertensive drugs in children with morning rise of BP and LVH.
References
1. Mansoor GA, McCabe EJ, White WB. Long-term reproducibility of ambulatory blood pressure. J Hypertens 1994;12:703–708.


2. Appel LJ, Stason WB. Ambulatory blood pressure monitoring and blood pressure self-measurement in the diagnosis and management of hypertension. Ann Intern Med 1993;118:867–882.


3. Asayama K, Ohkubo T, Kikuya M, Obara T, Metoki H, Inoue R, et al. Prediction of stroke by home "morning" versus "evening" blood pressure values: the Ohasama study. Hypertension 2006;48:737–743.


4. Ishikawa J, Kario K, Hoshide S, Eguchi K, Morinari M, Kaneda R, et al. Determinants of exaggerated difference in morning and evening blood pressure measured by self-measured blood pressure monitoring in medicated hypertensive patients: Jichi Morning Hypertension Research (J-MORE) Study. Am J Hypertens 2005;18:958–965.


5. Shimizu M, Ishikawa J, Eguchi K, Hoshide S, Shimada K, Kario K. Association of an abnormal blood glucose level and morning blood pressure surge in elderly subjects with hypertension. Am J Hypertens 2009;22:611–616.


6. Lee CG, Moon JS, Choi JM, Nam CM, Lee SY, Oh K, et al. Normative blood pressure references for Korean children and adolescents. Korean J Pediatr 2008;51:33–41.

7. Fang J, Alderman MH. Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971-1992. National Health and Nutrition Examination Survey. JAMA 2000;283:2404–2410.


8. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Curr Opin Cardiol 2006;21:1–6.


9. de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 1992;20:1251–1260.


10. Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med 1991;114:345–352.


11. Mancia G, Sega R, Bravi C, De Vito G, Valagussa F, Cesana G, et al. Ambulatory blood pressure normality: results from the PAMELA study. J Hypertens 1995;13(12 Pt 1): 1377–1390.

12. Ohkubo T, Imai Y, Tsuji I, Nagai K, Ito S, Satoh H, et al. Reference values for 24-hour ambulatory blood pressure monitoring based on a prognostic criterion: the Ohasama Study. Hypertension 1998;32:255–259.


13. White WB. Relevance of blood pressure variation in the circadian onset of cardiovascular events. J Hypertens Suppl 2003;21:S9–S15.

14. Kario K, James GD, Marion R, Ahmed M, Pickering TG. The influence of work- and home-related stress on the levels and diurnal variation of ambulatory blood pressure and neurohumoral factors in employed women. Hypertens Res 2002;25:499–506.


15. Acosta AA, McNiece KL. Ambulatory blood pressure monitoring: a versatile tool for evaluating and managing hypertension in children. Pediatr Nephrol 2008;23:1399–1408.


16. Imai Y, Hozawa A, Ohkubo T, Tsuji I, Yamaguchi J, Matsubara M, et al. Predictive values of automated blood pressure measurement: what can we learn from the Japanese population - the Ohasama study. Blood Press Monit 2001;6:335–339.


17. Gosse P, Ansoborlo P, Lemetayer P, Clementy J. Left ventricular mass is better correlated with arising blood pressure than with office or occasional blood pressure. Am J Hypertens 1997;10(5 Pt 1): 505–510.


18. Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation 2003;107:1401–1406.


19. Mazzali M, Hughes J, Kim YG, Jefferson JA, Kang DH, Gordon KL, et al. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension 2001;38:1101–1106.


20. Brown DW, Giles WH, Croft JB. Left ventricular hypertrophy as a predictor of coronary heart disease mortality and the effect of hypertension. Am Heart J 2000;140:848–856.


21. Kuwajima I, Mitani K, Miyao M, Suzuki Y, Kuramoto K, Ozawa T. Cardiac implications of the morning surge in blood pressure in elderly hypertensive patients: relation to arising time. Am J Hypertens 1995;8:29–33.


22. Schillaci G, Pasqualini L, Verdecchia P, Vaudo G, Marchesi S, Porcellati C, et al. Prognostic significance of left ventricular diastolic dysfunction in essential hypertension. J Am Coll Cardiol 2002;39:2005–2011.


23. Murdison KA, Treiber FA, Mensah G, Davis H, Thompson W, Strong WB. Prediction of left ventricular mass in youth with family histories of essential hypertension. Am J Med Sci 1998;315:118–123.


24. Friberg P, Allansdotter-Johnsson A, Ambring A, Ahl R, Arheden H, Framme J, et al. Increased left ventricular mass in obese adolescents. Eur Heart J 2004;25:987–992.


25. Garin EH, Araya CE. Treatment of systemic hypertension in children and adolescents. Curr Opin Pediatr 2009;21:600–604.


26. Schmieder RE, Schlaich MP, Klingbeil AU, Martus P. Update on reversal of left ventricular hypertrophy in essential hypertension (a meta-analysis of all randomized double-blind studies until December 1996). Nephrol Dial Transplant 1998;13:564–569.


27. Klingbeil AU, Schneider M, Martus P, Messerli FH, Schmieder RE. A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension. Am J Med 2003;115:41–46.


28. Feig DI, Soletsky B, Johnson RJ. Effect of allopurinol on blood pressure of adolescents with newly diagnosed essential hypertension: a randomized trial. JAMA 2008;300:924–932.



29. Zakopoulos NA, Tsivgoulis G, Barlas G, Spengos K, Manios E, Ikonomidis I, et al. Impact of the time rate of blood pressure variation on left ventricular mass. J Hypertens 2006;24:2071–2077.


30. London GM. Role of arterial wall properties in the pathogenesis of systolic hypertension. Am J Hypertens 2005;18(1 Pt 2): 19S–22S.




 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


